This article was medically reviewed by Troy A. Miles, MD. Dr. Miles is an Orthopedic Surgeon specializing in Adult Joint Reconstruction in California. He received his MD from the Albert Einstein College of Medicine in 2010, followed by a residency at the Oregon Health & Science University and fellowship at the University of California, Davis. He is a Diplomat of the American Board of Orthopaedic Surgery and is a member of the American Association of Hip and Knee Surgeons, American Orthopaedic Association, American Association of Orthopaedic Surgery, and the North Pacific Orthopaedic Society.
There are 18 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 24,368 times.
Trigger finger (TF), or stenosing tenosynovitis, is a condition in which a finger is forced to stay in a bent position making it difficult to straighten the affected finger. This disorder occurs when tendons in the finger swell, and the tendon sheath restricts movement of the finger.[1] Thus, the finger can become “stuck” in a bent position. When the finger is straightened, a snapping sound occurs, as if a trigger on a gun were being released. If this phenomenon becomes severe, the digit of the finger may be locked into a bent position. Learn about the steps you can take to understand whether or not you are being affected by trigger finger.
Steps
Recognizing Early Symptoms
-
1Identify pain in the base of the finger or palm. The most common symptom is pain experienced at the base of the finger or over the palm when trying to extend the finger. There is pain during extension or flexing of the finger because the tendon can no longer easily slide back out of the tendon sheath due to inflammation.
- If the inflamed portion of the tendon breaks free of its sheath, it may feel as if your finger is being dislocated.[2]
- Typically, the dominant hand is more likely to be affected by the disorder. In particular, the thumb, middle, and ring fingers. Also be aware that more than one finger can be affected at a time.[3]
-
2Notice a snapping sensation. When the affected finger is moved or extended, a “popping” or snapping sound (similar to the sound of cracked knuckles) can be heard. This occurs because the inflamed tendon is being pulled through a tendon sheath that is too narrow. It will happen when you straighten it and when you bend it.[4]Advertisement
-
3Notice any stiffness. Generally, stiffness will be worse in the morning. It is not clear why stiffness gets worse in the early hours of the day, but some suspect that this may be due to lack of cortisol (a hormone) at night to counteract substances that cause inflammation.[5] This is similar to "gelling" which occurs in hip and knee arthritis — inflammatory fluid builds up as you are not using the inflamed area at night and takes time in the morning to decrease that fluid.
- Generally, this stiffness will lessen as the finger is used throughout the day.[6]
-
4Look for bump or swelling. You may find a bump, or have swelling at the base of the affected finger or in the palm, this happens because the swelling causes the tendon to become bunched up into a hard knot.[7] The bump may also move when you move your finger because the tendon also moves when you move your finger.[8]
Recognizing Late Symptoms
-
1Notice your finger locked in a bent position. As the inflammation worsens, the finger will be unable to fully extend, which ultimately requires you to use the other hand to straighten the finger. In severe cases, the finger cannot be extended even with assistance.
- In some cases, it may abruptly pop straight from time to time, even when you are not trying to straighten it.[9]
-
2Notice any softness at the base of the involved finger. You may also find a nodule there that's tender. This is actually a knot in the lining of your tendon. It will be on the palm side at the base of the affected finger.
-
3See your doctor immediately if the joint feels hot and inflamed. This is an indication of infection, which is something you definitely don't want to wait around and see what happens with. Most trigger finger cases clear up on their own with adequate rest, and are not a cause for great concern.[10] However, infections can be very dangerous, even deadly if not treated quickly and properly.
- Dupuytren's contracture is another disorder that often gets mistaken for trigger finger, though it is not the same. With this disorder, the connective tissues thicken and shorten. That being said, it can occur in conjunction with trigger finger.[11]
-
4Be aware that an infection may lead to osteomyelitis. If the trigger finger is caused by infection of the synovium (lubricating membrane lining the joint), the infection may spread and cause osteomyelitis. Osteomyelitis is an infection of the bone where symptoms such as pain, fever, chills and swelling manifest.
- This is one of the main reasons seeing a doctor is advised, even if you're just experiencing mild joint pain. Although most cases of trigger finger go away, it is better to be safe than sorry.
- If you have recently had surgery, are an alcoholic, use steroids regularly, have sickle cell disease or rheumatoid arthritis, you should visit your doctor immediately as all these are risk factors for osteomyelitis.[12]
Understanding the Risk Factors
-
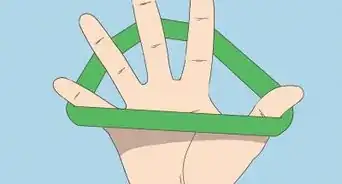
1Evaluate how often you use repetitive finger movements. People with occupations or hobbies that require routine, repetitive finger movements, such as operating machines or power tools and playing musical instruments may be at higher risk of developing trigger finger.[13]
- Constant grasping with forceful use of the finger to any object for an extended time can cause this condition due to repetitive trauma to the digits of the finger. Farmers, musicians, and even smokers (flicking the lighter) are at higher risk.[14]
-
2Consider whether or not you are between the ages of 40 and 60. Those most likely to develop trigger finger will be between 40 and 60 years old. This is perhaps because those who are older have spent considerably more time using their hands, and have likely sustained more damage over time than younger people.
-
3Find out if you have diabetes. Those with diabetes are at a greater risk of developing trigger finger. The elevated levels of glucose present in diabetes patients may change the balance of proteins in the body, which stiffens collagen (connective tissues in the body) thereby leading to the stiffening of tendons in the fingers.[15] The longer you have diabetes, the more likely you are to suffer from trigger finger. If you have diabetes and develop trigger finger, it can be indicative of other diabetic complications.[16]
-
4Know which conditions increase your risk of developing trigger finger. Consider other diseases such as gout, amyloidosis, thyroid problems, carpal tunnel syndrome, Dupuytren’s Contracture, De Quervain’s disease. Any of these diseases increases your risk of developing trigger finger. If you suffer from one or more, be conscientious of any symptoms of oncoming trigger finger.
- A recent study also found that most people with rheumatoid arthritis have swollen tendons, and may be at greater risk for developing trigger finger.[17]
-
5Be aware that women are more likely to suffer from trigger finger. Although it is not clear why, women tend to develop trigger finger more often than men.
Getting Diagnosed
-
1See your doctor. A simple medical history and physical exam of the affected finger must be performed in order to diagnose trigger finger. Your doctor will look for bumps or swollen spots in the affected area.[18]
- Your doctor will also likely search for the classic “popping and locking” that occurs in those suffering from trigger finger.[19]
-
2Be detailed and factual during your visit. Because trigger finger has a number of causes that are often unclear or questionable, it's wise to be as thorough and detailed as possible about your medical and family history. Even if you don't think it's related or important, it could be important for diagnosis and treatment.
- It is important that only factual information be given to the health care providers to ensure that a proper treatment plan can be developed. Patients are encouraged to answer questions in the most detailed way possible, and should not to hesitate to ask questions regarding possible treatment.
-
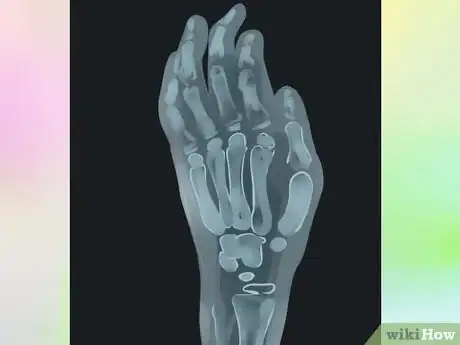
3Know that x-rays or any elaborate laboratory test are not required to diagnose trigger finger. It is only necessary for patients with history of inflammatory disease or trauma. In most cases, your doctor will rely on your symptoms, which is all the more reason to be honest and factual.[20]
References
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=a00024
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=a00024
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK459310/
- ↑ https://emedicine.medscape.com/article/1244693-overview
- ↑ http://arthritis.about.com/od/arthritissignssymptoms/a/Tips-For-Dealing-With-Morning-Stiffness.htm
- ↑ http://my.clevelandclinic.org/services/orthopaedics-rheumatology/diseases-conditions/hic-trigger-finger-and-dequervains-disease
- ↑ http://www.nhs.uk/Conditions/Trigger-finger/Pages/Causes.aspx
- ↑ http://www.nhs.uk/Conditions/Trigger-finger/Pages/Causes.aspx
- ↑ https://www.assh.org/handcare/blog/what-is-trigger-finger-and-what-can-i-do-about-it
- ↑ https://www.mountelizabeth.com.sg/healthplus/article/trigger-finger-common-questions
- ↑ http://dupuytrens-contracture.com/trigger-finger-dupuytren-contracture/
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/osteomyelitis#risk-factors
- ↑ https://www.assh.org/handcare/condition/trigger-finger
- ↑ https://my.clevelandclinic.org/health/diseases/7080-trigger-finger--trigger-thumb
- ↑ http://www.diabetesselfmanagement.com/Blog/David-Spero/diabetes-and-your-hands/
- ↑ http://clinical.diabetesjournals.org/content/19/3/132.full
- ↑ http://www.medicinenet.com/trigger_finger/article.htm
- ↑ https://www.pennstatehealth.org/services-treatments/trigger-finger
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684207/
- ↑ https://emedicine.medscape.com/article/1244693-workup
- ↑ https://my.clevelandclinic.org/health/diseases/7080-trigger-finger--trigger-thumb





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...