This article was co-authored by Chris M. Matsko, MD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
There are 8 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 94% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 27,469 times.
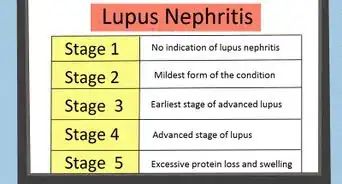
People affected by lupus anticoagulant antibodies (also known as Hughes syndrome, phospholipid antibody syndrome and antiphospholipid syndrome) have an increased risk of thrombosis (blood clots), which can cause strokes, heart attacks, and miscarriages.[1] Although these antibodies were first discovered in lupus patients, half of the people carrying lupus anticoagulant antibodies (LA) do not have lupus. With proper diagnosis and treatment, the harmful effects of LA can be avoided or at least managed.
Steps
Identifying and Diagnosing the Presence of Anticoagulants
-
1Consider any symptoms you may be having. Although there may not be any at all, some symptoms include having had one or more unexplained miscarriages, stroke, heart attack, and/or blood clots in the legs or lungs (clots may also occur in the brain, renal vein, or arteries).[2]
-
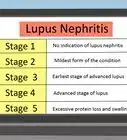
2Find out if you have any other diseases that might make you more susceptible to LA. If you suffer from something such as lupus, inflammatory bowel disease, chronic infections, or tumors, you may be more likely to develop LA.[3]
- Keep in mind that LA may develop at any time. Just because you didn’t have it 10 years ago, doesn’t mean you don’t have it now.
Advertisement -
3Contact your doctor. If you experience any of the following symptoms contact your doctor immediately, as it could be an indication that a potentially life threatening blood clot has formed:[4]
- Swelling and redness in your legs.
- Shortness of breath.
- Pain, numbness, or loss of color in an arm or leg.
-
4Ask your doctor about getting a Partial Thromboplastin Time (PTT) test. If you are having symptoms, or feel that you are susceptible to LA, a PTT test can determine whether or not you have anticoagulant antibodies present in your blood. Using a needle, blood is collected from a vein (usually the arm) and placed in a specimen container. A chemical is then added to the blood sample to measure how long it takes for the blood to clot.[5]
- Certain medications may affect the test results, so you should be sure to tell your doctor about any prescription and nonprescription medications you are taking to ensure you receive accurate results.
-
5Confirm the results. If you receive an abnormal result in your PTT test, your doctor will likely order further testing to confirm the results. Some examples include the Russell viper venom time test, and the thromboplastin inhibition test.[6]
- These tests may be repeated more than once to monitor the development of LA, especially if you have also been diagnosed with Lupus.[7]
Treating Lupus Anticoagulants Medically
-
1Discuss a treatment plan with your doctor. Each person is different; therefore, you should discuss the different methods for treating LA with your doctor. He or she can help you determine what’s best for you. If you are not symptomatic, or if you have never had a blood clot in the past, you may not need any medical treatment.[8]
-
2Consider anticoagulant therapy to reduce the effect of the antibodies. This therapy involves taking blood thinning medications such as warfarin, heparin, or low-dose aspirin, which help prevent blood clots. They work by inhibiting the production of vitamin K (responsible for blood clotting) in the liver. This increases the time the blood takes to clot. During this therapy, the level of anticoagulant in your blood will be monitored to determine how much, and for how long you need to continue the therapy. Some people only need to take medication for a few months, while others may have to manage the anticoagulants for their entire life.[9]
- If LA is still present after the initial therapy, the therapy is usually continued for at least three additional months before the next testing is done.
- If the result of the second post-therapy testing shows that the patient's blood no longer contains lupus anticoagulants, the therapy is discontinued.
-
3Talk with your doctor about using steroids to lower antibody levels. Steroids work by reducing the activity of the immune system. The immune system creates the lupus anticoagulant antibodies, and steroids can be used to suppress their production. If the activity of the immune system is suppressed or reduced, then the level of lupus anticoagulant antibodies will also decrease.[10]
- Examples of steroids include cortisone, prednisone and methylprednisolone.
-
4Consider utilizing plasmapheresis as a treatment.[11] Plasmapheresis is a process in which the liquid part of the blood, also known as plasma, which contains the lupus anticoagulant antibodies, is separated from the cells. A machine removes the affected plasma and replaces it with good plasma, or a plasma substitute that does not contain the antibodies.
- This is also known as plasma exchange.
Treating Lupus Anticoagulants at Home
-
1Ask your doctor about discontinuing certain medications. Medications such as phenothiazines, birth control pills, phenytoin, hydralazine, quinine, ACE inhibitors and amoxicillin are drugs that can induce LA. If you believe your LA is caused by a medication you are taking discontinuing the medication can help. However, you should not discontinue any medication until you have confirmed with your doctor that it will be safe to do so.
-
2Quit Smoking to improve blood flow. The nicotine in cigarettes constricts the blood vessels and impedes blood flow. Smoking will only exacerbate the formation of blood clots, so it is best to abstain from it completely.[12]
-
3Exercise regularly to bolster your cardiovascular system. Exercise minimizes the chance of blood clot formation by improving blood flow to different parts of the body. Exercises such as brisk walking, jogging, stair climbing, cycling, swimming and aerobics all offer good ways to get moving.[13]
- Avoid sports or exercises with a high risk of injury, especially if you are on medication which makes it more difficult for your blood to clot.
-
4Lose weight to promote good blood flow. Obesity leads to overproduction of substances in the body that come from fat cells and liver cells. These substances can inhibit clot breakdown and promote clot formation.[14]
-
5Avoid excessive alcohol intake. Binge drinking makes platelets more likely to clump together into blood clots, which can lead to heart attack or stroke.[15] According to a study by Harvard researchers in 2005, binge drinking doubled the risk of death among people who had initially survived a heart attack.
- Binge drinking is defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) as patterns of drinking that bring blood alcohol concentration (BAC) levels to 0.08 grams per decilitre. For men, this usually means about 5 drinks over about a 2 hour period, for women this is typically 4 drinks in about a two hour period. [16] Keep in mind, however, that BAC is affected by many other factors besides gender.
-
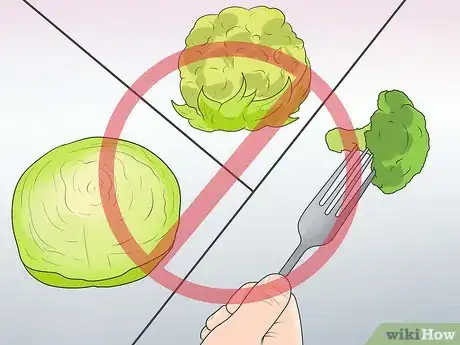
6Avoid vitamin K-rich foods to lower the chances of clotting. Vitamin K is responsible for the clotting of the blood. High intake of foods rich in vitamin K can contribute to blood clotting in persons with lupus anticoagulants. Also, if you are on anticoagulant therapy, such as warfarin or heparin, high vitamin K intake will counter the effect of the anticoagulant or blood thinning medications which are meant to inhibit the production of vitamin K.
- Foods rich in vitamin K include the following: asparagus, broccoli, brussels sprouts, cabbage, chili powder, cucumber, lettuce, oregano, parsley, prunes, spinach, spring onions.
-
7Move around. If you must spend a lot of time sitting (e.g. for work or on a long flight), get up and move around for a few minutes at least once per hour. If you cannot get up, at least try to move your feet and ankles around while sitting.[17] Doing so will make it more difficult for clots to form.
Warnings
- LA can be deadly if not treated properly. Before discontinuing any medication or taking action, discuss it with your doctor.⧼thumbs_response⧽
References
- ↑ https://medlineplus.gov/ency/article/000547.htm
- ↑ https://www.nhs.uk/conditions/antiphospholipid-syndrome/symptoms/
- ↑ https://my.clevelandclinic.org/health/diseases/21685-antiphospholipid-syndrome
- ↑ https://my.clevelandclinic.org/health/diseases/21685-antiphospholipid-syndrome
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK430980/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK430980/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK430980/
- ↑ https://medlineplus.gov/ency/article/000547.htm
- ↑ https://www.nhs.uk/conditions/antiphospholipid-syndrome/treatment/
- ↑ https://my.clevelandclinic.org/health/diseases/21685-antiphospholipid-syndrome
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2943363/
- ↑ https://my.clevelandclinic.org/health/diseases/21685-antiphospholipid-syndrome
- ↑ https://www.nhs.uk/conditions/antiphospholipid-syndrome/treatment/
- ↑ https://www.nhs.uk/conditions/antiphospholipid-syndrome/treatment/
- ↑ https://www.versusarthritis.org/about-arthritis/conditions/antiphospholipid-syndrome/
- ↑ http://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking
- ↑ https://medlineplus.gov/ency/article/000547.htm
About This Article
If you have lupus anticoagulant antibodies, you may not show symptoms but still have a higher chance of getting blood clots that can cause strokes, heart attacks, and miscarriages, so ask your doctor for a Partial Thromboplastin Time test if you feel you are at risk. Once your doctor confirms you have lupus anticoagulant antibodies, they will help you work out a personalized treatment plan, which may involve taking blood thinners or trying a plasma exchange. To further treat lupus anticoagulant antibodies at home, avoid nicotine and alcohol, and exercise regularly to bolster your cardiovascular system. For more advice from our Medical co-author, like how to treat lupus anticoagulant antibodies by reducing your vitamin K intake, scroll down.

















-Step-14.webp)
















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...