This article was co-authored by Peter Gardner, MD. Peter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelor’s degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York (Columbia) Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 105,331 times.
Helicobacter pylori (H. pylori) is a bacteria that causes chronic inflammation of inner lining of the stomach and is the leading cause of peptic ulcer disease worldwide. Over 50% of American people are infected with H. pylori and, in developing countries, the percentage may reach as high as 90%; however, only one in six persons develops symptoms of peptic ulcer. The only way to know for sure if you are infected is getting tested by a medical professional.
Steps
Recognizing the Symptoms
-
1Watch for dull pain in your stomach that does not go away.[1] An H. Pylori infection can cause peptic ulcers in your stomach and lower intestine. As H. Pylori rarely causes symptoms in and of itself, a peptic ulcer can alert you to a potential infection. If you have a peptic ulcer, you may display some of the following symptoms:[2]
- You may have a dull pain in your stomach that does not go away. Pain will usually come two to three hours after eating.
- The pain will come and go for several weeks, and may sometimes happen in the middle of the night when your stomach is empty.
- The pain may go away temporarily when you take medications like antacids and other over-the-counter pain medications.
-
2Pay attention to prolonged nausea. You may experience nausea if you have an H. Pylori infection.[3] Pay attention to your body and notice of any nausea you experience.[4]
- You may vomit when you experience nausea. With an H. Pylori infection, your vomit may include blood. You may also notice a substance that resembles coffee grounds.
- Nausea can be caused by a wide variety of factors, such as motion sickness, the flu, eating or drinking something that did not sit well with you, or morning sickness during pregnancy. If your nausea is persistent, and you do not have any obvious cause, it may be related to an H. Pylori infection.
Advertisement -
3Consider your appetite. A loss of appetite can also be a symptom of an H. Pylori infection. You may not be interested in food or eating. This may come in conjunction with the feelings of nausea and indigestion associated with the disease.[5]
- If you're having a loss of appetite, which is accompanied by unexplained weight loss, you may want to talk to a doctor. Loss of appetite is a common symptom of many diseases, including some cancers.[6] See your doctor to rule out any serious conditions if you're experiencing a loss of appetite.
-
4Watch out for unusual changes in your body. You may experience some odd changes in your body when you have an H. Pylori infection. Take note of any sudden changes and see a doctor for evaluation.[7]
- It's not uncommon for the abdomen to be bloated slightly during an H. Pylori infection.
- You may also notice your stools have become increasingly black and tarry.
- Sometimes, people with an H. Pylori infection will experience frequent bouts of the hiccups.
-
5Assess your risk factors. As symptoms are rare, and easily mistaken for other conditions, think about your risk factors. If you have a lot of risk factors for an H. Pylori infection, symptoms like stomach cramps may be cause for concern.[8]
- If you live in crowded conditions, such as a small home with many people, this increases your risk of infection.
- If you don't have regular access to clean water, you may also have an increased risk of infection.
- If you live in a developing country, or have recently visited one, this also increases your risk for infection.
- If you're living with someone who you know has H. Pylori, this means you're more likely to have the infection yourself.
-
6Seek immediate medical attention if symptoms get worse quickly. H. Pylori is not usually a medical emergency; however, some symptoms can become serious. If you experience any of the following, seek immediate medical attention:[9]
- Difficulty swallowing
- Severe abdominal pain
- Bloody stools
- Bloody vomit
Seeking Medical Testing
-
1Talk with your doctor about testing. Talk to your doctor about your symptoms and why you think you may have H. Pylori and see if she agrees that a test is necessary. People who should be tested for H. Pylori include those with certain gastric tumors, active peptic ulcer disease, or history of peptic ulcer disease. People who are under the age of 55 who have dyspepsia may be candidates for treatment.
-
2Take a breath test.[10] Though this is not the most accurate test for H. Pylori, it is not as invasive as some other options. During this test, you swallow a substance that contains a waste product called urea. Urea breaks down proteins in the stomach. If an infection is present, the urea will be converted to carbon dioxide which can be detected in the breath.[11]
- You will need to prepare for a breath test for about two weeks. Your doctor will advise you to stop taking any over-the-counter or prescription medication you're using to treat H. Pylori.
- You will swallow the urea in the doctor's office. After 10 minutes, you'll be asked to exhale and the doctor will test your breath for carbon dioxide.
-
3Consider a stool test.[12] Your doctor may want to test your stool for traces of H. Pylori. This is usually done after treatment to confirm H. Pylori has been eradicated and you no longer have an infection.[13]
- Your doctor may order a stool test after a positive breath test and subsequent treatment.
- Listen to your doctor's instructions carefully in regards on how to collect and store your stools. Collection methods vary by hospital.
- There is also a rapid stool antigen test for H.Pylori. Talk with your doctor about this option — it may not be available everywhere.
-
4Get a blood test done.[14] A blood test can also be used to check for H. Pylori; however, this test may not be as accurate as a breath test. It can only test whether your body currently contains H. Pylori antibodies. It cannot tell if you are presently infected.[15]
- Your doctor may order a blood test for a variety of reasons. She may want to confirm an infection. If your doctor orders a blood test, trust that your doctor knows what's best for you. It's a simple procedure that should not take long.
- Other methods that are not as commonly utilized include PCR chain reaction, salivary assays, urinary assays, and C13-urea blood test.
-
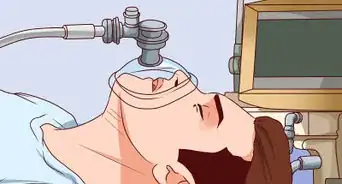
5See if your doctor wants a biopsy. A biopsy is the most accurate way to test for H. Pylori.[16] In a biopsy, a small tissue sample is taken from your stomach. You'll have to have an endoscopy, a somewhat invasive medical procedure, conducted at the hospital to remove the sample.[17]
- During an endoscopy, a small tube will be inserted into your mouth and then fed into your stomach. In addition to removing a tissue sample, your doctor will check for inflammation.[18]
- While the most accurate means to diagnose H. Pylori, your doctor will not call for this procedure unless an endoscopy is necessary for other reasons. Your doctor may want to conduct an endoscopy if you have a peptic ulcer or are at risk for stomach cancer.
Coping with an Infection
-
1Take drugs to suppress acid. After an infection is diagnosed, your doctor will recommend you take a variety of drugs to suppress stomach acid. Triple antibiotic therapy is the first line treatment for H. Pylori. The regimen most commonly employed for first line treatment include a proton pump inhibitor and two antibiotics for coverage against the bacteria. Treatment should last 14 days. Your doctor will recommend which particular drugs are best for you based on your medical history and current condition.[19]
- Proton pump inhibitors (PPIs) are a range of drugs that stop acid production in the stomach. Your doctor may prescribe these drugs if excessive stomach acid is causing you pain.
- Histamine (H-2) blockers can also block acid production by stopping the production of a substance called histamine. Histamine can trigger acid production in the stomach.
- Bismuth subsalicylate, sold commercially as Pepto-Bismol, can coat stomach ulcers and can reduce pain.
- Follow your doctor's instructions carefully in regards to which drugs he recommends. If you are on any existing medication, make sure to ask whether your current meds will interact with medication used to treat H. Pylori.
-
2Continue testing throughout treatment. Your doctor will want to make sure treatment of your H. Pylori was successful. He or she will probably want to do another round of testing about four weeks after your treatment. In the event treatment was unsuccessful, you may undergo a second round of treatment and be prescribed antibiotics. Usually the second round of testing includes upper endoscopy, fecal antigen test, or urease breath test for confirmation of eradication.
-
3Talk to your doctor about whether regular screenings are right for you. You may want to be regularly screened for H. Pylori if you have a high risk of stomach cancer. An H. Pylori infection may increase your risk of developing stomach cancer. Discuss your concerns with your doctor and she will decide if regular screening for H. Pylori is right for you.[20]
Expert Q&A
-
QuestionHow do you test for H pylori?
 Peter Gardner, MDPeter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelor’s degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York (Columbia) Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.
Peter Gardner, MDPeter W. Gardner, MD is a board certified physician who has practiced Gastroenterology and Hepatology for over 30 years. He specializes in diseases of the digestive system and liver. Dr. Gardner earned his Bachelor’s degree from the University of North Carolina and attended Georgetown Medical School. He completed his residency in Internal Medicine and then his fellowship in Gastroenterology at the University of Connecticut. He is a previous Chief of Gastroenterology at Stamford Hospital and remains on the staff. He is also on the staff of Greenwich Hospital and New York (Columbia) Presbyterian Hospital. Dr. Gardner is an Approved Consultant in Internal Medicine and Gastroenterology with the American Board of Internal Medicine.
Board Certified Gastroenterologist There are several different methods, including a breath test, a stool test, a blood test, and an endoscopy.
There are several different methods, including a breath test, a stool test, a blood test, and an endoscopy. -
QuestionCan I take creatine pill if I'm tested H. pylori positive?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician I would try to avoid all supplements and only take the medication that is prescribed by your doctor. You do not want to have any unwanted reactions.
I would try to avoid all supplements and only take the medication that is prescribed by your doctor. You do not want to have any unwanted reactions.
References
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ http://www.hopkinsmedicine.org/healthlibrary/conditions/digestive_disorders/helicobacter_pylori_85,P00373/
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Gastritis
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/helicobacter-pylori
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Gastritis
- ↑ http://www.cancer.org/cancer/pancreaticcancer/detailedguide/pancreatic-cancer-signs-and-symptoms
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Gastritis
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/helicobacter-pylori
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/helicobacter-pylori
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/007501.htm
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/007501.htm
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/007501.htm
- ↑ Peter Gardner, MD. Board Certified Gastroenterologist. Expert Interview. 25 August 2020.
- ↑ https://www.nlm.nih.gov/medlineplus/ency/article/007501.htm
- ↑ http://my.clevelandclinic.org/health/diseases_conditions/hic_Gastritis
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/helicobacter-pylori
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/helicobacter-pylori
About This Article
Common symptoms of H. Pylori include dull stomach pain that doesn’t go away, prolonged nausea, vomiting, and lack of appetite. You may also encounter a bloated abdomen, black and tarry stools, and frequent bouts of hiccups. H. Pylori is not usually a medical emergency, however, if you experience difficulty swallowing, severe abdominal pain, or bloody stools or vomit, you should seek medical attention immediately. For more tips from our Medical co-author, including how to manage an H. Pylori infection, read on!







-Step-3-Version-3.webp)
















-Step-11.webp)













































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...