This article was medically reviewed by Lacy Windham, MD. Lacy Windham, MD, is a Board-Certified Obstetrician & Gynecologist in Cleveland, Tennessee. Dr. Windham attended medical school at the University of Tennessee Health Science Center in Memphis. Her residency was completed at Eastern Virginia Medical School in Norfolk, Virginia. She was the recipient of multiple awards during her residency training, including Most Outstanding Resident in Maternal Fetal Medicine, Most Outstanding Resident in Oncology, Most Outstanding Resident Overall, and Special Award in Minimally Invasive Surgery.
There are 11 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 686,970 times.
Irregular spotting, also referred to as breakthrough bleeding, is normal for the first few months after starting a new prescription for birth control pills. The spotting usually involves only a small amount of blood and often does not require the use of a feminine hygiene product, such as a pad or tampon. If the problem persists, talk to your doctor.
Steps
Taking Your Pills Properly
-
1Expect spotting for the first few months. Spotting frequently occurs for the first three to four months after starting birth control pills for the first time. This is also the case if you have been on birth control pills in the past, took a break, and now have restarted this form of birth control, and in cases where you have changed the brand or type of birth control pills you are taking.[1]
- The clinical use of the term “spotting” refers to episodes of slight bleeding that do not require the use of a pad or tampon.
- The term “breakthrough bleeding” commonly indicates a level of bleeding that requires the use of a product.
- However, these terms can be misleading since they are often used interchangeably, even in the medical literature.
-
2Take your pills at the same time. Develop a schedule that works for you to help regulate your cycle. Consistently taking birth control pills at the same time each day reduces the incidence of spotting.[2]
- Altering the time by a few hours is generally okay, but if you alter your dose by four hours or more, then you are altering how your body absorbs the birth control pills and naturally produces hormones.
- This may lead to spotting. It may also decrease the effectiveness of the birth control pills, which can increase your short-term chances of getting pregnant.
- Pick a time that is convenient and that is the most likely to time you will remember. Try taking them last thing before bed, in the morning when you brush your teeth, or at another time when you consistently perform other daily activities like taking your shower or going for your morning walk.
- If you don’t like the time you picked and want to adjust, wait until you start the next new pack. Adjust your scheduled dose time with a fresh pack to be sure you do not compromise the way the pills work in your body. Adjusting your time mid-cycle can increase your chance of spotting as well as getting pregnant.
Advertisement -
3Keep your pills in their original container. Do not pop out the tablets or remove them from their original package or container. The packaging is designed to help you keep track of where you are in your cycle.[3]
- If your pack contains pills that are different in color, it is especially important to take them in the exact order as they are in the package.
- Colored tablets contain different strengths of hormones to provide the amount of hormones your body needs at different times of the month.
- Even if your pills are all the same color, take them in the order they are in the package. This can help you and your doctor identify any problems you may have, such as spotting, at a particular part of your cycle.
-
4Be prepared in case you miss a pill. Talk with your doctor in advance to be sure you know what to do if you miss a pill. Missing a pill is a common reason for spotting or breakthrough bleeding to occur.[4]
- If you miss a pill, ask your doctor when to take the missed dose and if added protection is needed to prevent pregnancy.
- However, these questions do not have simple answers. The answers vary depending on three primary factors. The factors include the type of pills you are taking, where you are in your cycle when you miss the pill, and if you missed more than one pill in a row.
-
5Review the general guidelines for missing one pill. Always check with your doctor to be sure you know what to do if you miss a pill. General guidelines that are used for women that take a new pack of pills every month, as opposed to packs that are designed for three month cycles, include the following:[5]
- If you miss the very first pill in a new pack, take the missed pill as soon as you remember and take the next pill at the normal time. It is okay to take two pills in one day. Use a backup form of birth control until you have taken the next seven tablets on schedule.
- If you miss a pill during the cycle, take it as soon as you remember. Take the next pill at the normal time. It is okay to two pills in one day.
- If you have a 28 day pill pack, and you miss a dose during the last week, or tablets 21 thru 28, then you are not at risk of getting pregnant. Start your new pack as you would according to your regular schedule.
-
6Follow the recommendations if you miss more than one pill. Every manufacturer provides additional information in their product literature to help guide you if you miss more than one pill during a cycle. You can also check with your doctor to be sure you understand what to do. Be aware that you will likely need to use another method of birth control until you get back on schedule with your pills.[6]
- If you miss two pills in a row during the first or second week, take two tablets on the day you remember and two tablets the following day. This will put you back on your normal schedule. Use another form of birth control until you begin new cycle and a fresh pack of pills.
- If you miss two pills in a row during the third week, then use another method of birth control until it is time to start a new pack. You can discard the remainder of the pack you were in when you missed the two pills in the latter part of your cycle.
- If you miss three or more pills in a row anytime during the cycle, then you should use another method of birth control and you will need to start a new pack.
- Contact your doctor for clear instructions as to when to start the new pack. In some cases you may need to wait until your menstrual cycle occurs and start the new pack as you normally would. Your doctor may want you to start another pack sooner than that, depending on the type of birth control pills you are taking and how long until your menstrual cycle would normally begin.
- Be sure to use other forms of birth control until you have taken seven days of your new pack.
Adjusting Your Lifestyle
-
1Quit smoking. If you don’t smoke, then don’t start. Smoking cigarettes is a risk factor for developing serious problems when combined with birth control pills. Smoking can increase your metabolism of estrogen, resulting in lower levels of estrogen and possibly lead to spotting.[7]
- Women who smoke more than 15 cigarettes a day and are over 35 years old should not take birth control.
- Smoking cigarettes while taking birth control pills has been proven to greatly increase the risk of serious side effects.
- Some examples of the serious complications that can occur from smoking and taking birth control pills include blood clots, liver tumors, and stroke.
-
2Maintain a healthy weight. Weight gain or weight loss can affect your body's natural hormonal balance. If you experience significant weight change, check with your doctor to be sure your birth control pill regimen is still appropriate for you.[8]
- Recent research has shown that birth control pills are equally effective in women that are overweight as they are in women of average weight.
- There are still questions about significant changes in weight, either weight gain or loss, and how that may alter the body’s general metabolism, normal production of hormones, and the effects on birth control pill absorption and metabolism.
-
3Beware of vitamins and supplements. Research has shown that some vitamins and herbal supplements influence the effectiveness of birth control pills. Some published remedies for spotting include taking vitamins or other supplements to alter the levels of hormones to prevent spotting.
- While it is true that some vitamins, supplements, and even foods, can interfere with the way your body absorbs the hormones in birth control pills, this is not a recommended method of trying to self-adjust your dose.
- Consult your doctor before you use vitamins, supplements, and some foods and beverages to try to alter your absorption of your birth control pills.
- These methods are not established in scientific research and are not recommended. There are many well-researched options available to balance the hormones in the birth control pills to match the needs of your body.
- Some examples of vitamins, herbal supplements, and foods that alter the absorption of the hormones in birth control pills include vitamin C, St. John’s Wort, and grapefruit juice. If these agents are part of your regular routine, let your doctor know.
-
4Control the stress in your life. Stressful situations cause your body to alter the release and absorption of the stress hormone called cortisol. Cortisol can alter the normal production of natural hormones, and may have an impact on the absorption and efficacy of your birth control pills.[9]
- Alterations in cortisol levels influence how your body uses available hormones. This can lead to abnormalities in your menstrual cycle and may include spotting and breakthrough bleeding even when taking birth control pills.
- Take steps to consistently manage the stress in your life. This may include participating in a new exercise routine or learning stress management tools such as yoga, meditation, and mindfulness exercises.
- Learn how to use breathing and relaxation techniques to control unexpected stressful circumstances.
Seeking Medical Attention
-
1Contact your doctor if you have persistent spotting. If you experience spotting or breakthrough bleeding for an extended amount of time, schedule an appointment with your doctor. Your doctor needs to know if you have spotting or breakthrough bleeding for more than seven days of your cycle. In addition, spotting or bleeding that persists for more than four months warrants medical attention.[10]
- See your doctor for new episodes of spotting. The spotting or breakthrough bleeding may be caused by something unrelated to your birth control pills.
- If you are continuing on the same regimen of birth control pills but begin to experience mid-cycle bleeding, this may be a symptom of another problem and should be evaluated by your doctor.
- Breakthrough bleeding may be a sign of other problems including pregnancy or conditions involving cervical changes. If you have made lifestyle changes such as smoking, or have started taking new medications that may be interacting with the birth control pill regimen, this can cause breakthrough bleeding as well.
-
2Consider another type of birth control pill. Many birth control pills are made to contain the lowest possible amounts of some hormones. Your doctor may change your pills to a type that contains slightly higher levels of estrogen if he or she is aware of your ongoing problem with spotting. Changing to a pill formulated with a different type of progesterone, such as levonorgestrel, may also help.[11]
- If you continue to have problems with spotting or breakthrough bleeding on your current pill, talk to your doctor about either switching to another strength or extending the number of days you take active pills vs the placebo pills at the end of most packs.
- There are many types of pills that are effective at preventing pregnancy. Finding the best one to suit the hormonal needs of your body is simply a matter of being patient and trying a few different types.
- Doctors routinely start with products that contain the lowest possible amounts of either estrogen, progesterone, or both. Changing to a brand with a slightly higher dose of estrogen usually stops the problem with spotting and breakthrough bleeding.
- Some packages are now designed to extend your days of active pills by taking advantage of a 3 month cycle as opposed to the usual 1 month pill pack.
- By switching to a 3 month cycle, you may have less trouble with your periods and fewer problems with spotting and breakthrough bleeding. Talk to your doctor about this option.
-
3Work with your doctor. Many women stop taking their birth control pills out of frustration due to continued problems with spotting or breakthrough bleeding.
- Consider being patient and open to trying other types of birth control pills.
- Realize that stopping your birth control pills means you will need to find another method of birth control.
- Birth control pills are one of the most effective and convenient ways to prevent pregnancy.
- Other methods are often less reliable, inconvenient, and sometimes require interruptions during sexual intercourse.
-
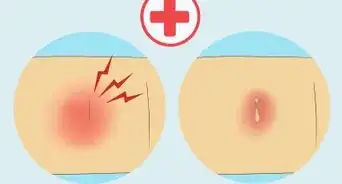
4Get regular pap smears and cervical exams. Your doctor will schedule your appointments at intervals felt to be most appropriate for your age and any risk factors you may have for other diseases. Many doctors may recommend scheduling your appointments on an annual basis to evaluate for changes and be sure your prescription birth control pills are at the best dose for you.[12]
- If you are having any problems with new or persistent bleeding, make an appointment as soon as possible for an evaluation.
- Vaginal bleeding can be a symptom of a medical condition, including some that are serious such as cervical cancer.
- In addition, your doctor may want to perform screening tests for sexually transmitted disease or other problems on a routine basis, possibly annually, depending on your personal circumstances.
- Birth control pills do not protect from sexually transmitted diseases. Let your doctor know as soon as possible if you think you may have acquired a sexually transmitted disease.
-
5Talk your doctor about any other your medications you are taking. Many drugs can interfere with the effectiveness of your birth control pills. Be sure your doctor has a list of all your medications. Continually update him or her on any changes that are made to your regular daily doses of prescription drugs, over-the-counter agents including aspirin and nonsteroidal anti-inflammatory drugs like naproxen and ibuprofen, vitamins, and herbal supplements.[13]
- Drugs that can interfere with the effectiveness of your pill can include everything from over-the-counter herbal supplements to antibiotics.
- Both short and longer term use of some antibiotics can alter the effectiveness of your birth control pills. If you are prescribed an antibiotic for any reason, it is important to let your doctor know since your birth control regimen may be less effective.
- Some antiseizure medications can also interfere with the effectiveness of your birth control pills. Seizure medications are sometimes used to treat mood disorders and chronic pain syndromes such as migraine headaches.
- Some herbal supplements, especially St. John's wort, may also interfere with hormonal birth control.
- Always ask your doctor or pharmacist about the need to use backup birth control when you are taking something new.
-
6Inform your doctor of any new or existing medical conditions. Medical conditions can alter the way birth control pills work in your body and may put you at additional risk of unwanted complications.[14]
- Some medical conditions may warrant closer monitoring for women that are taking birth control pills. Examples include diabetes, a history of cardiovascular disease, and a history of breast disease.
- If you get a virus, the flu, or a stomach condition that includes nausea, vomiting, and diarrhea, let your doctor know.
- The symptoms alone can alter the absorption of your birth control pills. This means they are probably less effective during this time and you may need to use another method of birth control until you are feeling better for at least seven days.
References
- ↑ https://www.rch.org.au/kidsinfo/fact_sheets/Oral_contraceptives_skipping_periods_when_taking_the_Pill/
- ↑ http://goaskalice.columbia.edu/answered-questions/taking-birth-control-pills-—-what-counts-same-time-every-day
- ↑ https://www.plannedparenthood.org/learn/birth-control/birth-control-pill/how-do-i-use-the-birth-control-pill
- ↑ https://www.plannedparenthood.org/learn/birth-control/birth-control-pill/how-do-i-use-the-birth-control-pill
- ↑ https://health.clevelandclinic.org/what-happens-when-you-skip-a-birth-control-pill/
- ↑ https://health.clevelandclinic.org/what-happens-when-you-skip-a-birth-control-pill/
- ↑ https://www.aafp.org/afp/2010/0915/p621.html
- ↑ http://abcnews.go.com/Health/Wellness/obesity-barrier-effect-pill/story?id=11429138
- ↑ https://www.apa.org/topics/stress/body
- ↑ https://www.rch.org.au/kidsinfo/fact_sheets/Oral_contraceptives_skipping_periods_when_taking_the_Pill/
- ↑ https://www.acog.org/womens-health/experts-and-stories/the-latest/what-you-should-know-about-breakthrough-bleeding-with-birth-control
- ↑ https://www.nhs.uk/common-health-questions/womens-health/what-causes-bleeding-between-periods/
- ↑ https://www.nhs.uk/conditions/contraception/contraceptive-pill-interact-medicines/
- ↑ https://patient.info/sexual-health/hormone-pills-patches-and-rings/combined-oral-contraceptive-coc-pill#nav-5
About This Article
Spotting is quite common for the first few months after starting birth control pills or after a break. If you’re spotting after 4 months, it might be a result of your schedule. It’s important to always take your pills at the same time each day, since missing a pill or taking it too late can lead to spotting. Try setting an alarm in your phone to remind you. If you’re sticking to your schedule but still spotting, it might be a result of too much stress in your life, which is upsetting your hormone balance. Try exercising, meditating, or doing other mindfulness exercises regularly to reduce stress. If your spotting still doesn’t go away, visit your doctor. They might offer you another type of birth control pill or switch you to a 3-month cycle. For more tips from our Medical co-author, including how to safely change the time you take your pill each day, read on.







































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...