This article was medically reviewed by Meera Subash, MD. Dr. Meera Subash is a board certified Rheumatologist and Internist. She specializes in scaling up healthcare technology solutions for rheumatic and chronic disease management. Dr. Subash holds a BA in Human Biology from Stanford University and a Doctor of Medicine (MD) from Texas Tech University Health Sciences Center. She completed a residency in Internal Medicine at The University of California, San Diego, where she served as Chief Resident in Quality and Patient Safety at The VA San Diego Healthcare System. Dr. Subash also completed a fellowship in Rheumatology at The University of California, San Francisco - School of Medicine. She is currently pursuing another fellowship in Clinical Informatics at The University of California, San Francisco - School of Medicine.
There are 23 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 13,015 times.
Vasculitis is a disease that results when your body mistakenly attacks its own blood vessel walls, causing inflammation.[1] Rather than a disease itself, it is generally a symptom of another condition, such as giant cell arteritis, hypersensitivity vasculitis, polyarteritis nodosa, or Kawasaki disease.[2] [3] However, the diagnostic process is similar for these diseases, so watch for symptoms and then make an appointment to see your doctor.
Steps
Watching for Symptoms
-
1Pay attention to fevers. This condition often causes a fever, which is technically anything above the normal body temperature of 98.6 °F (37.0 °C). If you feel warm and are alternating between sweats and chills, you should check your temperature with a thermometer.[4]
- Call your doctor or visit urgent care if your temperature is over 103 °F (39 °C).[5]
-
2Notice headaches and other pains. This condition can lead to pain in various areas across your body, including commonly in the abdomen as well as any joints. You may also experience headaches as a result of this condition.[6] Specifically, you may experience joint pain, but it depends on the type of vasculitis you have.[7]
- You may just feel a general achiness across your body, or you may feel a specific ache in a specific muscle.
Advertisement -
3Look for loss of appetite and weight loss. You may not feel like eating as much if you have this condition, which can result in weight loss. Check the scale yourself to see if weight has come off, or take note if your clothes suddenly start feeling looser without you trying to thin down.[8]
- This symptom can indicate a number of conditions, but you should visit the doctor anyway if you notice you're losing weight without wanting to.
-
4Watch for tiredness and fatigue over days or weeks. Of course, everyone gets a little sleepy or worn down now and then. However, if you have a more pervasive fatigue that sticks around for weeks, making you feel worn out, you should talk to your doctor.[9]
- For instance, maybe you feel like you've just been dragging your feet around for weeks, like you don't have any energy at all.
-
5Check for purple blood spots, lumps, and ulcers on your skin. With this condition, you may develop distinctive reddish-purple spots called "purpura," which are small pools of blood created by blood vessels bursting under the skin.[10] You may also notice lumps under your skin or ulcers in your mouth. While not every person with vasculitis develops a rash, it can be an indication of the condition.[11]
- Purpura can be small, purple pinpricks or large patches. While "burst blood vessels" may sound disconcerting, the spots themselves usually aren't harmful.
- Mouth ulcers are small sore spots that usually appear on your gums or cheeks.[12]
- Blood spots may also appear in your urine.
-
6Visit urgent care or the emergency room for shortness of breath. Your lungs may be affected, causing you to feel like you can't take a deep breath. You might also develop a cough. You may even show pneumonia-like signs when the doctor takes an x-ray, even though it may not actually be pneumonia.[13]
-
7Notice tingling and numbness across your body. If your nerves are affected, you may experience tingling like your limbs are waking up from being asleep, or other abnormal sensations. You might also have some numbness or impeded ability to control your movements, which can be a little scary. The numbness just means your nerves are being affected by the underlying vasculitis.[16]
- In addition, you may feel shooting pains in your limbs.
Visiting the Doctor
-
1Make an appointment if you are experiencing symptoms. Vasculitis is difficult to diagnose, as the symptoms are common to other diseases as well. However, if you are experiencing a combination of these symptoms, you should still visit your doctor for a diagnosis, even if tests reveal it's not vasculitis.[17]
- Bring a list of your symptoms with you. Note when you experience them and how often. That way, you have the list on hand when your doctor asks about symptoms, and you won't forget anything.
-
2Expect a physical examination. Your doctor will start by performing a physical examination, including a blood pressure test. This test is important in the diagnosis of vasculitis, as high blood pressure can indicate you have a type of this condition that is affecting your kidneys.[18]
-
3Be ready to give a urine sample. Both a urine test and a serum creatinine test are critical in diagnosing vasculitis. You will need to pee in a cup for this test and then give the sample to the doctor. It helps to not go to the bathroom before you go to your doctor's office, so you have enough urine for the sample.[19]
- The doctor will be looking for unusual levels of blood cells and/or protein in your urine.
-
4Expect to give blood while at the doctor's office. The doctor will also want to run blood tests, so you will need to have blood drawn while you're there. The doctor will run full counts and look for signs of inflammation in your blood.[20]
- Typically, the doctor will be checking if you have enough red blood cells, as well as look for certain antibodies that indicate different types of vasculitis. Your doctor may also run a blood culture, check kidney function, screen for drug use, and look for conditions like Lyme disease and hepatitis.
Using Imaging Tests and Other Diagnostics
-
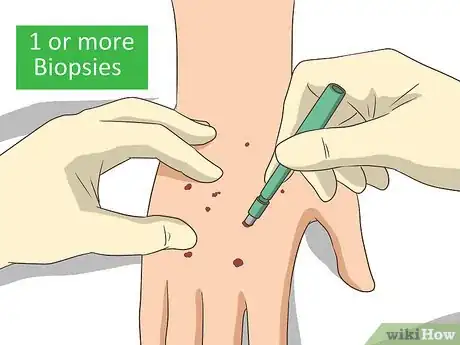
1Expect one or more biopsies. The most common and precise way to diagnose this condition with certainty is through a biopsy. A biopsy is when the doctor takes a small tissue sample from your skin or other organs, and then they test the skin sample in a lab. They will request a specific kind of biopsy based on the type of vasculitis they think you have.[21]
- A skin biopsy is a relatively simple outpatient procedure. The doctor will give you local anesthesia and apply a couple of stitches when done.
- Other biopsies, such as kidney, sural nerve, and temporal artery, are still done under local anesthesia, but they may require a short hospital stay.
- The most complicated biopsies are the lungs and brain, which will almost definitely involve a hospital stay if you need them done. Your doctor will only order a biopsy of these organs if they think you have a type of vasculitis that warrants it. They may also use these biopsies to rule out other diseases.
-
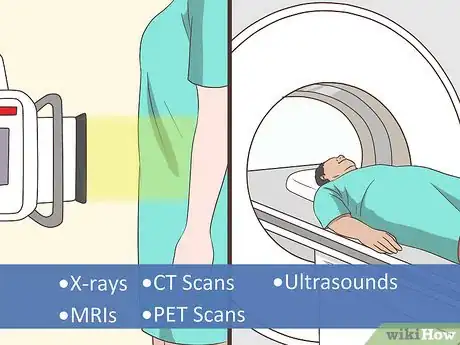
2Be ready for x-rays, MRIs, CT scans, PET scans, and/or ultrasounds. These imaging tools, which look at different parts of your body, can help your doctor narrow down your condition. Typically, they'll use these different types of scans to determine which of your internal organs are affected.[22]
- Common imaging tests for this condition include an abdominal ultrasound, chest x-ray, and a full-body MRI or CAT scan.[23]
- Generally, these tests are external, meaning they don't require anesthesia or incisions.
-
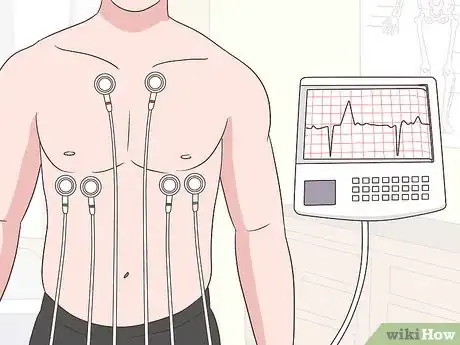
3Discuss whether an echocardiogram (ECG) is necessary. This test shows the doctor a moving image of your heart. They use it to make sure your heart is the size and shape it should be and to ensure it's pumping properly.[24]
- Doctors perform echocardiograms in different ways, depending on the technology they're using, such as Doppler or ultrasound.
- Typically, these procedures are non-invasive, though you may need a transesophageal echocardiogram. In that case, a flexible tube will be fed down your throat so that doctors can get a more direct image of your heart.[25]
-
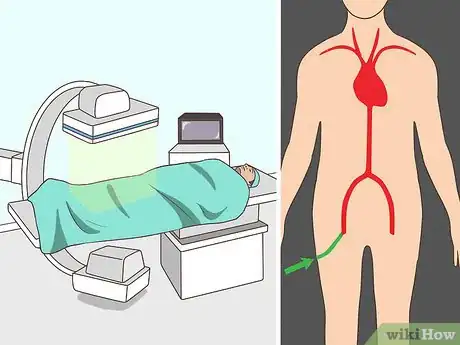
4Anticipate a blood vessel x-ray, also known as an angiography. With an angiography, the doctor or technician will first insert a catheter into an artery in your leg. Once it's in, they will inject your blood vessel with a dye that will be carried throughout your blood vessels, which they will then x-ray.[26]
- This process gives the doctor a complete picture of your blood vessels. Typically, they are looking for aneurysms, where a small part of your blood vessel pouches out a little. The presence of aneurysms can indicate Polyarteritis Nodosa, a type of vasculitis.
-
5Prepare for nerve conduction studies. In addition to other testing, your doctor may perform nerve conduction studies if neuropathy is present.[27] These measure how fast electrical impulses travel through the nerves. Such studies are generally done on an outpatient basis.
Expert Q&A
-
QuestionIs vasculitis always caused by an autoimmune condition?
 Meera Subash, MDDr. Meera Subash is a board certified Rheumatologist and Internist. She specializes in scaling up healthcare technology solutions for rheumatic and chronic disease management. Dr. Subash holds a BA in Human Biology from Stanford University and a Doctor of Medicine (MD) from Texas Tech University Health Sciences Center. She completed a residency in Internal Medicine at The University of California, San Diego, where she served as Chief Resident in Quality and Patient Safety at The VA San Diego Healthcare System. Dr. Subash also completed a fellowship in Rheumatology at The University of California, San Francisco - School of Medicine. She is currently pursuing another fellowship in Clinical Informatics at The University of California, San Francisco - School of Medicine.
Meera Subash, MDDr. Meera Subash is a board certified Rheumatologist and Internist. She specializes in scaling up healthcare technology solutions for rheumatic and chronic disease management. Dr. Subash holds a BA in Human Biology from Stanford University and a Doctor of Medicine (MD) from Texas Tech University Health Sciences Center. She completed a residency in Internal Medicine at The University of California, San Diego, where she served as Chief Resident in Quality and Patient Safety at The VA San Diego Healthcare System. Dr. Subash also completed a fellowship in Rheumatology at The University of California, San Francisco - School of Medicine. She is currently pursuing another fellowship in Clinical Informatics at The University of California, San Francisco - School of Medicine.
Board Certified Rheumatologist Sometimes vasculitis is not actually related to an autoimmune condition. Sometimes it can be related to a drug-induced state. Levamisole-induced vasculitis has been reported in patients who use cocaine. PTU, an older thyroid medication, and several other medications have been associated with the development of vasculitis. Vasculitis can also present as a paraneoplastic phenomenon, meaning that it's associated with either a known or an occult cancer or as a result of an underlying infection.
Sometimes vasculitis is not actually related to an autoimmune condition. Sometimes it can be related to a drug-induced state. Levamisole-induced vasculitis has been reported in patients who use cocaine. PTU, an older thyroid medication, and several other medications have been associated with the development of vasculitis. Vasculitis can also present as a paraneoplastic phenomenon, meaning that it's associated with either a known or an occult cancer or as a result of an underlying infection. -
QuestionIs vasculitis a chronic disease?
 Meera Subash, MDDr. Meera Subash is a board certified Rheumatologist and Internist. She specializes in scaling up healthcare technology solutions for rheumatic and chronic disease management. Dr. Subash holds a BA in Human Biology from Stanford University and a Doctor of Medicine (MD) from Texas Tech University Health Sciences Center. She completed a residency in Internal Medicine at The University of California, San Diego, where she served as Chief Resident in Quality and Patient Safety at The VA San Diego Healthcare System. Dr. Subash also completed a fellowship in Rheumatology at The University of California, San Francisco - School of Medicine. She is currently pursuing another fellowship in Clinical Informatics at The University of California, San Francisco - School of Medicine.
Meera Subash, MDDr. Meera Subash is a board certified Rheumatologist and Internist. She specializes in scaling up healthcare technology solutions for rheumatic and chronic disease management. Dr. Subash holds a BA in Human Biology from Stanford University and a Doctor of Medicine (MD) from Texas Tech University Health Sciences Center. She completed a residency in Internal Medicine at The University of California, San Diego, where she served as Chief Resident in Quality and Patient Safety at The VA San Diego Healthcare System. Dr. Subash also completed a fellowship in Rheumatology at The University of California, San Francisco - School of Medicine. She is currently pursuing another fellowship in Clinical Informatics at The University of California, San Francisco - School of Medicine.
Board Certified Rheumatologist Vasculitis itself is not really a disease. Rather, vasculitis is a symptom of another disease, such as Kawasaki disease, polyarteritis nodosa, giant cell arteritis, or hypersensitivity vasculitis.
Vasculitis itself is not really a disease. Rather, vasculitis is a symptom of another disease, such as Kawasaki disease, polyarteritis nodosa, giant cell arteritis, or hypersensitivity vasculitis.
Warnings
- Vasculitis can mimic other diseases. That's why it can be difficult to diagnose, particularly if you're trying to do so at home. Make sure to visit your doctor if you are noticing odd symptoms.⧼thumbs_response⧽
References
- ↑ https://www.nhlbi.nih.gov/health-topics/vasculitis
- ↑ https://www.nhs.uk/conditions/vasculitis/
- ↑ Meera Subash, MD. Board Certified Rheumatologist. Expert Interview. 5 February 2021.
- ↑ https://medlineplus.gov/vasculitis.html
- ↑ https://my.clevelandclinic.org/health/symptoms/10880-fever
- ↑ https://my.clevelandclinic.org/health/diseases/12101-vasculitis
- ↑ https://www.nhs.uk/conditions/vasculitis/
- ↑ https://www.versusarthritis.org/about-arthritis/conditions/vasculitis/
- ↑ https://my.clevelandclinic.org/health/diseases/12101-vasculitis
- ↑ https://my.clevelandclinic.org/health/diseases/14893-iga-vasculitis-henoch-sch%C3%B6nlein-purpura
- ↑ https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Vasculitis
- ↑ https://www.nhs.uk/conditions/mouth-ulcers/
- ↑ https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Vasculitis
- ↑ https://www.hopkinsvasculitis.org/vasculitis/symptoms-vasculitis/
- ↑ https://my.clevelandclinic.org/health/symptoms/17696-coughing-up-blood
- ↑ https://www.nhs.uk/conditions/vasculitis/
- ↑ https://www.hopkinsvasculitis.org/vasculitis/diagnosing-vasculitis/
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/iga-vasculitis
- ↑ https://www.nhlbi.nih.gov/health-topics/vasculitis
- ↑ https://www.niddk.nih.gov/health-information/kidney-disease/iga-vasculitis
- ↑ https://www.hopkinsvasculitis.org/vasculitis/diagnosing-vasculitis/
- ↑ https://www.hopkinsvasculitis.org/vasculitis/diagnosing-vasculitis/
- ↑ https://www.nhlbi.nih.gov/health/vasculitis/diagnosis
- ↑ https://www.nhlbi.nih.gov/health-topics/vasculitis
- ↑ https://my.clevelandclinic.org/health/diagnostics/4992-echocardiogram-transesophageal-tee
- ↑ https://www.hopkinsvasculitis.org/vasculitis/diagnosing-vasculitis/
- ↑ https://emedicine.medscape.com/article/1172488-workup#c5















-Step-14.webp)














































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...