This article was co-authored by Robert Dhir, MD. Dr. Robert Dhir is a board certified Urologist, Urological Surgeon, and the Founder of HTX Urology in Houston, Texas. With over 10 years of experience, Dr. Dhir’s expertise includes minimally-invasive treatments for enlarged prostate (UroLift), kidney stone disease, surgical management of urological cancers, and men’s health (erectile dysfunction, low testosterone, and infertility). His practice has been named a Center of Excellence for the UroLift procedure, and is a pioneer in non-surgical procedures for ED using his patented Wave Therapy. He earned his undergraduate and medical degrees from Georgetown University and was awarded honors in pre-medical studies, urology, orthopedics, and ophthalmology. Dr. Dhir served as chief resident during his urological surgical residency at University of Texas at Houston / MD Anderson Cancer Center in addition to completing his internship in general surgery. Dr. Dhir was voted Top Doctor in Urology for 2018 to 2019, one of the top three Best Rated Urologists in 2019 & 2020 for Houston Texas, and Texas Monthly has named him to the 2019 & 2020 Texas Super Doctors Rising Stars list.
There are 17 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 33,885 times.
Male incontinence is a symptom of many other syndromes and conditions and warrants investigation. You could have problems neurologically or with your genitourinary tract or another such disorder. The key to preventing the problem from happening again is to determine what has caused it in the past. Consider if anything new changed in your life, such as a new medication, that could be causing this effect or any added weight that could be placing additional pressure on your bladder. There are some general prevention measures that apply to all healthy individuals, but if you are currently experiencing male incontinence, a visit to your healthcare provider to discuss your symptoms is a great place to start.
Steps
Taking Steps to Prevent Future Incontinence
-
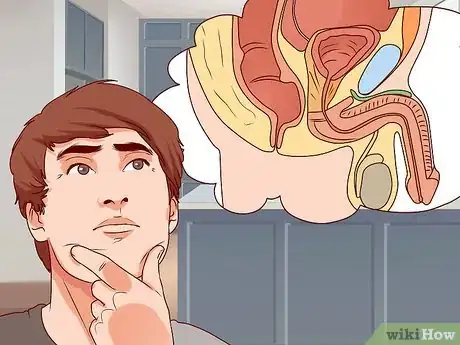
1Identify the forms of incontinence that you can prevent. Many of the underlying causes of incontinence unfortunately cannot be controlled. Benign prostatic hypertrophy, neurological disorders, stroke, prostate/bladder cancer, etc. cannot be prevented.[1] However, you can take steps to minimize your risk of some of these underlying conditions.
-
2Stop smoking. One excellent way to reduce your risk of developing incontinence is to stop smoking. The National Institutes of health reports that up to 50% of bladder cancer cases are caused by smoking. Pressure in the bladder caused by tumors results in incontinence. If you need help quitting, schedule an appointment with your doctor, who can help you quit. There are prescribed medications to help you, and she can also help you find a local support group.[2]Advertisement
-
3Lose weight to prevent incontinence. When you are overweight, extra pressure gets placed on your bladder. This extra pressure on your bladder can lead to incontinence. While losing weight may seem like a daunting task, it will be well worth it in the end. Start exercising more and make an effort to eat healthy foods. Other ways you can lose weight include:
- Making sure that you get the right amount of protein, fruits, vegetables, low-fat dairy, and healthy carbohydrates each day. Your daily intake of each food group will depend on your weight, age, and health. If you should be consuming 2,000 calories a day, you should eat six to eight servings of grains, four to five servings of veggies, four to five servings of fruit, 3 – 6 ounces of protein, two to three servings of low-fat dairy, and two to three servings of fats and oils.
- Developing an exercise routine and sticking to it. Your exercise routine should include cardiovascular training (like running or swimming), weight training (like doing push-ups or lifting weights), and flexibility training (like yoga or stretching).
- Limiting the portions of each meal you have.
- Choosing low-calorie snacks like fruits and vegetables.
-
4Increase zinc in your diet. Research has indicated that men with prostate cancer had 62 – 75% decreased zinc in malignant prostate cells and that zinc plays a role in the progression of prostate cells to malignancy. The recommendation is for zinc supplementation, but amounts are not clear at present. Consult your doctor regarding a healthy amount of zinc supplementation based on the present zinc levels in your diet.[3]
-
5Increase your lycopene intake. Lycopenes are powerful phytonutrients and antioxidants shown to fight cancer. Five of the foods highest in lycopenes per cup include:[4]
- Guava: 8587 uq
- Watermelon: 6889 uq
- Tomatoes: 7298 uq
- Papaya: 2651 uq
- Grapefruit: 2611uq
-
6Eat more soy. Some recent findings have suggested that the isoflavones in soy may help prevent prostate cancer.[5] You can increase the amount of soy in your diet with edamame, soy milk, or tofu.
-
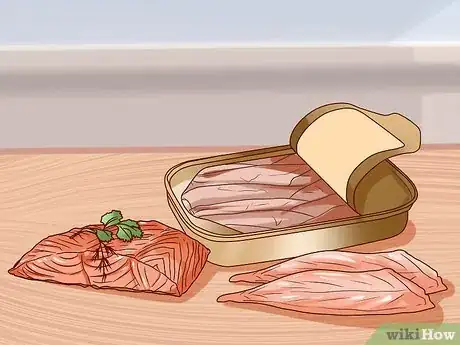
7Add more omega-3 fatty acids to your diet. Omega-3 fatty acids are present in a wide array of fish and seafood options, including salmon, mackerel, sardines, and bass. Studies have shown that omega-3's protect against cancers of the breast, colon, and prostate.[6]
-
8Stay hydrated. Drink at least eight glasses of water during the day to prevent conditions such as urinary tract infection, constipation, and kidney stones that cause incontinence. You should also consider drinking most of your fluids during the day and limiting the amount of fluids you drink in the evening before going to bed.
-
9Practice timed voiding. If you are afraid that you may develop incontinence, you can train your bladder to some degree. Plan particular times during the day to visit the restroom. This is a way to train your bladder, which helps to avoid incontinence.
-
10Avoid incontinence-causing food and drinks. Substances that can lead to incontinence include alcohol, caffeine, acidic foods, spicy foods, and sugar or artificial sweetener.
- Alcohol is a diuretic, an agent that causes your body to lose fluid. It also irritates the bladder, causing incontinence. Try to limit your alcohol intake to one glass per night if at all.
- Caffeine is also a diuretic. Drink caffeinated beverages early in the day if at all.
-
11Try out some Kegel exercises. Kegel exercises are a great way to prevent incontinence because they strengthen the muscles of your pelvic floor. Learning how to do them correctly can be a little tricky because you have to isolate your pelvic muscles. Your pelvic muscles are the muscles you use when you try to stop urinating midstream. You will see or feel your testicles rising when you squeeze your pelvic muscles.[7]
- Once you’ve isolated your pelvic muscles, squeeze them and hold for a count of five and then relax for a count of five. Your goal is to do ten repetitions, three times a day.
-
12Avoid diuretics. A diuretic is a medication that gets rid of extra fluid in the body. This is usually prescribed for patients who have heart conditions. Sadly, it also has a tendency to cause incontinence. There are several different kinds of diuretics: thiazide, loop, potassium-sparing, and quinazoline diuretics. Recognizable diuretic medications include[8] :
- Thiazide diuretics: Clorpres, Tenoretic, Thalitone, Capozide, Dyazide, Hyzaar, Lopressor HCT, Maxzide, and Prinzide.
- Loop diuretics: Lasix and Demadex.
- Potassium-sparing diuretics: Aldactazide, Aldactone, Dyazide, and Maxzide.
- Quinazoline diuretics: Zaroxolyn
- Always consult your doctor before taking yourself off a prescribed medication.
-
13Consider avoiding muscle relaxants. A muscle relaxant is a medication prescribed for certain types of injuries to muscles. It may not come as too much of a surprise that the medications that relax your body also cause incontinence. Recognizable muscle relaxants include:[9]
- Valium, Soma, Flexeril, Skelaxin, and Robaxin.
- Sedatives can also cause incontinence.
-
14Identify antihypertensive drugs that may cause incontinence. An antihypertensive drug is a medication used to lower blood pressure. Antihypertensive drugs can be a combination of different kinds of diuretics. If you are using an antihypertensive drug, ask your doctor about other medications available that do not list incontinence as a side effect. Recognizable antihypertensive drugs include:[10]
- Moduretic, Minizide, Monopril HCT, and Accuretic.
Treating Overflow Incontinence
-
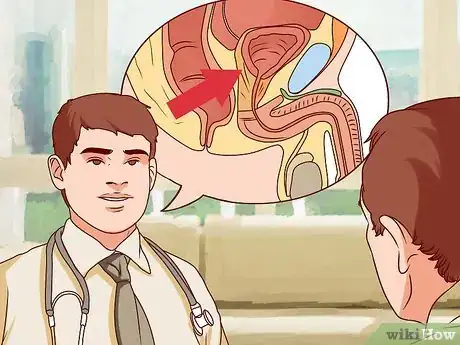
1Look for symptoms of overflow incontinence. Overflow incontinence occurs due to an outlet obstruction that then “overflows” to cause incontinence. Benign prostatic hypertrophy (BPH) is a leading cause because the enlarged prostate pushes against and pinches off the urethra as it passes through the prostate. However, other conditions can also cause the symptoms, which include:[11]
- Increased urinary frequency
- Urinary hesitancy (trouble urinating despite needing to)
- Nocturia (going to the restroom at night a lot)
- Weakened urinary stream
- Recurrent urinary tract infections (UTIs)
- Urinary incontinence
- Occasion urinary retention (cannot urinate at all)
-
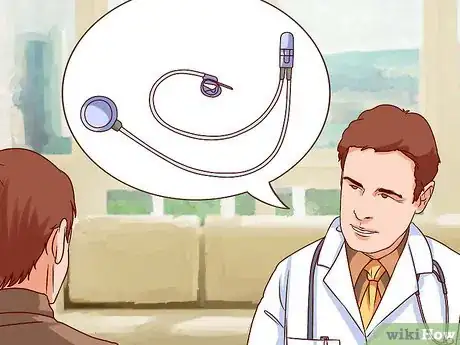
2See your doctor. While BPH is one of the most common causes of overflow incontinence, it’s not the only cause. See your doctor and describe your symptoms in order to help him or her determine the correct diagnosis for your specific condition.[12]
- A tumor in the bladder or prostate can also lead to overflow incontinence, so your doctor will likely perform a screening to rule out these possibilities. Tests will include a prostate-specific antigen (PSA) test of your blood, a digital rectal exam (DTE) to feel for prostate abnormalities, and/or a cystoscopy (a tube inserted into the bladder via the urethra to check for a tumor). If the doctor finds a tumor in any of these instances, he or she will like perform a biopsy to determine whether it is benign or malignant.
-
3Identify medications that can lead to overflow incontinence. During your appointment, your doctor will also ask about any medications you take since some of them can lead to overflow incontinence as a side effect. Diuretics for cardiac problems, sedatives, and muscle relaxants are common medications that can lead to incontinence issues. Some antidepressants, sleeping pills, and high blood pressure medications have also been linked to overflow incontinence.[13]
- Since many of these medications are prescriptions to help with much more serious issues than just incontinence, never stop taking a prescribed medication unless under the guidance of your doctor.
- Though not medications, excess consumption of coffee, tea, alcohol, and vitamins B or C can also lead to overflow incontinence. Your doctor can run a blood panel to test if your diet is too high in B and/or C vitamins.
-
4Ask about medications designed to treat overflow incontinence. For mild-to-moderate BPH symptoms, there are several prescription medications that are available for symptom control such as:[14]
- Alpha blockers such as Hytrin, which does not actually work to shrink the size of the prostate, but will relieve symptoms within a few weeks
- 5-alpha-reductase inhibitors such as Avodart work to reduce the size of the prostate but may not improve symptoms for up to six months
- Cialis, which although originally marketed for erectile dysfunction (ED) improves symptoms of BPH as well
- Your doctor may prescribe a combination of Avodart and Hytrin to have both advantages. This is common, safe, and effective approach to control overflow incontinence.
-
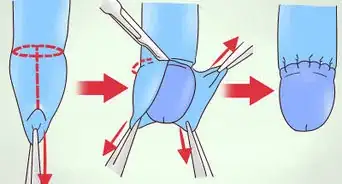
5Consider surgical options for severe symptoms.[15] A transurethral resection of the prostate (TURP) is the go-to procedure for relieving lower urinary tract outlet obstruction due to enlargement of the prostate blocking of the bladder from emptying.This technique uses an endoscope to enter the urethra and clear or ablate the excessive prostate tissue encroaching on the urethra.[16]
Treating Stress Incontinence
-
1Identify symptoms of stress incontinence. Stress incontinence more often relates to leaking urine than some of the more myriad symptoms associated with overflow incontinence. You may notice the leakage when you laugh, cough, sneeze, jog, or lift heavy objects.[19]
-
2Identify causes of stress incontinence. Increased pressure on the bladder due to obesity or pregnancy is the most common cause of stress incontinence. Stress incontinence can also occur due to a lack of bladder sphincter pressure as a result of surgical complications. Surgeries commonly associated with this complication include prostate surgery and transurethral resections of the prostate.[20]
- Stress incontinence can results from 10-20% of TURP surgeries or higher percentages from prostate cancer surgery.[21]
-
3See your doctor. Your doctor will examine your symptoms and run a variety of tests to determine the best course of action for your case. For obese patients, this may include testing for metabolic disorders, such as underlying thyroid conditions, that may have caused the weight gain.[22]
-
4Lose weight. If your doctor concludes that your weight has placed unnecessary pressure on your bladder, he or she will likely suggest that you lose weight as a primary treatment for the condition.
- This will include turning to a healthy, well-balanced diet in conjunction with a regular exercise routine. You can find more information at How to Lose Weight and How to Eat Healthy.
- You may want to consult a dietician and a personal trainer to develop the best, healthiest plan for you in order to lose weight.
-
5Use Kegel exercises. Though known primarily for helping women to improve pelvic floor muscles after pregnancy, men can also perform Kegels to help with stress incontinence. Perform by clenching the muscles that control urination. You may initially have to practice by cutting off your urinary stream midstream to get a good idea of how the clenches should feel when doing them apart from actually urinating.[23]
- Slowly clench while counting to five before using another five count to slowly release. Perform Kegels in sets of ten up to three times per day.[24]
-
6Consider surgical weight loss options. For morbidly obese patients, their physician may recommend lap band or other weight loss surgery options. In one study, 71% of participants who lost 18+ BMI (body mass index) points as a result of gastric bypass surgery had regained urinary continence by one year after the procedure.[25]
Treating Neurogenic Bladder Incontinence
-
1Identify causes of neurogenic bladder incontinence. Urination occurs by a complex arc of nerves communicating with the brain and causing muscles within the bladder and surrounding areas to contract and relax. If you have a neuromuscular disorder—such as multiple sclerosis (MS), for example—you may experience disruptions in these signals, resulting in a neurogenic bladder. People who have had a stroke can also have a resultant neurogenic bladder if the muscles that cause the bladder muscles to contract and relax are affected.
-
2See your doctor. Most of those who have a neurogenic bladder will already be familiar with the underlying causes. However, you should still see your doctor for a positive diagnosis. You doctor will also provide you with the best overview of treatment options and weigh in on which is likely best for your specific situation.
-
3Try physical-psychological therapy options. Also known as timed voiding, physical-psychological therapy combines will power and exercise to help treat the incontinence. This combines Kegel exercises (outlined in the method on stress incontinence) and a voiding diary to help you avoid incontinence episodes before they occur.
- A voiding diary is a daily record of the fluids you’ve taken in, the times and amounts you urinated, and the instances of leakage. You can use this record to help determine the best times to stay close to a bathroom, as well as times when you should force yourself to go, to minimize incontinence episodes.
-
4Discuss medication options with your doctor. Though no drugs currently target the bladder sphincter to help with neurogenic bladder, some drugs do reduce muscle spasms or induce contractions. Your doctor will help determine if one of these classes of medications can help with your specific case.
-
5Discuss surgical options with your doctor. A variety of difference surgical options are available, depending upon the underlying cause for your neurogenic bladder. Your doctor may discuss:
- Electrical-stimulatory therapy, which involves electrodes and a small stimulator implanted to help deliver the signals disrupted by the damaged nerves
- An artificial sphincter, which is a cuff that attaches to the neck of the bladder and works in coordination with an implanted pump and regulating balloon to collect the urine.
Treating an Overactive Bladder
-
1Identify the symptoms of an overactive bladder. An overactive bladder (OAB) is a syndrome which leads to an immediate and unstoppable need to urinate.[26] Common symptoms of the syndrome include:
- Urinary urgency (primary symptom)
- Urgency incontinence (not making it to the toilet quickly enough)
- High urinary frequency and nocturia (getting up at night to go)
-
2See your doctor. Your doctor will help you officially diagnose OAB as the underlying cause. Only 2% of men who suffer from OAB experience regular symptoms of incontinence, so your doctor will want to exhaust other potential causes.
- Your doctor will likely perform a physical exam, as well as ordering urinalysis to test your urine and potentially even a cystoscopy in complicated cases.
- Findings also suggest the overactivity of the detrusor muscle, which is found in the wall of the bladder.
-
3Use timed voiding. Treatment involves behavioral therapy with a timed-voiding regimen. A timed voiding regimen involves going to urinate at set times—for example, every four hours—whether or not you actually feel the need to empty your bladder.
- This is a bladder retraining regimen, and a form of cognitive behavior therapy. Trying to train the bladder to empty at certain times to prevent incontinence.
- A recent report has shown that biofeedback-assisted behavioral therapy (timed voiding) was shown to be superior to pharmacologic therapy with Oxybutynin or placebo in patients receiving treatment for detrusor instability.[27]
- Biofeedback is when a patient is attached to some electrodes that measure their subjective, unconscious physiologic responses. That way they can see in plain sight when their body is having a physiologic response (such as the urge to urinate, and attend to their needs) versus a “false alarm.” This ability to see factual data rather than guessing increases their accuracy of judging their bodies cues.
-
4Ask your doctor about potential medications. There are some pharmacologic interventions, specifically Ditropan, which is dosed as 5 mg twice daily or 5 mg extended release tablet once daily. Combination therapies, using combination of behavioral, pharmacologic, and biofeedback are common.
Expert Q&A
-
QuestionWhat causes severe incontinence?
 Robert Dhir, MDDr. Robert Dhir is a board certified Urologist, Urological Surgeon, and the Founder of HTX Urology in Houston, Texas. With over 10 years of experience, Dr. Dhir’s expertise includes minimally-invasive treatments for enlarged prostate (UroLift), kidney stone disease, surgical management of urological cancers, and men’s health (erectile dysfunction, low testosterone, and infertility). His practice has been named a Center of Excellence for the UroLift procedure, and is a pioneer in non-surgical procedures for ED using his patented Wave Therapy. He earned his undergraduate and medical degrees from Georgetown University and was awarded honors in pre-medical studies, urology, orthopedics, and ophthalmology. Dr. Dhir served as chief resident during his urological surgical residency at University of Texas at Houston / MD Anderson Cancer Center in addition to completing his internship in general surgery. Dr. Dhir was voted Top Doctor in Urology for 2018 to 2019, one of the top three Best Rated Urologists in 2019 & 2020 for Houston Texas, and Texas Monthly has named him to the 2019 & 2020 Texas Super Doctors Rising Stars list.
Robert Dhir, MDDr. Robert Dhir is a board certified Urologist, Urological Surgeon, and the Founder of HTX Urology in Houston, Texas. With over 10 years of experience, Dr. Dhir’s expertise includes minimally-invasive treatments for enlarged prostate (UroLift), kidney stone disease, surgical management of urological cancers, and men’s health (erectile dysfunction, low testosterone, and infertility). His practice has been named a Center of Excellence for the UroLift procedure, and is a pioneer in non-surgical procedures for ED using his patented Wave Therapy. He earned his undergraduate and medical degrees from Georgetown University and was awarded honors in pre-medical studies, urology, orthopedics, and ophthalmology. Dr. Dhir served as chief resident during his urological surgical residency at University of Texas at Houston / MD Anderson Cancer Center in addition to completing his internship in general surgery. Dr. Dhir was voted Top Doctor in Urology for 2018 to 2019, one of the top three Best Rated Urologists in 2019 & 2020 for Houston Texas, and Texas Monthly has named him to the 2019 & 2020 Texas Super Doctors Rising Stars list.
Board Certified Urologist & Urological Surgeon Incontinence can have many causes, but an enlarged prostate is one of the most common ones. I recommend you talk to your doctor to rule out other underlying issues.
Incontinence can have many causes, but an enlarged prostate is one of the most common ones. I recommend you talk to your doctor to rule out other underlying issues.
References
- ↑ Robert Dhir, MD. Board Certified Urologist & Urological Surgeon. Expert Interview. 23 September 2020.
- ↑ http://www.cnn.com/2011/HEALTH/03/21/worse.incontinence.health/index.html
- ↑ Pamela Christudos, R Selvakumar, Joseph, Fleming. Zinc Status in Patients With Benign Prostatic Hyperplasia and Prostatic Carcinoma, Indian Journal of Urology 2011 Jan-March 27 (1) 14-18
- ↑ http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-new-research
- ↑ http://www.cancer.org/cancer/prostatecancer/detailedguide/prostate-cancer-new-research
- ↑ Zhennen, Gu, Janel Suburu, Haigin, Chin et al Mechanism of Action of Omega Poly usaturated Fatty Acids in Prostate Cancer Prevention, Biomedical Resident International 2013 824563 May 23 doi 1155/2013/824563
- ↑ http://www.webmd.com/urinary-incontinence-oab/kegel-exercises-treating-male-urinary-incontinence
- ↑ http://www.webmd.com/hypertension-high-blood-pressure/diuretics-for-high-blood-pressure
- ↑ http://www.webmd.com/back-pain/muscle-relaxants-for-low-back-pain
- ↑ http://www.health.harvard.edu/newsletters/Harvard_Womens_Health_Watch/2009/August/Medications-for-treating-hypertension
- ↑ Jonathan L Edwards MD Diagnosis and Management of Benign Prostatic Hyperplasia American Family Physician, 2008 May 1577 (10) 1403-1410
- ↑ Robert Dhir, MD. Board Certified Urologist & Urological Surgeon. Expert Interview. 23 September 2020.
- ↑ http://www.webmd.com/urinary-incontinence-oab/4-medications-that-cause-or-worsen-incontinence
- ↑ Jonathan L Edwards MD Diagnosis and Management of Benign Prostatic Hyperplasia American Family Physician, 2008 May 1577 (10) 1403-1410
- ↑ Robert Dhir, MD. Board Certified Urologist & Urological Surgeon. Expert Interview. 23 September 2020.
- ↑ Ravi Kacker, Stephen B Williams EndoUrologic Procedures for Benign Prostatic Hyperplasia, Urology Journal71-176.
- ↑ Ravi Kacker, Stephen B Williams EndoUrologic Procedures for Benign Prostatic Hyperplasia, Urology Journal71-176.
- ↑ Ravi Kacker, Stephen B Williams EndoUrologic Procedures for Benign Prostatic Hyperplasia, Urology Journal71-176.
- ↑ http://www.webmd.com/women/tc/kegel-exercises-topic-overview
- ↑ Daniel Elliot, Landon Trost Male Stress Incontinence : A Review of Surgical Treatment Options and Outcomes Advanced Urology 2012 May 8 101155 /2012/287489
- ↑ Daniel Elliot, Landon Trost Male Stress Incontinence : A Review of Surgical Treatment Options and Outcomes Advanced Urology 2012 May 8 101155 /2012/287489
- ↑ Daniel Elliot, Landon Trost Male Stress Incontinence : A Review of Surgical Treatment Options and Outcomes Advanced Urology 2012 May 8 101155 /2012/287489
- ↑ http://www.webmd.com/urinary-incontinence-oab/kegel-exercises-treating-male-urinary-incontinence
- ↑ http://www.webmd.com/urinary-incontinence-oab/kegel-exercises-treating-male-urinary-incontinence
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/17978117
- ↑ http://emedicine.medscape.com/article/459340-overview
- ↑ Cardozo, LD, Biofeedback in Overactive Bladder, Urology 2005, May 55( 5A Supp) 24-28 Dis.


















































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...