This article was medically reviewed by Farah Khan, MD and by wikiHow staff writer, Christopher M. Osborne, PhD. Dr. Farah Khan is a Board Certified Allergist and Immunologist who graduated from fellowship in 2020. She specializes in asthma, food allergy, skin conditions, and rhinosinusitis care, and treats both adult and pediatric patients. Dr. Khan holds an MD from Ross University School of Medicine. She completed her Pediatric Residency training at INOVA Children's Hospital and her fellowship at Virginia Commonwealth University. Dr. Khan is an active member of the American Academy of Allergy, Asthma and Immunology as well as the Clinical Immunology Society.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 7,083 times.
The little red bumps on your skin known as hives can be unsightly, uncomfortable, and really itchy! You can treat this allergic reaction in a variety of ways, however, and often significantly reduce the itching sensation. Quick home remedies like a cool compress or a baking soda paste may provide short-term relief, and making simple lifestyle changes like wearing loose clothes and staying out of the sun can also cut down on the itching. For longer-term relief, though, your best bet is to work with your doctor to find the best medication options for your condition.
Steps
Trying Home Remedies
-
1Hold a cool washcloth or wrapped ice pack over your hives. Soak a washcloth in cold water, wring it out, and apply it to the affected area. Alternatively, wrap an ice pack or a zip-close bag of ice in a soft kitchen towel and apply it. In either case, apply the cooling cloth for up to 15 minutes per hour as needed.[1]
- Cool moisture helps to dull pain receptors and soothe dry, itchy skin.
- These remedies can provide noticeable short-term relief, but won’t help with long-term management of itching due to hives.
-
2Cover the area with a wet dressing soaked in aluminum acetate solution. Aluminum acetate solution, also known as Burow’s solution, can help relieve itching and irritation from hives.[2] Soak a washcloth or gauze pad in the solution and squeeze out the extra liquid, then let it sit on your irritated skin for 20-30 minutes, 4-6 times a day, or as often as your doctor or pharmacist recommends.
- If the area is severely irritated, you may need to rewet the cloth a few times to keep it moist enough.
- You can buy aluminum acetate solution over the counter as Burow’s Solution, Domeboro, or Star-Otic.
Advertisement -
3Apply an alkaline substance like calamine lotion or milk of magnesia. Calamine lotion is an alkaline mixture that may provide relief from itching for a few hours. However, in some cases it may make hives worse, so avoid using it if this is the case for you. Also, dab it on no more than 3-4 times per day or as directed by your doctor.[3]
- Both milk of magnesia and Pepto-Bismol (bismuth subsalicylate) are also alkaline substances that may provide similar anti-itch relief. As with calamine lotion, however, they may worsen itchy hives in some cases.
- Whichever alkaline substance you use, wash it away with cool water and a soft cloth once it begins to dry out and flake off.
-
4Make an anti-itch paste out of baking soda or cream of tartar. Add a heaping spoonful of baking soda or cream of tartar to a bowl, then add just enough water to create a paste that’s roughly the consistency of white toothpaste. Spread it over your hives and leave it there until it dries out and starts to flake off. Repeat this up to 4 times per day, or more often if your doctor recommends it.[4]
- Both baking soda and cream of tartar are alkaline substances that may potentially reduce itching in the short term.
- Don’t rub the paste firmly onto your skin, as the grittiness may cause additional irritation.
- Don’t apply the paste if you have any open wounds in the area.
-
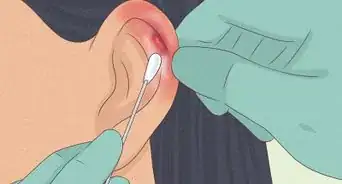
5Combine vinegar and water and apply it with a cotton ball. Mix 3 parts of water with 1 part of vinegar in a small bowl—for instance, 15 ml (0.51 fl oz) of water and 5 ml (0.17 fl oz) of vinegar. Dip a cotton ball or cotton swab into the mixture and dab it gently over your hives. You may experience temporary itch relief due to vinegar’s antibacterial properties.[5]
- While apple cider vinegar has become a home remedy “cure all,” any type of vinegar should work the same here.
- In some cases, vinegar may cause additional irritation. Stop using it if it does!
-
6Take an oatmeal bath if you have widespread hives or itching. Finely ground (or colloidal) oatmeal is great for soothing and moisturizing itchy, irritated skin.[6] If you have hives all over, draw a cool or lukewarm bath and sprinkle in some Aveeno or another oatmeal-based bath soak. Soak in the bath for 10-15 minutes or the amount of time recommended on the package.
- You can also make your own oatmeal soak by grinding up uncooked, rolled oats in a coffee grinder or food processor. Grind the oats until they’re fine enough to quickly dissolve in water.
-
7Create a pineapple compress to soothe itchy hives. Pour a small can of crushed pineapple—or crush some fresh pineapple pieces—into a bowl lined with a thin cotton cloth. Pull up the corners of the cloth and tie them off with a string or rubber band, then place the compress on your hives for up to 15 minutes. Store the compress in the fridge for up to 24 hours and use it as often as needed during this time.
- Pineapple contains bromelain, an enzyme which may reduce itching and swelling.
- Eating pineapple may also help, or you can try bromelain supplements.
-
8Don’t scratch at your itchy hives![7] This may seem like the fastest and easiest “home remedy” for itchy hives, but it can easily cause more harm than good. Scratching will increase your skin irritation and make it more itchy and painful soon after you stop. Even worse, you may break the skin and cause an infection.[8]
- If you experience signs of infection like increased redness or swelling, oozing, a foul odor, or a fever, contact your medical provider right away.
Making Lifestyle Changes
-
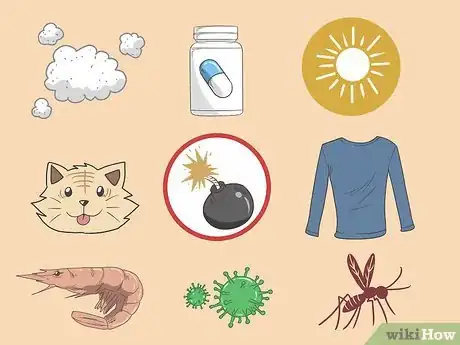
1Attempt, when possible, to identify and avoid your triggers.[9] While many cases of hives occur without any clear cause, others can be traced to a specific trigger. Whenever you experience hives, see if you can identify any recurring triggers—if you do, see if reducing or eliminating your exposure relieves your hives. Common triggers include (but aren’t limited to):[10]
- Airborne allergens like dust, dander, and pollen.
- Allergies to certain foods, medications, pets, and so on.
- Environmental stimuli, such as exposure to sunlight, heat, or (less commonly) cold.
- Contact pressure on your skin, such as from tight clothing or a purse strap.
- Viral, fungal, or bacterial infections.
- Insect bites.
-
2Take a cool shower or bath no more than once per day. Unless your hives are triggered by exposure to cold—which is uncommon—taking a cool bath or shower every day may provide short-term relief from itching. Try lukewarm or warm water if cool water triggers your hives.[11]
- Don’t shower or bathe more than once per day. Otherwise, you may further dry out your skin and make your hives even more itchy and uncomfortable.
- When taking a bath, try stirring in a scoopful of baking soda or finely-ground colloidal oatmeal while the water is running. Soaking in the tub for up to 30 minutes may provide additional itch relief.
-
3Wash with a gentle soap and apply a fragrance-free moisturizer as needed. Don’t use harsh cleansers or scented soaps when bathing, showering, or washing up, as these may further irritate your skin. Instead, use a mild skin cleanser and a soft cloth. After you dry off gently with a soft towel, apply a fragrance-free moisturizer to help your skin stay hydrated.[12]
- Consult your primary care doctor, dermatologist, or pharmacist for moisturizer recommendations based on your particular condition.
- Be extra gentle when cleaning, drying, and moisturizing areas in which you have hives. Change cleansers and/or moisturizers if they seem to make your hives worse.
-
4Wear loose, soft clothing, especially in the area of your hives. Wearing rough or tight clothing will almost certainly make your hives more itchy, and may be a trigger for your hives in the first place. Opt for breathable fabrics like cotton and wear clothing that does not rub against your itchy hives.[13]
- Hives can sometimes occur in an area where a purse strap, waistband, or bra strap presses and rubs against your skin. Adjusting your wardrobe may make a big difference in this case.
-
5Find healthy ways to reduce stress in your life. Dealing with itchy hives can be stressful! Unfortunately, excessive stress can sometimes trigger hives, and it can also worsen hives caused by other known or unknown triggers. But, by using healthy stress-fighting techniques like the following, you may be able to reduce the itchiness and irritation caused by your hives:[14]
- Meditation, prayer, or mindfulness techniques.
- Deep breathing exercises.
- Yoga or tai chi.
- Light- or moderate-intensity cardiovascular exercise.
- Listening to relaxing music or reading a calming book.
- Getting a good night’s sleep.
- Talking to a friend or loved one.
- Discussing your stress with a licensed therapist.
-
6Eat foods rich in vitamin C to possibly help manage hives. Vitamin C has antihistamine properties, so eating more citrus fruits, berries, leafy greens, and tomatoes (to name a few excellent vitamin C sources) may help manage your hives. However, be sure to avoid any vitamin C-rich foods that are triggers for your hives!
- Vitamin C supplements may be helpful, but there’s less evidence to support this. Talk to your doctor if you’re interested in taking supplements.
-
7Take supplements like nettle that may provide some hives relief. Nettle teas and similar concoctions have long been used for itch relief due to nettle’s presumed antihistamine properties. The easier option is to take up to 6 nettle supplement capsules (400 mg each) per day. Keep in mind that there is little scientific evidence to support the anti-itch benefits of nettle, though.[15]
- Consider other potential anti-itch supplements as well, such as fish oil, rutin, quercetin, and coleus forskohlii.
- For your safety, consult your doctor or pharmacist before taking any new supplements, as they may cause side effects or interfere with medications.
Using Medications
-
1Take an over-the-counter (OTC) or prescription antihistamine.[16] This is typically the first-line treatment for itchy hives, and is often quite effective. Try an OTC oral antihistamine, such as Claritin (10 mg once daily for adults and kids ages 6 and up; 5 mg once per day for kids 3-5), Zyrtec (10 mg once a day for adults and kids 12 and up; 5 mg once a day for kids 6-11; 2.5 mg per day for kids 3-5), Allegra (a 180 mg tablet once a day for adults), or Benadryl (25-50 mg every 4-6 hours for adults; 12-25 mg every 6 hours for kids 6-12; 6.25 mg every 6 hours for kids 3-6), or talk to your doctor about getting a prescription version. You’ll take a single daily pill in most cases, but follow the package directions or your doctor’s instructions.
- Opt for non-drowsy antihistamines when possible, or you may feel really tired and worn out all day. They’re also less likely to cause side effects such as dizziness, low blood pressure, or a rapid heartbeat.
- Talk to your doctor or pharmacist first if you have any other medical conditions or are taking prescription medications.
-
2Apply a topical OTC or prescription anti-itch cream as advised. Hydrocortisone 1% cream is a common OTC anti-itch cream that is often effective in dealing with itchy hives, and it’s also available in prescription strength as needed. However, be aware that, in some cases, hydrocortisone and other steroidal anti-itch creams can make hives worse.[17]
- For adults and children over 6 years old, apply a thin film of hydrocortisone cream to the hives 4 times a day as needed for 5-7 days.
- Try starting with the lowest concentration of hydrocortisone and gradually raise the strength until you find the concentration that works for you. You can get hydrocortisone ointment in 0.5%-1% concentrations, while the creams come in a range of strengths from 0.5%-2.5%.
- Don’t use hydrocortisone if you have liver problems or are pregnant or nursing. Discuss other possible restrictions, side effects, and drug interactions with your doctor or pharmacist.
-
3Swallow a prescribed daily corticosteroid tablet. Prescription corticosteroids such as prednisone reduce your body’s inflammatory response and can significantly reduce the itchiness and irritation of hives. Corticosteroids carry many potential risk factors, side effects, and drug interactions, however, so be sure to have a detailed discussion with your doctor before starting on a daily oral dose.[18]
- Once you start taking prednisone, you should not stop taking it suddenly unless specifically advised to do so by your doctor. Instead, you’ll likely be directed to taper off of the medication over a period of days or weeks.
-
4Try immunosuppressant medications if other options aren’t helping. If you’re not getting relief from typical anti-itch options, there are several immunosuppressant medications that your doctor may consider prescribing. As always, make sure your doctor knows about any health conditions you have and other medications and supplements you take, and take the prescribed medication exactly as directed.[19]
- Your doctor is more likely to try immunosuppressants if you’ve been diagnosed with chronic hives (also called chronic urticaria), which means you’ve experienced hives daily or nearly daily for at least 6 weeks.
- Taking an immunosuppressant makes you more susceptible to infection, among other risk factors that you should weigh with your doctor.
-
5Make sure you know the signs that you need immediate medical help. In rare cases, hives can develop into a severe and possibly life-threatening condition. If you experience any signs of a severe allergic reaction, seek emergency medical help right away—or if you’ve been prescribed epinephrine (such as an Epi-Pen), use it and then get immediate help. Serious signs include:[20]
- Difficulty breathing or swallowing.
- A rapid heart rate.
- Fainting or severe dizziness.
- Severe nausea or vomiting.
- Rapid and severe swelling of the throat, mouth, or face.
Expert Q&A
-
QuestionHow do antihistamines work against allergies?
 Farah Khan, MDDr. Farah Khan is a Board Certified Allergist and Immunologist who graduated from fellowship in 2020. She specializes in asthma, food allergy, skin conditions, and rhinosinusitis care, and treats both adult and pediatric patients. Dr. Khan holds an MD from Ross University School of Medicine. She completed her Pediatric Residency training at INOVA Children's Hospital and her fellowship at Virginia Commonwealth University. Dr. Khan is an active member of the American Academy of Allergy, Asthma and Immunology as well as the Clinical Immunology Society.
Farah Khan, MDDr. Farah Khan is a Board Certified Allergist and Immunologist who graduated from fellowship in 2020. She specializes in asthma, food allergy, skin conditions, and rhinosinusitis care, and treats both adult and pediatric patients. Dr. Khan holds an MD from Ross University School of Medicine. She completed her Pediatric Residency training at INOVA Children's Hospital and her fellowship at Virginia Commonwealth University. Dr. Khan is an active member of the American Academy of Allergy, Asthma and Immunology as well as the Clinical Immunology Society.
Board Certified Allergist & Immunologist Antihistamine medications provide relief by blocking a large portion of the "itch signals" running through your body.
Antihistamine medications provide relief by blocking a large portion of the "itch signals" running through your body.
References
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=stb117158&lang=en-ca
- ↑ https://www.besthealthmag.ca/best-you/home-remedies/natural-home-remedies-for-hives/
- ↑ https://www.besthealthmag.ca/best-you/home-remedies/natural-home-remedies-for-hives/
- ↑ https://www.besthealthmag.ca/best-you/home-remedies/natural-home-remedies-for-hives/
- ↑ https://newsnetwork.mayoclinic.org/discussion/home-remedies-help-with-itchy-hives/
- ↑ Farah Khan, MD. Board Certified Allergist & Immunologist. Expert Interview. 5 January 2022.
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ Farah Khan, MD. Board Certified Allergist & Immunologist. Expert Interview. 5 January 2022.
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://acaai.org/allergies/types-allergies/hives-urticaria
- ↑ https://acaai.org/allergies/types-allergies/hives-urticaria
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://www.aad.org/public/diseases/a-z/hives-chronic-relief
- ↑ https://www.besthealthmag.ca/best-you/home-remedies/natural-home-remedies-for-hives/
- ↑ Farah Khan, MD. Board Certified Allergist & Immunologist. Expert Interview. 5 January 2022.
- ↑ https://acaai.org/allergies/types-allergies/hives-urticaria
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://www.nhs.uk/conditions/hives/






















-Electric-Shock-Step-9.webp)




















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...