This article was medically reviewed by Venessa Peña-Robichaux, MD. Dr. Peña-Robichaux is a board certified Dermatologist and Clinical Professor in Texas specializing in the treatment of pediatric and adult skin conditions. She completed her MD at Harvard Medical School in 2010 and completed her residency at Henry Ford Hospital in Detroit, Michigan. She is a member of the American Academy of Dermatology and the American Telemedicine Association.
There are 20 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 91% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 283,876 times.
Eczema, also called atopic dermatitis, is a chronic condition characterized by dry, red and itchy skin. The exact cause for eczema is unknown but it is thought to be hereditary and tends to flare up after you are exposed to certain triggers; eczema is often seen in those with a family history of asthma or allergies. Fortunately, you can avoid the triggers and use certain treatments to control the disease.[1]
Steps
Treating Your Eczema
-
1Use steroid creams. Topical treatments, such as creams, are the first thing you should try when it comes to treating eczema. Corticosteroid creams can help reduce itching resulting from eczema. In a clinical study, 80% of respondents reported that their eczema or dermatitis responded well to hydrocortisone. Ask your doctor if you should use a corticosteroid cream or an ointment to treat eczema.[2]
- Your doctor may prescribe a corticosteroid cream or you can try an over-the-counter product, such as a 1% hydrocortisone cream.[3]
- If using an over-the-counter hydrocortisone cream, use it two to three times per day for seven days. If you fail to see improvement or an abatement of itching in seven days, discontinue use and call your doctor.[4]
- Ask your doctor if you need prescription steroids. They are much stronger and more effective than 1% hydrocortisone.
- If you are not improving with prescription topical steroids, your doctor may recommend systemic corticosteroids
- Although the dosage of steroids in over-the-counter products is small, use the product only as directed on the package or by your doctor. Overuse of corticosteroids can cause side effects including but not limited to thinning of the skin, redness, lightening of the skin and acne.
-
2Ask your doctor about antibiotics. Because eczema causes itching, you are at risk of a bacterial skin infection if you scratch and damage the itchy skin. Your doctor may recommend you take antibiotics to treat the infection.[5]
- Always take antibiotics as instructed by your doctor and complete the treatment regimen even if the infections seems to have subsided.
Advertisement -
3Consult your doctor if you should use calcineurin inhibitors. These creams help control itching and reduce eczema flare ups; however, these prescription-only creams should only be used when other medications have failed due to side effects.[6]
- Calcineurin inhibitors include tacrolimus (Protopic) and pimecrolimus (Elidel)
-
4Try light therapy. Phototherapy uses natural sunlight or artificial ultraviolet (UV) radiation to suppress overactive immune system and reduce inflammation in the skin. As a result, it helps relieve rash and itching. The most common type of phototherapy used for eczema is called narrow band UVB and overall is a very safe and effective treatment.[7]
- Because long-term phototherapy has harmful effects (including skin aging and risk of cancer), consult your doctor before using light therapy.[8]
- Phototherapy is not the same as visiting a tanning bed — it can only be administered in a doctor's office.
- If your child has atopic dermatitis, narrowband UVB is considered safe. Talk to your doctor about this treatment.
-
5Take a bleach bath. Bathing in a diluted-bleach water helps reduce bacterial infections on your skin. Try bleach baths two to three times a week for a few weeks to see if it helps relieve your symptoms.[9]
- Add 1/2 cup of bleach (use household bleach and not concentrated bleach) to a bathtub filled water. Soak just the affected skin (not in the face) for 10 minutes. Rinse with warm water and moisturize.
- Another option is to try an oatmeal bath. The ingredient in oats has anti-inflammatory and anti-itching properties that can be very soothing for your skin.
-
6Use a cold compress. Hold an ice pack over your eczema-prone areas to help relieve the itching. You can also use a clean, wet washcloth soaked in cold water.[10]
- Cold compress also helps protect the skin and may prevent you from scratching the itchy skin.
-
7Avoid scratching. You may feel tempted to scratch the itchy skin, but try to avoid this as much as you can. Scratching can damage the skin and cause a bacterial infection.[11]
- Keep your fingernails short to help keep your skin damage to a minimum.
- You may also want to wear gloves during the night to prevent yourself from scratching while sleeping.
- You may also want to wrap your skin to prevent yourself from scratching. Cover the eczema-prone areas of skin in bandages or gauze when you sleep.
Recognizing Eczema Triggers
-
1Recognize your lifestyle triggers. Eczema flare ups can be triggered by different things that are not the same for everyone. Thus, it is important you learn to recognize the factors (such as clothing materials, chemicals, or foods) that trigger your eczema.[12]
- Keep a diary and write down the products you use and foods you eat. When you experience a flare-up, it is easier to track the possible causes.
- Try eliminating one product at a time to see which may trigger your eczema.
-
2Avoid clothing made of irritating materials. Some materials may irritate your skin and worsen or trigger your eczema. Keep track of your symptoms and if you recognize a material that triggers your eczema, stop using it.[13]
- Avoid scratchy materials, such as wool, and tight-fitting clothes that can irritate your skin and trigger an episode. Opt for light and breathable materials, such as cotton, silk and bamboo.
- Be sure to wash new clothes before wearing them for the first time to soften the fabric and wash off any possible irritants.
- However, some detergents may also trigger an episode by leaving a slight residue on your clothes. Before throwing away your favorite outfit, try using a natural washing powder or a different detergent and see if that makes a difference.
-
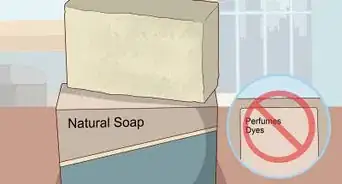
3Check your cosmeceuticals and personal hygiene products. Some cosmeceuticals and personal hygiene products contain ingredients that can trigger eczema. You may need to choose non-irritating lotions, creams, soaps and makeups that are hypoallergenic and/or without added perfumes.[14]
- Use the product for a few weeks to see if it triggers your eczema. If it does, switch the product.
- Avoid products containing sodium lauryl sulfate and parabens. These are common irritants that can dry the skin and trigger a flare-up.
-
4Analyze your diet. Some foods or added ingredients in foods can also trigger your eczema, though this is very rare. Also, you may want to keep a food diary that will help you identify the foods that trigger your condition.[15]
- If you are unsure whether a food triggers your episode, eat it for a few days to see if you experience a flare-up. Then eliminate the product from your diet and see if your eczema clears up. Do the same for all foods that you believe may be triggering the conditions.
- Try eliminating milk and gluten, which are common dietary triggers for eczema.[16]
Preventing Future Flare-ups
-
1Moisturize regularly. To keep your skin moist and prevent eczema and dryness flareups, use a moisturizer at least twice a day. Creams and ointments help retain the skin’s natural moisture and reduce dryness and itching resulting from eczema.[17]
- Use creams and ointments over lotions — lotions contain a lot of water, while creams and ointments have a higher oil content and are better at repairing the skin barrier and retaining moisture.
- Apply moisturizers after bathing or showering to trap in moisture to your skin.
- Choose an unscented, moisturizing soap.
- Pat the skin dry rather than rubbing it to avoid irritation.
- Consider using a barrier repair moisturizers (such as petroleum jelly, Aquaphor, Aveeno Healing Ointment, Crisco, or Coconut Oil) that help lock water into the skin and prevent dryness.
-
2Avoid the environmental factors that trigger your eczema. If and when you identify the factors that cause your eczema (see previous section), avoid these and/or switch products to those that are non-irritating.[18]
- Avoid chemicals, cosmetics and personal hygiene products that trigger your eczema. Remember that it is usually a certain ingredient within a product that is irritating; thus, you may need to avoid a group of products that contain that ingredient.
- Use gentle soaps that are hypoallergenic or made for "sensitive skin."
- Use protective clothing and gloves if you need to use a product that causes your eczema.
-
3Change your showering habits. Wash with warm water, not hot, and limit your showers to 10 minutes. Hot water dries out the skin more than warm water as does a prolonged contact with water.[19]
- If you like to take baths, limit those to 10 minutes also and use bath oil in the water.
- Moisturize immediately after a bath when your skin is still a little moist.
-
4Pay attention to how the weather affects you. Sweating and overheating can increase the chances of eczema flare-ups and worsen the symptoms for some people with eczema.[20] On the other hand, many with eczema do well in the summer but suffer in the winter due to the cold air and dryness. Pay attention to how the weather affects your eczema so you know when to stay indoors and perhaps be extra conscious of moisturizing.[21]
-
5Use a humidifier during winter months or if you live in a dry climate. Where hot and humid weather causes sweating that may trigger eczema, dry air can also exacerbate the condition.[22]
- Use an air humidifier in your bedroom during the night to add moisture to the air and to your skin.
- However, remember to wash the humidifier regularly to prevent harmful microbes from growing in the water.
-
6Limit stress in your life. Stress can trigger eczema flare ups (not to mention increase risk for other health complications); thus, it is important to reduce your stress load. Take steps to organize your life, reduce stress, and deal with anxiety.[23]
- Try Relaxation Techniques, Controlled Breathing and Yoga to reduce stress.
- Regular Exercise can also help fight stress.
Warnings
- Don't try to cover your eczema with makeup, unless it's very well under control. Even then, use an un-scented natural makeup that won't make your skin flare.⧼thumbs_response⧽
- If a topical ointment burns or stings, stop using it and consult your dermatologist.⧼thumbs_response⧽
- Do not use steroids (either topical or oral) if you do not need them — prolonged use of strong steroids can cause harmful effects, such as skin thinning.[24]⧼thumbs_response⧽
References
- ↑ https://www.nhs.uk/conditions/atopic-eczema/causes/
- ↑ https://nationaleczema.org/eczema/treatment/topicals/
- ↑ https://www.nhs.uk/medicines/hydrocortisone-skin-cream/
- ↑ http://www.nlm.nih.gov/medlineplus/druginfo/meds/a682793.html
- ↑ https://www.aad.org/public/diseases/eczema/childhood/treating/antibiotics-antimicrobials
- ↑ https://eczema.org/information-and-advice/treatments-for-eczema/topical-calcineurin-inhibitors/
- ↑ https://eczema.org/information-and-advice/treatments-for-eczema/phototherapy/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK424892/
- ↑ https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/bleach-bath-recipe-for-skin-conditions
- ↑ https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/bleach-bath-recipe-for-skin-conditions
- ↑ https://www.aad.org/public/diseases/eczema/childhood/itch-relief/home-remedies
- ↑ https://my.clevelandclinic.org/health/diseases/9998-eczema
- ↑ https://eczema.org/information-and-advice/triggers-for-eczema/clothing-and-eczema/
- ↑ https://nationaleczema.org/eczema/causes-and-triggers-of-eczema/
- ↑ https://patient.info/skin-conditions/atopic-eczema/eczema-triggers-and-irritants#nav-8
- ↑ https://www.nhs.uk/conditions/atopic-eczema/causes/
- ↑ https://nationaleczema.org/eczema/treatment/moisturizing/
- ↑ https://nationaleczema.org/eczema/treatment/moisturizing/
- ↑ https://nationaleczema.org/eczema/treatment/bathing/
- ↑ https://nationaleczema.org/earning-place-sun/
- ↑ https://eczema.org/information-and-advice/triggers-for-eczema/weather-and-eczema/
- ↑ https://nationaleczema.org/eczema-in-winter/
- ↑ https://nationaleczema.org/eczema-emotional-wellness/
- ↑ https://www.nhs.uk/medicines/hydrocortisone-skin-cream/
About This Article
To treat eczema, start by applying a topical corticosteroid cream, like an over-the-counter 1% hydrocortisone cream, and use it 2-3 times a day for 7 days. If that doesn’t work, talk to your doctor about using a more powerful prescription steroid. You might also consider trying non-medical treatments, like using light therapy or taking a bleach bath, which you can do by putting 1/2 cup of household bleach into your bath and soaking for 10 minutes 2-3 times a week. For tips from our Dermatologist reviewer, including how to prevent future eczema flare-ups, read on!









































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...