This article was medically reviewed by Siddharth Tambar, MD. Dr. Siddharth Tambar, MD is a board certified rheumatologist at Chicago Arthritis and Regenerative Medicine in Chicago, Illinois. With over 19 years of experience, Dr. Tambar specializes in Regenerative Medicine and Rheumatology, with a focus on platelet rich plasma and bone marrow derived stem cell treatments for arthritis, tendinitis, injuries, and back pain. Dr. Tambar holds a BA in Economics from State University of New York at Buffalo. He earned his MD from State University of New York at Syracuse. He completed his Internship, Residency in Internal Medicine, and his Rheumatology Fellowship at Northwestern Memorial Hospital. Dr Tambar is board certified in both rheumatology and internal medicine. He also holds Musculoskeletal Ultrasound Diagnostic and Interventional certifications from the American College of Rheumatology and the American Institute of Ultrasound in Medicine.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 22,404 times.
Gout is a type of arthritis that is quite common and painful. Fortunately, if your fingers swell or grow tender due to gout, there are ways to relieve the pain. Work with your doctor to alternate over-the-counter and prescription medications to reduce any inflammation.[1] Applying ice packs to your fingers can also provide immediate relief. Reducing or eliminating uric acid-rich foods, such as red meat, in your diet can help, too.[2]
Steps
Reducing Gout Pain with Medication
-
1Develop a pain medication dosing schedule with your doctor.[3] Instead of just taking the standard dosage of pain medication, your doctor may suggest that you use higher doses for a sudden onset attack. If you take a consistent lower-dose pain medication as well, you’ll be covered for both acute and daily episodes.[4]
- Don’t try this method without getting your doctor’s approval first. Taking high doses of pain medication can impact the health of your liver or stomach.
- Start taking medicine with 24 hours of an attack. Do not stop taking the medication during the attack.
- Ask your doctor if any of your other medications might affect your serum uric acid levels. If so, make sure that you do not stop or change your dose during an attack.
-
2Take an over-the-counter pain medication. Either naproxen sodium (Aleve) or ibuprofen (Motrin, Advil) can help to reduce the inflammation and swelling within your hand and fingers.[5] Read the label carefully and take the medication as soon as you start to feel the gout pain. Continue using the medication until the pain reduces or you take with your doctor about other options.[6]
- Both naproxen sodium and ibuprofen are nonsteroidal anti-inflammatory drugs (NSAIDs). If your pain is severe or regular, your doctor may suggest a prescription NSAID, such as celecoxib (Celebrex).
Advertisement -
3Ask your doctor if colchicine might work for you. Colchicine is taken with an NSAID during a gout attack. If you have an acute attack, your doctor will prescribe a large dose to be taken during the attack. If you experience chronic attacks, you may take a smaller, daily dose to reduce inflammation.[7]
- Tell your doctor if you have kidney disease or if you are taking other medications before using colchicine.
-
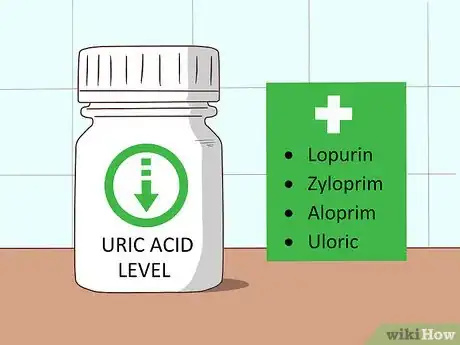
4Use a medication that lowers uric acid production for frequent attacks.[8] Xanthine oxidase inhibitor (XOI) drugs can help to reduce your body’s uric acid levels, which can reduce the severity and frequency of your attacks. You’ll usually need to take these medications daily. It’s possible that any other gout symptoms that you are experiencing may be reduced as well.[9]
- Lopurin, Zyloprim, Aloprim, and Uloric are all frequently prescribed XOI medications.
- Contact your doctor if you develop a rash or feel nauseous, as these are possible XOI medication side effects.
-
5Get a corticosteroid injection if pain medication doesn’t work for you. If you have a bad reaction to NSAIDs, then your doctor might suggest using corticosteroids to lessen the inflammation in your joints. Your doctor will either give you pills to take in the event of a gout attack or you can come into their office for a shot.[10]
- Corticosteroids can cause side effects, including elevated blood pressure.
- During severe attacks, your doctor may combine corticosteroids with colchicine.
Responding Immediately to Pain
-
1Eat 20-30 cherries as soon as you feel an attack developing. There is some evidence showing that the nutrients in cherries can reduce uric acid levels in your body. For best results, eat fresh cherries, but frozen or canned ones are okay, too. You can also drink 2-3 sips of concentrated black cherry juice (often sold in natural groceries).[11]
- To help prevent future attacks, continue to eat 6-10 cherries each day.
-
2Apply an ice pack to your finger for 20-30 minutes. Get an ice pack or bag of frozen vegetables and wrap it in a washcloth.[12] Then, place the washcloth on your hand and fingers. Keep applying the cold for half-an-hour or until your finger feels better. Repeat this process every few hours throughout the day to reduce any swelling.[13]
- If you don’t have the materials for an ice pack, simply holding your injured finger under cold running water can provide some relief.
- Wrapping the pack or vegetable bag in a cloth prevents your skin from being burned by the cold.
-
3Keep your finger elevated until the pain lessens. Prop your hand and arm up on a few pillows, so that your finger stays in a position higher than your heart. This balances out the blood flow to your finger and can help to reduce swelling.[14]
-
4Sip herbal tea during an attack. Boil some water in a kettle and add 2 tablespoons (16 grams) of dried tea herb. Peppermint, rose hip, and yarrow are all particularly effective at reducing inflammation and minimizing pain. Let the tea steep for 10-20 minutes. Pass the tea through a strainer before drinking.[15]
-
5Contact your doctor within 24 hours of the onset of pain. If you are in severe pain, your doctor might suggest that you come in for a corticosteroid injection. Or, they may call in a new or higher dose pain medication prescription. If you haven’t been diagnosed with gout, this is a good time to come into your doctor’s office for testing.[16]
- It’s important to reach out to your doctor as soon as you notice your finger pain, as quick action can shorten the duration of an attack.
Minimizing Potential Gout Attacks
-
1Protect your fingers from injury as much as possible. Finger jams or other injuries can prompt the onset of a painful gout attack. Your body responds to the injury by inflaming the area and simply doesn’t know how to stop. If you have a history of gout attacks, use caution when participating in sports or other physical activities. Wear protective gloves when performing home improvement projects.[17]
- Gout attacks prompted by an injury can last for weeks, especially if you don’t reach out to your doctor for help early on.
-
2Drink 5-6 glasses of water each day. Substitute sugary beverages for water with a slice of fruit. Carry around a refillable water bottle and sip from it throughout the day. Staying hydrated can reduce the uric acid level circulating in your body. Any excess acid will be removed from your body when you urinate, keeping your body more balanced.[18]
- It’s also important to avoid drinking alcohol, such as beer, if you are prone to gout attack. Alcohol can boost your purine levels.
- Avoid drinks that are high in high-fructose corn syrup, such as sodas, some juices, and sports drinks.
-
3Lower your stress levels by doing activities that you enjoy. High stress levels can contribute to the severity and frequency of gout attacks. If you are feeling stressed, go for a walk in your neighborhood or take a yoga class. Take a relaxing bath or go see a movie. Do whatever you know helps you to relax and stay calm.[19]
- Stress can cause you to gain weight, and being overweight may be a contributing factor to gout.
-
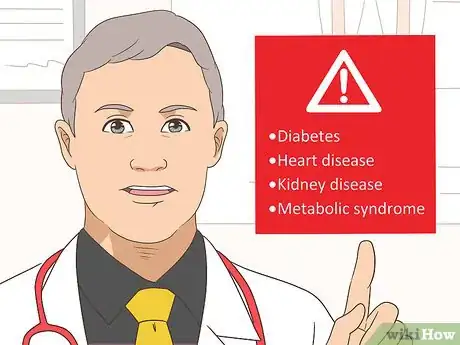
4Work with your doctor to treat any underlying medical conditions. If you are suffering from diabetes, heart disease, kidney disease, or metabolic syndrome, develop a treatment plan with your doctor. If these illnesses go untreated, then they can increase your odds of suffering from gout attacks.[20]
- You will also want to work with your doctor to ensure that any medications that you take for your gout do not interact with other medications that you are currently on.
-
5Avoid eating foods with high purine levels. A purine is a compound found in may processed foods that can increase your chances of a gout attack. Minimize your intake of red meats, seafood (especially sardines and shellfish), fruit juice, salt, and sugar, as they contain high purine levels as well.[21]
- Replace packaged foods, such as sugar-heavy crackers, with healthy options, such as fresh fruit.
- Organ meats, such as liver, also are considered high-purine foods.
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionHow can I relieve gout symptoms at home?
 Siddharth Tambar, MDDr. Siddharth Tambar, MD is a board certified rheumatologist at Chicago Arthritis and Regenerative Medicine in Chicago, Illinois. With over 19 years of experience, Dr. Tambar specializes in Regenerative Medicine and Rheumatology, with a focus on platelet rich plasma and bone marrow derived stem cell treatments for arthritis, tendinitis, injuries, and back pain. Dr. Tambar holds a BA in Economics from State University of New York at Buffalo. He earned his MD from State University of New York at Syracuse. He completed his Internship, Residency in Internal Medicine, and his Rheumatology Fellowship at Northwestern Memorial Hospital. Dr Tambar is board certified in both rheumatology and internal medicine. He also holds Musculoskeletal Ultrasound Diagnostic and Interventional certifications from the American College of Rheumatology and the American Institute of Ultrasound in Medicine.
Siddharth Tambar, MDDr. Siddharth Tambar, MD is a board certified rheumatologist at Chicago Arthritis and Regenerative Medicine in Chicago, Illinois. With over 19 years of experience, Dr. Tambar specializes in Regenerative Medicine and Rheumatology, with a focus on platelet rich plasma and bone marrow derived stem cell treatments for arthritis, tendinitis, injuries, and back pain. Dr. Tambar holds a BA in Economics from State University of New York at Buffalo. He earned his MD from State University of New York at Syracuse. He completed his Internship, Residency in Internal Medicine, and his Rheumatology Fellowship at Northwestern Memorial Hospital. Dr Tambar is board certified in both rheumatology and internal medicine. He also holds Musculoskeletal Ultrasound Diagnostic and Interventional certifications from the American College of Rheumatology and the American Institute of Ultrasound in Medicine.
Board Certified Rheumatologist Gout generally requires actual medical intervention. When someone is having an extreme flare up, it is caused by uric acid crystals, which are needle-like crystals that cause severe inflammation. At that point, anything that can help reduce pain and swelling will help. This includes ice, resting the joint that's been affected, and anti-inflammatory medication in the short term.
Gout generally requires actual medical intervention. When someone is having an extreme flare up, it is caused by uric acid crystals, which are needle-like crystals that cause severe inflammation. At that point, anything that can help reduce pain and swelling will help. This includes ice, resting the joint that's been affected, and anti-inflammatory medication in the short term.
Warnings
- It’s important to treat your gout quickly, as repeated attacks can wear down your finger tendons. This can even lead to loss of use.[22]⧼thumbs_response⧽
References
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://www.arthritis.org/health-wellness/healthy-living/nutrition/healthy-eating/which-foods-are-safe-for-gout
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ https://www.hopkinsarthritis.org/arthritis-info/gout/gout-treatment/
- ↑ https://www.prevention.com/health/18-ways-to-treat-gout
- ↑ Siddharth Tambar, MD. Board Certified Rheumatologist. Expert Interview. 25 August 2020.
- ↑ https://www.arthritis.org/about-arthritis/types/gout/articles/how-to-stop-a-gout-attack.php
- ↑ https://www.arthritis.org/about-arthritis/types/gout/articles/how-to-stop-a-gout-attack.php
- ↑ https://www.prevention.com/health/18-ways-to-treat-gout
- ↑ https://www.arthritis.org/about-arthritis/types/gout/articles/how-to-stop-a-gout-attack.php
- ↑ http://www.health.com/health/gallery/0,,20458446,00.html#family-history-5
- ↑ https://my.clevelandclinic.org/health/diseases/4755-gout
- ↑ https://www.arthritis.org/about-arthritis/types/gout/articles/how-to-stop-a-gout-attack.php
- ↑ https://www.nhs.uk/conditions/gout/
- ↑ https://www.arthritis.org/about-arthritis/types/gout/self-care.php
- ↑ http://www.assh.org/handcare/hand-arm-conditions/Gout-and-Pseudogout




































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...