This article was medically reviewed by Farah Khan, MD. Dr. Farah Khan is a Board Certified Allergist and Immunologist who graduated from fellowship in 2020. She specializes in asthma, food allergy, skin conditions, and rhinosinusitis care, and treats both adult and pediatric patients. Dr. Khan holds an MD from Ross University School of Medicine. She completed her Pediatric Residency training at INOVA Children's Hospital and her fellowship at Virginia Commonwealth University. Dr. Khan is an active member of the American Academy of Allergy, Asthma and Immunology as well as the Clinical Immunology Society.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 34,611 times.
Have you developed a sudden rash? Is it itchy, inflamed, and blistered?[1] You may have contact dermatitis. Dermatitis is a general term for inflammation of the skin and has many varieties and possible causes. Contact dermatitis is caused when the skin reacts to an allergenic or irritating substance. To spot it, know how to recognize the symptoms and find the culprit. You’ll then be able to avoid a repeat in the future.
Steps
Recognizing Symptoms
-
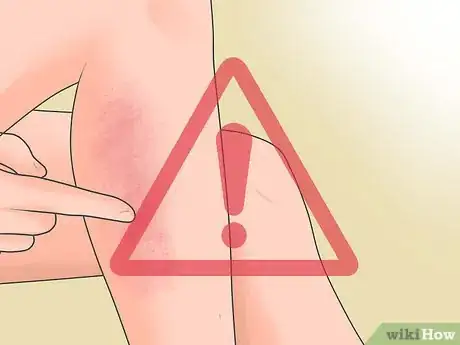
1Beware of sudden rashes. Contact dermatitis usually shows up when you’ve been touched by a substance that triggers a reaction, like poison ivy or oak or latex gloves. The rash usually will crop up suddenly, within hours of contact. It may also last for two to four weeks.[2]
- There are two basic kinds of contact dermatitis, allergic or irritant. Allergic dermatitis occurs when you have contact with an allergenic substance and it produces a delayed reaction. This may develop over a period of 48 to 96 hours, or it may take even longer, between seven and 10 days after the first exposure.
- Allergenic contact dermatitis can also cause oozing blisters, intense itching, and sometimes swelling in the face, eyes, or genitals.[3]
- Irritant contact dermatitis occurs when skin comes into contact with an irritant, like a detergent or solvent. Skin damage may be permanent if the irritant is powerful, like acid or lye soap.[4]
- This kind of dermatitis may also cause mild swelling, itching, blisters, painful ulcers, or tight-feeling and cracked skin.
- If you note a rash and think you may have come into contact with a plant like poison oak, ivy, or sumac, make sure you wash everything that may have been in contact with the plant with cold water. This includes clothing, gardening tools, sports equipment, and pets.
-
2Check that the rash is localized. Contact dermatitis happens when a substance comes into contact with the skin – your reaction will therefore be limited more or less to where the substance touched you (so if you ran through poison oak with pants on but no shoes, your feet will react but your legs will be spared). If the rash is localized, try to determine if the source is in fact a foreign substance.[5]
- Is the rash on your hands or face? Contact dermatitis most often affects these areas and rarely occurs on the scalp, palms of hands or soles of the feet.
- Is the rash confined to the area that was exposed? A delayed reaction sometimes makes it look like a rash from contact dermatitis is spreading, but for the most part it should only occur where your skin was in contact with the irritant or allergen.
Advertisement -
3Note other swelling, blistering, burning, or tenderness. Contact dermatitis may cause many other symptoms besides redness and a rash.[6] Depending on the strength of the irritant or allergen, you may have pain, blistering, bumps, and severely dry and cracked skin. You may also show non-dermatological signs if the cause is an allergen, like burning lungs, eyes, or nasal passages.[7]
- Dry skin with a glazed, parched aspect is often the first sign with irritants. Thickened skin and cracking can follow if contact continues for a longer period of time.
- In very severe cases of exposure to an irritant, the skin may also exhibit burns or tissue death (necrosis).
- Burning eyes, nose, and lungs can indicate allergic contact dermatitis, but can also point to an irritant in the air.
Narrowing in on the Culprit
-
1Focus on the affected area. Pay close attention to the area that is irritated and to anything around it. The culprit may be a substance you touched, triggering a reaction, or it might be a fabric, plastic, or metal item that is coming into contact with the skin. The rash’s location will often suggest a cause.[8]
- If you’ve been handling an irritant like a mild solvent and develop a rash on your hands, for example, the solvent is probably the cause.
- Were you walking outdoors and then got a rash on your legs? You might be dealing with contact dermatitis from poison ivy, poison oak, or poison sumac.
- People sometimes develop dermatitis from allergies to fabrics, plastics, or metals. A plastic wristwatch band can cause a reaction, for instance.
-
2Recall your activities. Try to remember your recent activities and what sorts of substances may have contacted the affected area of skin – think in terms of chemicals but also plant materials, fabrics, plastics or rubber, soaps, and sanitizers. Any of these materials may be responsible.[9]
- Have you been outside on a nature trail, in a wooded lot, or in scrubby area? Keep in mind that you can easily touch poison ivy or a similar plant and not realize it, leading to allergic contact dermatitis. Affected areas for these rashes are often the feet, ankles, legs, or arms. The rash will usually appear linear where the plant has brushed across the skin or resin has been spread by scratching.
- Have you handled cleaning products lately, like soaps, detergents, or solvents? These products can cause irritant contact dermatitis, as can rubber and latex and metals like nickel and gold.
- Write things down, if it helps. Keep a notebook with all the activities and items that may have led to the reaction or list anything that might have touched your skin for two days before the rash appeared.
-
3Get tested for allergies.[10] The best and most accurate way to determine if your dermatitis is caused by an allergic reaction is through testing. Make an appointment with an allergy specialist. She can then perform a battery of tests to see whether you have allergies to the substances that most likely caused the rash.[11]
- Skin prick test can test for reaction to as many as 40 different allergens. A diluted allergen is applied with a prick to your skin. Your skin is observed for 15 minutes. A wheal, irritation, redness or itching may indicate that you are allergic to a substance that was applied.
- Another way to test for allergies is through a patch test. This means that you will have to wear patches containing a small amount of each substance for about 48 hours. If you react to a patch, it indicates you have an allergy.
- The allergist can use patch testing to check fragrances, hair dyes, rubber, and other substances. It will also detect photoallergic reactions, which occur when a substance like shaving lotion or sunscreen reacts in sunlight to cause a skin reaction.
Preventing Repeats
-
1Avoid allergenic and irritating products. Obviously, you should avoid contact with the substance that caused your dermatitis in the first place. This is not always so easy, however, especially if it’s a common chemical or something you have to work around daily. Use vigilance and proper protection.[12]
- If avoidance is not possible, apply a barrier lotion such as IvyBlock, Work Shield, Zinc Oxide paste, or Desenex prior to potential exposure.
- Check the labels on all products that you put on your skin for allergens or irritants, or contact the manufacturer directly. Substitute other products for ones that gives you contact dermatitis.
- The allergen in poison ivy may remain active for months. It is crucial for exposed clothing, shoes, tools, camping equipment and pets to be washed thoroughly to avoid spreading the allergen.
-
2Wear protective clothing. Clothing can form an effective physical barrier between your skin and irritants and help prevent repeat contact dermatitis or if you have had issues with photoallergic reactions to sunlight. Use basic protection: long pants, long-sleeved shirts, and boots can go a long way, whether against chemicals, plants, or other substances.[13]
- Consider using gloves. Irritant contact dermatitis often affects the hands, so gloves are an easy way to reduce contact. Use cotton gloves if you have an allergy to latex or rubber. Take your gloves off periodically, too, as sweat can aggravate dermatitis symptoms.
- Follow all safety instructions on protective equipment if you work with irritants.
-
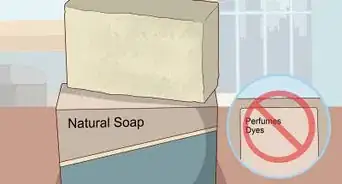
3Keep clean. Be sure to wash thoroughly if you come into contact with an allergenic or irritating substance. Treat the area with cool water and soap for at least 25 seconds and then rinse again. Try to remove as much of the substance as you can, as fast as you can, in order to avoid a repeat reaction.[14]
- Wash the area with Dial brand soap, GOOP (a grease removing agent), or Tecnu as these have been shown to be effective in binding to urushiol (the oil in plants that causes allergic reaction) for more thorough removal. Be sure to wash under the fingernails, too, especially if you have been scratching.
- Consider an after-work cream, as well, if you can’t totally avoid contact with an irritating or allergenic substance. These are designed for use after work to calm your skin and reduce the frequency and severity of reactions.
Warnings
- Contact dermatitis rashes can get infected. Therefore, follow up with your primary care provider immediately if symptoms worsen or signs of infection develop (fever, increased pain, purulent drainage).⧼thumbs_response⧽
- There are other conditions that may have symptoms similar to contact dermatitis, including: insect bites, herpes simplex, herpes zoster, impetigo, ringworm, scabies, sea bather's eruption, swimmer's itch, Stevens-Johnson Syndrome, varicella, and bullous pemphigoid.⧼thumbs_response⧽
References
- ↑ Farah Khan, MD. Board Certified Allergist & Immunologist. Expert Interview. 5 January 2022.
- ↑ https://my.clevelandclinic.org/health/diseases/6173-contact-dermatitis
- ↑ https://dermnetnz.org/topics/allergic-contact-dermatitis
- ↑ https://dermnetnz.org/topics/irritant-contact-dermatitis
- ↑ https://medlineplus.gov/ency/article/000869.htm
- ↑ Farah Khan, MD. Board Certified Allergist & Immunologist. Expert Interview. 5 January 2022.
- ↑ https://my.clevelandclinic.org/health/diseases/6173-contact-dermatitis
- ↑ http://acaai.org/allergies/types/skin-allergies/contact-dermatitis
- ↑ http://acaai.org/allergies/types/skin-allergies/contact-dermatitis
- ↑ Farah Khan, MD. Board Certified Allergist & Immunologist. Expert Interview. 5 January 2022.
- ↑ http://acaai.org/allergies/types/skin-allergies/contact-dermatitis
- ↑ http://www.nhs.uk/Conditions/Eczema-(contact-dermatitis)/Pages/Prevention.aspx
- ↑ http://www.nhs.uk/Conditions/Eczema-(contact-dermatitis)/Pages/Prevention.aspx
- ↑ http://www.nhs.uk/Conditions/Eczema-(contact-dermatitis)/Pages/Prevention.aspx



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...