This article was co-authored by Chris M. Matsko, MD and by wikiHow staff writer, Christopher M. Osborne, PhD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
There are 15 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 24,243 times.
Turner Syndrome (TS) is a relatively rare condition that affects only females and is caused by a sex chromosome abnormality. It can cause a wide range of physical and developmental challenges, but early detection and ongoing treatment allow most females with the condition to live generally healthy and independent lives. Several telltale physical signs, which can appear as early as in the womb and as late as the teenage years, often indicate TS, but only genetic analysis can diagnose the condition. Learn the signs to watch out for and you can help ensure that Turner Syndrome is diagnosed and treated promptly.[1]
Steps
Identifying Fetal and Newborn TS
-
1Conduct an ultrasound to check for prenatal indicators. Many cases of TS are detected inadvertently and while a baby is still in the womb. A typical prenatal ultrasound can often reveal several indicators of the condition, although specific testing is required for a diagnosis of TS.[2]
- Lymphoedema, a swelling of the body’s tissues, is a frequent prenatal indicator of TS and can often be picked up on an ultrasound. If it is detected, testing for TS may be warranted.[3]
- Lymphoedema on the back of the neck is a strong indicator of TS. Other common prenatal indicators include specific heart and kidney abnormalities.[4]
- Certain anomalies noted on fetal ultrasound warrant a karyotype analysis on fetal cord blood or neonate’s blood to check for TS.
-
2Identify signs of TS in early life. If not detected in the womb, many cases of TS are clearly indicated as soon as a female child is born. When these physical indicators are present at birth or during early life, genetic testing to confirm or rule out TS should be done.[5]
- If not detected in the womb, lymphoedema or heart or kidney abnormalities after birth are possible signs of TS.[6]
- Additionally, newborns with TS may have one or more of the following: wide or web-like necks; small lower jaws; broad chests ("shield chests") with widely-spaced nipples; short fingers and toes; upward turned fingernails; below-average height and growth rate; and other possible signs.[7]
Advertisement -
3Diagnose TS via karyotype testing. Karyotype testing is a chromosomal analysis that will detect the abnormality that causes TS. For newborn girls onward, a simple blood draw is all that is required to begin the testing process. Karyotype testing is very accurate in diagnosing TS.[8]
- For fetuses still in the womb, an ultrasound that indicates possible TS will usually be followed by testing of the mother’s blood, which contains traces of fetal DNA. If this also indicates TS, testing of a sample of the placenta or of the amniotic fluid can confirm the condition.
Diagnosing TS in Teens and Young Adults
-
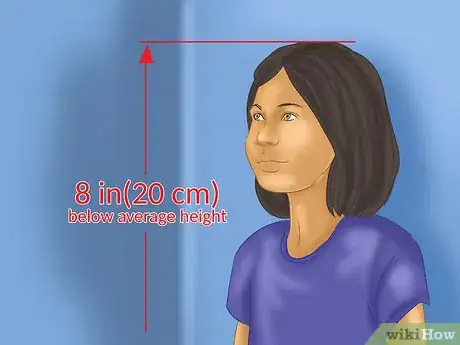
1Watch for a growth rate that is well below average. In a small number of cases, signs of TS do not become apparent until a girl reaches her teens or even early adulthood. A female that is consistently well below average height or seems to never experience a "growth spurt" may benefit from testing for TS.[9]
- Generally speaking, if a teen girl is 8 inches (20 cm) or more below average height, testing for TS may be warranted.
-
2Take notice if signs of puberty's onset are missing. Most females with TS have ovarian failure that causes infertility and prevents the onset of puberty. This failure can occur early in life or progressively over time, making it possible that it will not become apparent until the teen years.[10]
- If there is little indication of the start of puberty — body hair growth, breast development, menstruation, sexual maturation, etc. — in a girl who is well into her teens, TS should be considered a strong possibility.[11]
-
3Look for specific learning and social difficulties. TS can also impact the mental and emotional development of some females, and these effects may not be as noticeable during early childhood. If, however, as a teen or young adult, a girl has social difficulties due to an inability to "read" others' emotions and responses, TS should be considered.[12]
- Additionally, teen girls with TS may have a particular learning disability in regards to spatial concepts. This, for instance, may become more apparent as mathematics classes become increasingly advanced. This doesn't mean that any girl having trouble in math class has TS, of course, but it may be worth consideration when other factors are present.
-
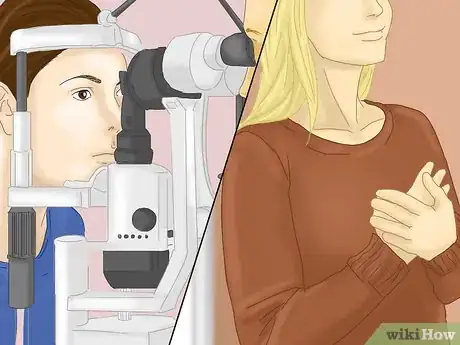
4See a doctor to confirm your suspicions. Just because a girl is especially short, has kidney problems, has a low hairline on the neck, or has not started puberty by the typical age range does not mean she has TS. Visual cues and common symptoms can only indicate TS; a medical diagnosis via genetic testing is the only way to confirm the condition.[13]
- Karyotype genetic testing to accurately diagnose TS requires only a blood draw and a wait of a week or two for the lab results. It is simple and highly accurate.
- Most cases of TS are detected and diagnosed before or shortly after birth, but if you suspect an undiagnosed case, seek a medical opinion promptly. The sooner the condition is confirmed (if present), the sooner important treatments can begin. A timely use of growth hormones, for instance, can make a significant difference in the final height of a female with TS.
Understanding and Dealing with TS
-
1Recognize that TS is a random occurrence. TS is caused by a missing, partly missing, or abnormal “X” chromosome in a female. All indications are that this is a random developmental occurrence, and that family history plays no role. This means, for instance, that you are no more likely to have a second child with TS if you already have one with the condition.[14]
- A male gets an X chromosome from his mother and a Y chromosome from his father; A female gets two X’s, one from each parent. Females with TS, however, are either missing one of the X’s (monosomy); have one X that is damaged or partly missing (mosaicism); or have traces of Y chromosomal material mixed in.
- TS occurs in about 1 in 2,500 female births worldwide. This ratio, however, is much higher among miscarried and stillborn females, of which TS can play a significant role. Testing improvements also mean that an indeterminate (but likely higher) ratio of fetuses with TS are aborted.[15]
-
2Prepare for a range of possible medical and developmental challenges. Beyond the typical impacts on physical growth and reproductive development, the possible effects of TS are wide-ranging and can vary greatly from person to person. The precise nature of the X chromosome abnormality and a host of other factors play into determining just how TS will affect a female. Expect, however, to face numerous challenges.[16]
- Complications arising from TS can include, but are by no means limited to: heart and kidney defects; increased risks for diabetes and high blood pressure; hearing loss; vision, dental, and skeletal problems; immune disorders such as an underactive thyroid; infertility (in nearly all cases) or significant pregnancy complications; and psychological conditions such as ADHD.[17]
-
3Conduct regular testing for common health impacts. Females with TS are 30% more likely to have congenital heart defects, and 30% more likely to have kidney abnormalities. All females diagnosed with TS, therefore, should undergo a cardiac evaluation and renal ultrasound, and continue to have regular checkups with specialists in these areas.[18]
- A female with TS should also undergo regular blood pressure, thyroid, and hearing tests, among other tests and examinations recommended by her medical team.
- Managing TS requires regular and ongoing medical care from a team of medical specialists from a variety of fields, which can be a daunting prospect; however, in most cases, this team-oriented approach will permit females with TS to live largely independent and healthy lives.[19]
-
4Live your life with TS. A Turner Syndrome diagnosis, whether it occurs before birth or during early adulthood, is far from a death sentence. Females with TS are every bit as capable of living long, active, fulfilling lives as anyone else. Proper diagnosis and treatment are essential for making this possibility a reality, though.[20]
- Treatments for TS usually include growth hormone therapy, to increase final height; estrogen therapy, to spur physical and sexual development as associated with puberty; and symptom treatments (such as for a heart or kidney condition).[21]
- Fertility treatments can in some cases enable women with TS to bear children, but most women with the condition remain infertile. A normal, active sex life is almost always possible regardless of fertility status.
References
- ↑ https://my.clevelandclinic.org/health/diseases/15200-turner-syndrome
- ↑ https://rarediseases.org/rare-diseases/turner-syndrome/
- ↑ http://www.nhs.uk/Conditions/Turners-syndrome/Pages/Diagnosis.aspx
- ↑ https://rarediseases.org/rare-diseases/turner-syndrome/
- ↑ https://rarediseases.info.nih.gov/diseases/7831/turner-syndrome
- ↑ http://www.nhs.uk/Conditions/Turners-syndrome/Pages/Diagnosis.aspx
- ↑ https://my.clevelandclinic.org/health/diseases/15200-turner-syndrome
- ↑ https://kidshealth.org/en/parents/turner.html
- ↑ https://www.nichd.nih.gov/health/topics/turner/conditioninfo/symptoms
- ↑ https://kidshealth.org/en/teens/turner.html
- ↑ http://www.nhs.uk/Conditions/Turners-syndrome/Pages/Diagnosis.aspx
- ↑ https://kidshealth.org/en/teens/turner.html
- ↑ https://www.nichd.nih.gov/health/topics/turner/conditioninfo/diagnosed
- ↑ https://www.nichd.nih.gov/health/topics/turner/conditioninfo/causes
- ↑ https://www.genome.gov/19519119/learning-about-turner-syndrome/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2600710/
- ↑ https://rarediseases.org/rare-diseases/turner-syndrome/
- ↑ https://www.aafp.org/afp/2007/0801/p405.html
- ↑ https://www.uptodate.com/contents/management-of-turner-syndrome-in-adults
- ↑ https://turnersyndromefoundation.org/living/
- ↑ https://www.nichd.nih.gov/health/topics/turner/conditioninfo/treatment


























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...