This article was medically reviewed by Shari Forschen, NP, MA. Shari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
There are 17 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 286,779 times.
Studies show that antibiotics, particularly those in the penicillin and sulfa groups, are the most common cause of drug allergies.[1] Most drug allergies are usually limited to hives, swelling, and skin rashes, but some people experience rare and life-threatening reactions, called anaphylaxis.[2] Drug allergies are caused by your immune system mistaking the antibiotic for a foreign substance, inflaming your skin or, in more severe cases, restricting airways and causing shock, which can lead to unconsciousness or death. Experts note that if you experience the symptoms of anaphylaxis, it's crucial that you seek medical help immediately, as it is a medical emergency.[3] Learning how to treat skin rashes and recognize the signs of a more severe reaction can help you feel your best, and could save your life.
Steps
Seeking Medical Assistance
-
1Go to the emergency room or call emergency services. If you believe you are experiencing an allergic reaction to antibiotics, seek medical help immediately, no matter how severe your symptoms are. Many allergic reactions are confined to skin rashes and will not result in any complications, but it's important to talk to your doctor about any reaction. Some rashes can be caused by Stevens-Johnson syndrome, a severe complication that needs hospitalization.[4] Other rashes are a precursor to anaphylaxis, which can be life-threatening if not treated.[5] Seek immediate medical assistance if you experience:[6]
- Fever
- Sore throat/mouth, with or without a cough
- Facial swelling
- Tongue swelling
- Skin pain
- Rashes and/or blisters
- Hives
- Difficulty breathing or tightness in the throat
- An abnormally hoarse voice
- Hives or swelling
- Nausea or vomiting
- Abdominal pain
- Dizziness or fainting
- Rapid heartbeat
- Feelings of doom
-
2Stop taking the medicine. If you're experiencing any allergic reactions to an antibiotic, you must discontinue using that medication, and avoid all exposure to it. Exposure can happen accidentally, so it's important to take preventative action.
- Tell healthcare workers about your allergy any time you are receiving medical treatment of any kind.[7] Ensure that this is included in your medical records for future reference, but don't ever assume medical personnel have seen the chart or know of your allergy. It is your responsibility to communicate your allergies when being treated.
- Wear a medical alert bracelet. These bracelets can be invaluable, especially if you ever require emergency care while unconscious. It alerts healthcare workers about your allergy in times when you cannot communicate your allergy.[8]
- You may want to carry an epinephrine auto-injector (commonly called an "Epipen"). This is typically only needed for people susceptible to anaphylaxis, but your doctor may recommend that you have one if your allergies are severe.[9]
Advertisement -
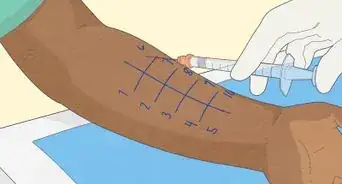
3Ask your doctor about desensitization. In most cases, if you have a known allergy, your doctor will prescribe an alternative drug. In some very isolated cases where benefit outweighs the risk, and there are no alternative treatments, that may not be an option. If you must take a particular drug and have a known allergy to that medication, your doctor may work with you through a drug desensitization treatment.[10]
- During drug desensitization treatments, your doctor will administer a minimal dose of the drug you're allergic to and will monitor your symptoms. Then they will administer an increasingly larger dose every 15 to 30 minutes, over the course of several hours or even days.[11]
- If you can tolerate the desired dosage without any adverse reactions, your doctor may then safely prescribe a regular course of the medication.[12]
- This is usually done in severe cases and should only be done by a professional with training in emergency treatment.
Treating Minor Allergies with Medication
-
1Take oral antihistamines. Antihistamines increase the passage of white blood cells in your body while reducing your body's production of histamine, which your immune system releases in response to an allergen.[13] Depending on the severity of your reaction, your doctor may recommend a prescription-strength antihistamine, or they may advise you to use an over-the-counter antihistamine.[14]
- Diphenhydramine (Benadryl). In the case of severe allergy, it is always good to use diphenhydramine (Benadryl) as this is a strong antihistamine. Consider keeping some in your first aid kit for emergencies.
- Other common over-the-counter antihistamines include loratadine (Claritin), cetirizine (Zyrtec), or chlorpheniramine (Aller-Chlor).[15]
- The dosage you take will depend on some factors, including your age and the particular antihistamine you are taking.[16] Follow the instructions on the package, or ask a doctor or pharmacist for dosage instructions.
- Do not drive or operate machinery after taking antihistamines, as most first-generation antihistamines (like Benadryl) can cause severe drowsiness, making it difficult to function.[17]
- Do not use antihistamines if you are pregnant or breastfeeding. These medications may cause adverse side effects in infants and could cause birth defects in developing fetuses.[18]
- Do not give antihistamines to children under four years of age. If your little one is experiencing a severe allergy, take them to the emergency room. Do not wait it out with respiratory difficulties or facial swelling — get emergency care as soon as possible.
- Some elderly patients experience adverse side effects from an antihistamine. These side effects include confusion, dizziness, drowsiness, nervousness, and irritability.[19] This places them at risk for falling. Falling and breaking hips can be fatal to the elderly, as their immune systems are not as robust as young to middle-aged adults.
-
2Apply calamine lotion. If you are experiencing a rash or hives caused by an allergic reaction, calamine lotion may help soothe the itching and discomfort.[20]
- Calamine lotion contains a mixture of calamine, zinc oxide, and other ingredients. Calamine and zinc oxide are both known anti-itch topical medications.[21]
- Calamine is for external use only. You should not ingest calamine, nor should you apply it near the eyes, nose, mouth, genitals, or anal areas.[22]
-
3Try hydrocortisone cream. Low-dose hydrocortisone cream is available over-the-counter at 0.5 or one percent concentrations, though stronger concentrations are available by prescription. This topical medication suppresses your body's immune system reaction to relieve skin irritations, itching, and rashes.[23]
- Hydrocortisone cream is a topical steroid. This class of medication is generally safe, but should not be used for more than seven consecutive days to avoid complications, including itching, cracked skin, thinned skin, and acne.[24]
- Topical hydrocortisone should not be used on children under two years of age. Do not use this medication if you are pregnant or breastfeeding, unless otherwise directed by your physician.[25]
- Apply to the affected areas one to four times daily for up to seven days. Avoid contact with the eyes if you are applying this medication to your face.[26]
Using Home Remedies and Lifestyle Changes
-
1Take a tepid bath. Both hot and cold temperature extremes can affect hives, and may cause them to worsen when hives are already present.[27] For best results, take a comfortable, room-temperature bath to soothe skin rashes.
- Sprinkle baking soda, uncooked oatmeal, or finely-ground colloidal oatmeal into your bath to help relieve itching.
- Avoid using soap until you know whether or not a given soap brand will irritate your hives.[28]
-
2Apply a cold compress. Cool, wet compresses can help alleviate the symptoms associated with rashes and hives. Exposure to a cold, wet bandage or dressing can help soothe irritated skin, and may help reduce inflammation by slowing blood flow to the rash.
-
3Avoid irritants. There are many things that can irritate hives and rashes. Even if you are not normally affected by common household irritants, it's best to avoid them until you know how your current rash/hives will react to these items.[29] Common irritants include:[30]
- Cosmetics
- Dye (including dye used in clothing)
- Fur and leather products
- Hair coloring
- Latex
- Nickel products, including jewelry, zippers, buttons, and kitchen utensils
- Nail care products, including nail polish and artificial nails
- Soap and household cleaning products
-
4Refrain from scratching or rubbing. Even though your rash may itch very intensely, it's important to avoid scratching or rubbing the rash/hives. Scratching can cause the skin to break, leaving you prone to infection and delaying the healing process.[31]
-
5Avoid exposure to heat. In some people, exposure to heat and humidity can further irritate hives and rashes. If you are experiencing rashes or hives, avoid exposure to heat, humidity, and exercise.
-
6Wear comfortable clothing. If you are experiencing rashes and hives, it's important that you choose the right clothing to prevent further irritating your skin. Choose loose, smooth-textured material like cotton. Avoid constricting clothing and any materials that are rough and scratchy like wool.
Expert Q&A
-
QuestionWhat can I use to get rid of an irritating rash on my genitals that I contracted after being hospitalized?
 Shari Forschen, NP, MAShari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
Shari Forschen, NP, MAShari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
Master's Degree, Nursing, University of North Dakota Go to your doctor to get adequate treatment. You may have a secondary infection from hospitalization and may need specific antibiotics to treat it.
Go to your doctor to get adequate treatment. You may have a secondary infection from hospitalization and may need specific antibiotics to treat it. -
QuestionI took the antibiotic bacterium and I immediately I starting itching in my vagina then got a big red sore. It's not filled with any fluid but it's painful. What can I do to help get rid of it?
 Shari Forschen, NP, MAShari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
Shari Forschen, NP, MAShari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
Master's Degree, Nursing, University of North Dakota Go back to physician who prescribed the antibiotic and have them assess you.
Go back to physician who prescribed the antibiotic and have them assess you. -
QuestionWhat kind of cream to used if the rash is on my arms?
 Shari Forschen, NP, MAShari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
Shari Forschen, NP, MAShari Forschen is a Registered Nurse at Sanford Health in North Dakota. Shari has worked in healthcare since 1996 and her expertise lies in acute care bedside nursing on a medical oncology floor. She received her degree from Medcenter one College of Nursing in 2003 and her Family Nurse Practitioner Masters from the University of North Dakota in 2014. Shari is a member of the American Nurses Association.
Master's Degree, Nursing, University of North Dakota This website is not a diagnostic website, so your best bet is to talk to your doctor. Good general advice is to use a cream without added perfumes or scents, and one that is geared towards sensitive skin. If this does not help, then going to a medical provider for advice is necessary.
This website is not a diagnostic website, so your best bet is to talk to your doctor. Good general advice is to use a cream without added perfumes or scents, and one that is geared towards sensitive skin. If this does not help, then going to a medical provider for advice is necessary.
References
- ↑ http://acaai.org/allergies/types/drug-allergies
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/symptoms/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/symptoms/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/stevens-johnson-syndrome/basics/definition/con-20029623
- ↑ http://acaai.org/allergies/anaphylaxis
- ↑ http://acaai.org/allergies/anaphylaxis
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/prevention/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/prevention/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/prevention/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/treatment/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/treatment/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/treatment/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/treatment/con-20033346
- ↑ http://www.mayoclinic.org/diseases-conditions/drug-allergy/basics/treatment/con-20033346
- ↑ http://www.mayoclinic.org/drugs-supplements/antihistamine-oral-route-parenteral-route-rectal-route/description/drg-20070373
- ↑ http://www.mayoclinic.org/drugs-supplements/antihistamine-oral-route-parenteral-route-rectal-route/proper-use/drg-20070373
- ↑ http://www.mayoclinic.org/drugs-supplements/antihistamine-oral-route-parenteral-route-rectal-route/before-using/drg-20070373
- ↑ http://www.mayoclinic.org/drugs-supplements/antihistamine-oral-route-parenteral-route-rectal-route/before-using/drg-20070373
- ↑ http://www.mayoclinic.org/drugs-supplements/antihistamine-oral-route-parenteral-route-rectal-route/before-using/drg-20070373
- ↑ http://www.mayoclinic.org/drugs-supplements/calamine-topical-route/description/drg-20062463
- ↑ http://www.medicinenet.com/calamine_lotion-topical/article.htm
- ↑ http://www.mayoclinic.org/drugs-supplements/calamine-topical-route/proper-use/drg-20062463
- ↑ https://nationaleczema.org/eczema/treatment/topical-corticosteroids/hydrocortisone-faq/
- ↑ https://nationaleczema.org/eczema/treatment/topical-corticosteroids/hydrocortisone-faq/
- ↑ https://nationaleczema.org/eczema/treatment/topical-corticosteroids/hydrocortisone-faq/
- ↑ https://www.nlm.nih.gov/medlineplus/druginfo/meds/a682793.html
- ↑ http://acaai.org/allergies/types/skin-allergies/hives-urticaria
- ↑ http://acaai.org/allergies/types/skin-allergies/contact-dermatitis
- ↑ http://acaai.org/allergies/types/skin-allergies/contact-dermatitis
- ↑ http://acaai.org/allergies/types/skin-allergies/contact-dermatitis
- ↑ http://www.healthline.com/health/rashes
About This Article
If you have a skin rash caused by an antibiotic, stop taking the medication immediately and visit your doctor for treatment. To relieve the symptoms of your rash at home, hold a cool, wet bandage or dressing to your skin to reduce inflammation. Alternatively, take a lukewarm bath to soothe your skin. Sprinkle some baking soda or uncooked oatmeal in the bath to help relieve your itching. You can also apply calamine lotion or hydrocortisone cream to your skin to reduce itching and redness. Try to avoid scratching or rubbing the rash, which can make it worse. For more tips from our Medical co-author, including how to treat a minor allergic reaction with antihistamines, read on.





















-Step-17-Version-3.webp)




















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...