This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
This article has been viewed 23,961 times.
Frozen shoulder (or adhesive capsulitis) causes stiffness and pain in your shoulder joint. You are at risk of developing frozen shoulder if you are recovering from a medical condition like a stroke or a mastectomy. It’s most common in individuals over forty years of age and in women, typically appearing in 3 stages: freezing (painful stage), frozen (adhesive stage), and thawing (recovery stage). Frozen shoulder can be difficult to diagnose, as its symptoms are similar to other health issues. You can diagnose this medical condition by checking for the symptoms and by checking with your doctor. You can then consult with your doctor to treat the issue so it does not get worse.
Steps
Checking for the Symptoms of Frozen Shoulder
-
1Check for stiffness and pain in the shoulder. The first stage of frozen shoulder is the “freezing” phase. In this phase, you will experience stiffness and pain in your shoulder that builds up over time, usually 2-9 months. The onset of pain is slow and gradual and localizes near the deltoid insertion. Most people describe it as achy, but it can become sharp when the affected shoulder reaches its extreme range of motion. Movement of your shoulder will be limited or very difficult without pain.[1]
- You may also notice your shoulder hurts more at night and when you lie down on the side with the frozen shoulder. You may not be able to sleep on the affected side.
-
2Notice if you cannot rotate your arm outward. The second stage is the “frozen” or stiff phase. It usually lasts 4-12 months. The pain in the shoulder will ease but you will still feel stiffness and limited movement. You cannot rotate your arm outward and you may notice the muscles around your shoulder appear weak or skinny due to underuse.[2]Advertisement
-
3Check if the pain goes away after several years. The final stage is the “thawing” phase, where your shoulder starts to thaw out and the symptoms go away temporarily. This can take several months to three years. The pain and stiffness in your shoulder will go away and your shoulder will go back to normal and you’ll notice a gradual improvement in your range of motion. That is, until the “freezing” phase starts up again.[3]
-
4Notice if you cannot drive, dress, or sleep comfortably. Throughout the first two phrases of frozen shoulder, you will find it hard to do daily tasks like driving, dressing, or sleeping. You may develop sleep issues and have to ask others to drive or dress you due to your frozen shoulder.[4]
- You may also find it difficult to do basic things like scratch your back and pick up items from the floor with your affected arm.
Consulting with Your Doctor
-
1Share your medical history with your doctor. At your appointment, your doctor will ask you about your medical history to determine if you have had a medical condition that makes you susceptible to frozen shoulder. People who have had a stroke or a mastectomy are at a higher risk for this condition.
- Your doctor will also want to rule out other medical conditions that could cause pain and stiffness in the joint, such as osteoarthritis, shoulder strain, dislocations, rotator cuff problems, subacromial impingement syndrome, acromioclavicular joint disease, impingement syndrome, sternoclavicular joint sprain, and glenohumeral instability.
-
2Let the doctor examine the shoulder. Because frozen shoulder takes a long time to develop and go through each phase, it can be difficult to diagnosis on your own. Let your doctor perform a physical exam of your shoulder to confirm your condition. They will move it carefully in all directions to check for pain.[5]
- They will also check to see if the movement of your shoulder is limited. They may try to rotate or lift your arm to better examine your shoulder.
- They may also examine your neck and spine to rule out degenerative disk disease or facet joint arthritis that might cause shoulder pain.
-
3Have an MRI done on the shoulder. A Magnetic Resonance Imaging (MRI) is done on your shoulder to look for problems in the soft tissues of your shoulder. It will tell the doctor if there are any problems like a torn rotator cuff in your shoulder, which can cause frozen shoulder.[6]
- An MRI is painless and can often be done at the doctor’s office during your appointment.
-
4Allow the doctor to do an X-ray on the shoulder. X-rays can also help your doctor look for issues or damage to the bones in your shoulder that could be causing the frozen shoulder. Your doctor can also check for other issues like arthritis.[7]
- An X-ray does not cause any pain and can be performed at the doctor’s office.
Treating Frozen Shoulder
-
1Take anti-inflammatory painkillers. Your doctor will likely recommend that you take anti-inflammatory painkillers like ibuprofen, diclofenac, and naproxen. These medications can ease pain and reduce swelling in your shoulder.[8]
- Follow the dosage instructions on the label and never take more than recommended. Do not use them for more than 2 to 4 weeks.
-
2Apply ice. Ice is a potent anti-inflammatory agent that can reduce pain as well as muscle spasms. You can make your own ice pack wrapped in a towel or plastic bag, or even use a package of frozen peas. Apply the ice as often as desired and as long as inflammation is present.
- Never place ice directly on an injury and don't apply it for more than 30 minutes at one time – more than that can damage the skin and nerves.[9]
- You also shouldn’t use ice packs on your left shoulder if you have a heart condition.
-
3Get a steroid injection. Your doctor can also administer a steroid injection into or near your shoulder joint. This will help to reduce pain and swelling temporarily. Your symptoms will return over time but you may like the initial relief of the steroid injection.[10]
-
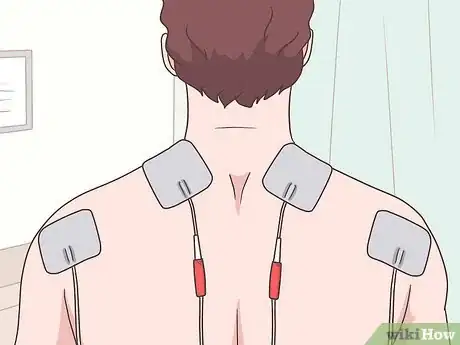
4Get TENS treatments. If conservative therapy fails, in some cases transcutaneous electrical nerve stimulation, or TENS, may reduce pain. This treatment uses a low-voltage electrical current that in some people seems to stimulate nerves in the affected area, “scrambling” the normal pain signals to the brain or causing the body to produce natural pain killers like endorphins.[11]
- TENS is generally considered safe. Still, always talk to your doctor if you are considering an alternative therapy.
-
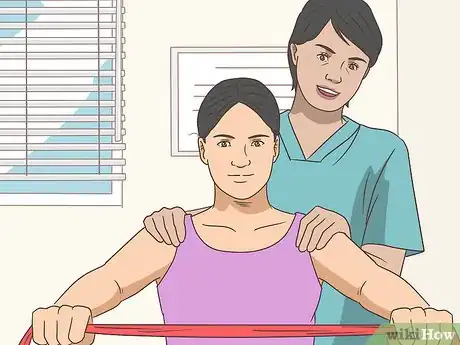
5Work with a physiotherapist. Your doctor may also recommend a physiotherapist that you can work with to help regain movement in your shoulder and to reduce pain. The physiotherapist will show you shoulder exercises you can do at home and in your sessions with them.[12]
- The exercises will prevent the shoulder for stiffening up and allow for a wide range of movement.
References
- ↑ https://patient.info/health/frozen-shoulder-leaflet
- ↑ https://patient.info/health/frozen-shoulder-leaflet
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=a00071
- ↑ https://patient.info/health/frozen-shoulder-leaflet
- ↑ https://patient.info/health/frozen-shoulder-leaflet
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=a00071
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=a00071
- ↑ http://www.mayoclinic.org/diseases-conditions/frozen-shoulder/basics/treatment/con-20022510
- ↑ https://www.scoi.com/patient-resources/health-articles/should-you-ice-or-heat-injury
















-Step-3-Version-3.webp)


















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...