This article was co-authored by Zora Degrandpre, ND. Dr. Zora Degrandpre is a Natural Health Doctor and Licensed Naturopathic Physician in Vancouver, Washington. She is a grant reviewer for the National Institutes of Health and the National Center for Complementary and Alternative Medicine. She received her ND from the National College of Natural Medicine in 2007.
There are 11 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 25 testimonials and 89% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 1,481,664 times.
Hives are a raised, itchy skin rash caused by an allergic reaction. In almost all cases they're harmless and go away on their own eventually. In the meantime, however, they can cause a lot of discomfort. While an allergist can run some tests and determine what exactly is causing your hives, you can treat most cases by yourself at home with only a few ingredients and lifestyle changes. If your hives are chronic or you experience any breathing issues, then see a doctor right away.
Steps
Reducing the Itching
-
1Apply a cold compress to soothe the hives. Cool temperatures usually alleviate the itching from hives. Take either an ice pack or a towel soaked in cold water and press it against the affected area. Hold it on for 15 minutes at a time to soothe the hives. This is a good treatment for hives that don’t cover a widespread area.[1]
- If you use ice or a cold pack, always wrap it in a towel before applying it. Cold temperatures directly on your skin can cause damage.
- You can re-wet the towel as needed if you’re using cold water.
-
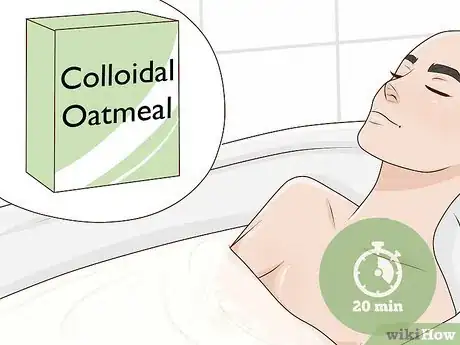
2Take a cool bath with colloidal oatmeal for widespread hives. If the hives cover a large area of your body, then it’s much harder to treat them with compresses. Instead, try a cool or lukewarm bath. Take come colloidal oatmeal, which is ground up into a fine powder, and throw 1 or 2 handfuls under the faucet while the tub is filling. Then soak for 20-30 minutes to soothe your skin.[2]
- If you can bear it, a cool bath will soothe the hives best. However, this may be uncomfortable, so a lukewarm bath is a good choice for more comfort that won’t aggravate the hives.
- You can buy colloidal oatmeal at most food stores and pharmacies. You can also make your own by grinding up normal oats in a food processor.
- If you don’t like taking baths, a cool shower will also help.
Advertisement -
3Rub calamine lotion onto the hives after bathing. After you bathe, your pores are more open and will absorb lotions better. Put a dab of calamine lotion onto your finger or a cotton ball and rub it onto any itchy areas. Continue rubbing until the lotion is clear.[3]
- Follow the application instructions on the product bottle. Usually, instructions say to apply the cream no more than 3 times per day.
- Don't apply calamine lotion to your face.
- You can buy calamine lotion at most pharmacies.
-
4Wear loose-fitting clothes to avoid trapping heat and moisture. Pressure, heat, and friction can increase itching and make your hives worse. Until your symptoms improve, stick with comfortable, loose-fitting clothing to let your skin breathe. Good choices are sweatpants, loose shirts, pajama pants, and athletic shorts.[4]
- Try to dress as cool as possible too, because heat can make hives worse. Wear light fabrics and shorts if the weather allows.
- Also avoid rough or scratchy clothes. Wool and denim will probably be uncomfortable. Soft fabrics like cotton are best.
- If you suffer from chronic hives, then changing your wardrobe permanently could help. Get a lot of loose, light, cotton clothes to prevent friction and heat.
-
5Keep yourself cool until the hives subside. Heat makes itching and hives worse, so stay as cool as you can until they go away. Besides dressing in light clothing, try avoiding activities where you’ll heat up and sweat. Take a day off from the gym or sports and relax instead. In most cases, the hives will subside in a day or so and you can get back to your normal activities.[5]
- Sit in front of fan or turn the AC on to keep your skin cool if the weather is hot.
- Also wear light clothes so you don’t get overheated.
- Some foods like spices and hot beverages can also increase your body temperature. Stick to iced drinks and mild food until the outbreak subsides.
-
6Stay in the shade if you have to go outside. Direct sunlight can heat up your skin and aggravate hives. If you can't stay inside, then avoid sunlight as much as possible. Stay in the shade and under trees or awnings to prevent the hives from getting worse.[6]
- If you have light pants and long sleeve shirts, wear them to keep your hives out of direct sunlight.
-
7Use fragrance-free lotions and moisturizers. Harsh skincare products are a major cause of hives. Switch all of your moisturizers and lotions to fragrance-free varieties. Also look for water-based products instead of oil-based ones, which are heavy and can clog your pores.[7]
- Try using hypoallergenic lotions designed for sensitive skin. These are less likely to cause hives.
-
8Avoid scratching the hives so they don’t get worse. This might be tough, but scratching really does make hives itchier and more painful. Resist the urge to scratch as well as you can. Instead, apply a cold compress or just press down lightly with your fingers to alleviate the itching.[8]
- If you can’t avoid itching, try wearing soft gloves. These prevent you from breaking your skin.
Preventing Further Outbreaks
-
1Track your activities to see if something specific causes your hives. In many cases, your hives have a specific trigger that causes a flareup. Figuring out your triggers can help you treat the hives and avoid further outbreaks. Track your meals, outfits, and activities to see what you were doing leading up to a hive outbreak. This will give you an idea of what caused it.[9]
- Almost anything can cause hives, so the triggers are very specific to you. Common hive triggers are certain foods, medications, pet dander, plants, dyes and food colorings, heat, stress, and pressure.
- Keeping a hive journal is a good way to track your activities. Write down when your hives started and what you did 1-2 hours before that, including what you were wearing and what you ate. If you see a doctor or allergist at some point, bring the journal with you.
-
2Avoid your triggers to prevent further flareups. Once you’ve made a list of activities you were doing before getting the hives, you’ll probably have an idea of what caused them. If you can narrow the list down to a few specific ingredients or activities, then avoid them as much as you can to prevent future hive outbreaks.[10]
- If you can’t narrow down your triggers, try gradual elimination. For instance, if you suspect that either shellfish or Advil caused your hives, eliminate Advil first and see if your hives come back. If they do, then avoid shellfish instead. This way, you can gradually see what activities do and don’t cause your hives.
- Remember that you can still treat your hives effectively even if you don’t know what causes them. Many people with chronic hives never find out their specific trigger, but still manage their symptoms just fine.[11]
-
3Reduce your stress to avoid flareups. Stress is another major cause of hive outbreaks and a number of other issues as well. If you suffer from chronic hives or regularly get outbreaks when you’re feeling stressed, then take steps to alleviate that stress. Take some time to do enjoyable activities like listening to music, watching a movie, or anything else you enjoy. Regular exercise is also a great stress-reducer.[12]
- Try some stress-reducing activities like meditation, yoga, or deep breathing exercises. Set aside 10 minutes in the morning and evening to de-stress with these activities.
- If you do get hives, try to remain calm because increased stress can make the hives worse. Remind yourself that the hives are an inconvenience, but they aren’t dangerous.[13]
- Try speaking with a professional therapist if you have trouble reducing your stress.
-
4Switch your medications if hives are a side effect. Many medications, both prescription and over the counter, can cause hives as a side effect. If you regularly take any medications, check them for potential side effects or ask your doctor or pharmacist if they could cause hives. Avoid medications that could cause outbreaks and ask your doctor to switch you to a different prescription if you have to.[14]
- While almost any medication could cause hives, aspirin and ibuprofen are common culprits.[15]
- If you avoid a medication but still get hives, then the medication was probably not the cause.
-
5Take a vitamin D supplement to improve your immune response. There is some evidence that vitamin D supplements help alleviate chronic hives by boosting your body’s immune system. Try getting a supplement from the pharmacy and taking it as the product instructs you to. Over time, this can improve your immunity and help your body fight hive outbreaks.[16]
- Always consult your doctor before starting on any supplements to make sure they won’t negatively affect your health.
Seeking Medical Care
-
1Get immediate care for swelling in your throat. In rare cases, hives can cause swelling in your throat due to an anaphylactic reaction, which can be vary scary.[17] However, try not to worry because epinephrine can help. Use your EpiPen, if you have one. Alternatively, get someone to take you to the emergency room or call for help. A doctor will likely administer epinephrine to combat your reaction. During an anaphylactic reaction, you may also have these symptoms:[18]
- Skin rashes which may include hives, itching, and flushed or pale skin.
- A sense of warmth.
- The sensation or feeling a lump in the throat.
- Wheezing or other difficulty in breathing.
- A swollen tongue or throat.
- A rapid pulse and heartbeat.
- Nausea, vomiting or diarrhea.
- Dizziness or fainting.
-
2Visit your doctor if your symptoms continue after 2-3 days of home care. Your hives should start to improve after a few days. However, home treatment may not work for everyone. If your hives don’t get better or start to get worse, go to your doctor to learn about your other treatment options. Your doctor will do a physical examination to diagnose your hives.[19]
- Tell your doctor when your hives started, as well as what home treatments you’ve used.
- If you have hives often or they last longer than 6 weeks, you may want to see a dermatologist. They can help you figure out what’s causing your hives so that you can find relief.[20]
-
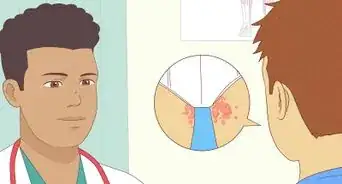
3Get an allergy test to find out what’s causing recurring hives. In most cases, you won’t need an allergy test. However, your doctor may recommend getting one if you have chronic hives.[21] During the allergy test, a nurse will prick or scratch your skin with 40 different allergens. Then, they’ll check your skin after 15 minutes to see if you had a reaction to any of the allergens. Finally, your doctor will evaluate the results and determine if you have any allergies.[22]
- An allergy test shouldn’t hurt, but you may feel some discomfort.
- Your doctor is more likely to recommend an allergy test if you have chronic hives.
-
4Take a non-drowsy antihistamine to treat your hives and relieve itching. These medicines stop your body’s reaction to an allergen. They will reduce the inflammation or swelling in your body, relieve itching, and reduce redness. Over time, they may help you recover from the hives.[23]
- You can buy some antihistamines over-the-counter. For instance, cetirizine (Zyrtec, Zyrtec-D), clemastine (Tavist), fexofenadine (Allegra, Allegra D) and loratadine (Claritin, Claritin D, Alavert) are all non-drowsy options.
- Your doctor may prescribe a stronger prescription antihistamine, if they think you need it.
-
5Use an anti-inflammatory to reduce swelling, itching, and redness. You can use an NSAID to reduce inflammation, but you may need a corticosteroid. Use these medications for a short period of time, such as a week, or as directed by your doctor.[24]
- It’s not safe to use NSAIDs or corticosteroids for the long-term, unless your doctor tells you to do so.
- You can buy NSAIDs over-the-counter. For instance, take ibuprofen (Advil, Motrin) or naproxen (Aleve) as directed on the label for pain and inflammation relief.
- For another over-the-counter option, you can try corticosteroid nasal spray, such as Nasacort. However, this won’t be as effective as taking a prescription treatment.
- Your doctor may prescribe you a corticosteroid, such as Prednisone, Prednisolone, or Methylprednisolone. These medications can provide more relief than over-the-counter options.[25]
-
6Ask your doctor about a leukotriene inhibitor if your hives are chronic. If you have hives often, then you may need a long-term treatment. Your doctor may prescribe a medication called a leukotriene inhibitor, such as montelukast (Singulair). These medications are nonsteroidal anti-inflammatories, and they reduce pain and swelling in your body.[26]
- Although this medication is usually safe to take for a longer period of time, it’s not right for everyone. Your doctor will help you find the right treatment for you.
Expert Q&A
-
QuestionCan I substitute Flonase for Nasacort?
 Zora Degrandpre, NDDr. Zora Degrandpre is a Natural Health Doctor and Licensed Naturopathic Physician in Vancouver, Washington. She is a grant reviewer for the National Institutes of Health and the National Center for Complementary and Alternative Medicine. She received her ND from the National College of Natural Medicine in 2007.
Zora Degrandpre, NDDr. Zora Degrandpre is a Natural Health Doctor and Licensed Naturopathic Physician in Vancouver, Washington. She is a grant reviewer for the National Institutes of Health and the National Center for Complementary and Alternative Medicine. She received her ND from the National College of Natural Medicine in 2007.
Natural Health Doctor Both Flonase and Nasacort are available without a prescription. These medications contain different steroids but both are meant to treat sinus congestion due to allergies. Neither should be used in children without talking to your doctor first. You can substitute Flonase for Nasocort, but you should use it regularly but shouldn't use more than 1 spray in each nostril twice a day. If you have diabetes, glaucoma, cataracts or liver disease, ask your doctor before using.
Both Flonase and Nasacort are available without a prescription. These medications contain different steroids but both are meant to treat sinus congestion due to allergies. Neither should be used in children without talking to your doctor first. You can substitute Flonase for Nasocort, but you should use it regularly but shouldn't use more than 1 spray in each nostril twice a day. If you have diabetes, glaucoma, cataracts or liver disease, ask your doctor before using. -
QuestionI've had an itchy, red, bumpy rash all over my body for the last 16 months. I have been to specialists but they haven't helped. What can I do?
 Zora Degrandpre, NDDr. Zora Degrandpre is a Natural Health Doctor and Licensed Naturopathic Physician in Vancouver, Washington. She is a grant reviewer for the National Institutes of Health and the National Center for Complementary and Alternative Medicine. She received her ND from the National College of Natural Medicine in 2007.
Zora Degrandpre, NDDr. Zora Degrandpre is a Natural Health Doctor and Licensed Naturopathic Physician in Vancouver, Washington. She is a grant reviewer for the National Institutes of Health and the National Center for Complementary and Alternative Medicine. She received her ND from the National College of Natural Medicine in 2007.
Natural Health Doctor You may have a sensitivity to detergent, soap, clothing, perfumes and/or foods. Have you changed any daily habit in the last 16 months? New detergent or soap? Try using only natural detergents and soaps for a while to see if it helps. Wear only cotton or linen clothing. Keep a diet diary, writing down all the foods you eat — see if the itching gets worse after you eat certain foods.
You may have a sensitivity to detergent, soap, clothing, perfumes and/or foods. Have you changed any daily habit in the last 16 months? New detergent or soap? Try using only natural detergents and soaps for a while to see if it helps. Wear only cotton or linen clothing. Keep a diet diary, writing down all the foods you eat — see if the itching gets worse after you eat certain foods. -
QuestionHow long can I safely take 10 mg. Loratadine to treat urticaria?
 Zora Degrandpre, NDDr. Zora Degrandpre is a Natural Health Doctor and Licensed Naturopathic Physician in Vancouver, Washington. She is a grant reviewer for the National Institutes of Health and the National Center for Complementary and Alternative Medicine. She received her ND from the National College of Natural Medicine in 2007.
Zora Degrandpre, NDDr. Zora Degrandpre is a Natural Health Doctor and Licensed Naturopathic Physician in Vancouver, Washington. She is a grant reviewer for the National Institutes of Health and the National Center for Complementary and Alternative Medicine. She received her ND from the National College of Natural Medicine in 2007.
Natural Health Doctor Loratadine is commonly used to treat both acute (sudden) and chronic (long-term) urticaria (hives). It is considered safe to use long-term, but talk to your doctor to make sure you should continue after about six months.
Loratadine is commonly used to treat both acute (sudden) and chronic (long-term) urticaria (hives). It is considered safe to use long-term, but talk to your doctor to make sure you should continue after about six months.
Warnings
- There are some remedies that either haven't been evaluated by doctors or are proven ineffective. Witch hazel could aggravate hives, and aloe doesn't work well on them. Stick to remedies that are proven effective.⧼thumbs_response⧽
References
- ↑ https://www.aad.org/public/diseases/a-z/hives-chronic-relief
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://www.aad.org/public/diseases/a-z/hives-chronic-relief
- ↑ https://www.mayoclinic.org/diseases-conditions/chronic-hives/diagnosis-treatment/drc-20352723
- ↑ https://www.mayoclinic.org/diseases-conditions/chronic-hives/diagnosis-treatment/drc-20352723
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://www.aad.org/public/diseases/a-z/hives-chronic-relief
- ↑ https://www.mayoclinic.org/diseases-conditions/chronic-hives/diagnosis-treatment/drc-20352723
- ↑ https://www.allergy.org.au/patients/skin-allergy/urticaria-hives
- ↑ https://www.allergy.org.au/patients/skin-allergy/urticaria-hives
- ↑ https://www.aad.org/public/diseases/a-z/hives-chronic-relief
- ↑ https://www.stress.org/what-to-do-when-stress-gives-you-hives
- ↑ https://www.aad.org/public/diseases/a-z/hives-chronic-relief
- ↑ https://www.allergy.org.au/patients/skin-allergy/urticaria-hives
- ↑ https://www.aad.org/public/diseases/a-z/hives-chronic-relief
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4203568/
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/symptoms-causes/syc-20354908
- ↑ https://www.mayoclinic.org/diseases-conditions/anaphylaxis/symptoms-causes/syc-20351468
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/symptoms-causes/syc-20354908
- ↑ https://www.aad.org/public/diseases/itchy-skin/hives#treatment
- ↑ https://www.aad.org/public/diseases/itchy-skin/hives#treatment
- ↑ https://www.mayoclinic.org/tests-procedures/allergy-tests/about/pac-20392895
- ↑ https://www.aad.org/public/diseases/itchy-skin/hives#treatment
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://www.aad.org/public/diseases/itchy-skin/hives#treatment
- ↑ https://www.mayoclinic.org/diseases-conditions/hives-and-angioedema/diagnosis-treatment/drc-20354914
- ↑ https://www.drugs.com/mtm/calamine-topical.html
About This Article
To treat hives naturally, try using a cold compress to alleviate skin irritation. Soak a clean, cotton towel in cold water and hold it over the affected area for 10 minutes. Re-soak the towel after 10 minutes to help keep the area cool. You can also try an oatmeal bath to get relief from the discomfort of hives. Add 1 to 2 cups of powdered, rolled oats to a warm bath. Soak in the bath for as long as you like and repeat it as often as you need. Some supplements may also be effective at treating hives. Try taking rutin supplements as these can reduce inflammation and swelling. You can also take quercetin supplements to help reduce swelling. If the hives last longer than 3 days or if you have trouble breathing, see your doctor. For more information from our Naturopathy co-author, like how to avoid your allergens, read on!











































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...