This article was medically reviewed by Mark Ziats, MD, PhD. Dr. Mark Ziats is an Internal Medicine Physician, Scientist, Entrepreneur, and the Medical Director of xBiotech. With over five years of experience, he specializes in biotechnology, genomics, and medical devices. He earned a Doctor of Medicine degree from Baylor College of Medicine, a Ph.D. in Genetics from the University of Cambridge, and a BS in Biochemistry and Chemistry from Clemson University. He also completed the INNoVATE Program in Biotechnology Entrepreneurship at The Johns Hopkins University - Carey Business School. Dr. Ziats is board certified by the American Board of Internal Medicine.
This article has been viewed 52,588 times.
Studies show that Remicade (infliximab) can reduce inflammation in your body, so it may help relieve symptoms from conditions like Crohn's disease, ulcerative colitis, rheumatoid arthritis, ankylosing spondylitis, and plaque psoriasis.[1] However, Remicade can cause serious side effects and reduces your body's ability to fight infections, so you may decide it's no longer the right choice for you. Experts agree that it's important to work closely with your healthcare provider while taking Remicade so you can stop the medication if necessary.[2] Talk to your doctor before stopping your treatments so you can do it safely.
Steps
Stopping Remicade
-
1Don’t stop Remicade because your condition is in remission. Some conditions, like Crohn’s disease, will have periods during which symptoms seem disappear or go into remission, but the condition is still present. Stopping your medication during these periods may cause your condition to flare up again. Talk to your doctor before stopping Remicade, even if your symptoms seem to have subsided and you are feeling well.
- The manufacturer recommends staying on a maintenance dose of Remicade even when you are in remission to prevent symptoms from coming back.
- The maintenance dose and frequency will vary depending upon your condition.
-
2Ask your doctor whether you can go back on Remicade. According to the manufacturer, when patients stop taking Remicade, their bodies sometimes produce antibodies against Remicade. This can make it less effective in the future.
- Ask your doctor if she expects that this would occur to you if you tried to go back onto Remicade after stopping.
- Your doctor may be able to tell you how often this occurs to patients that restart Remicade and how severely reduced the effectiveness of the medication is.
Advertisement -
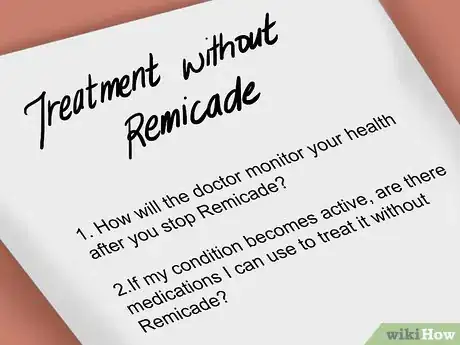
3Make a plan for treatment without Remicade. If you have a serious condition, talk to your doctor about what you will do if your condition worsens. Stopping Remicade will not produce withdrawal symptoms, but it is important that you be monitored to make sure your condition does not get worse. Questions to ask your doctor include:
- What signs should you look for to make sure that your condition is not coming back?
- How will the doctor monitor your health after you stop Remicade?
- Are there other medications or lifestyle changes you can make to keep your condition in remission?
- If your condition becomes active, are there medications you can use to treat it without Remicade?
- Does your doctor recommend decreasing the Remicade gradually and then starting another medication?
-
4Make a schedule to taper off. Chances are your doctor will not recommend suddenly stopping. Your doctor may be concerned that stopping suddenly may increase the likelihood that your condition will flare up again.
- Ask your doctor for recommendations on how to taper off. Your doctor may suggest spacing out your doses further and further until you no longer need it.
- Or alternatively, your doctor might recommend gradually lowering the doses.
- What your doctor feels will be right for you will depend upon your particular situation. You should work with a doctor to determine how to stop Remicade.
Evaluating Whether You Should Stop Remicade
-
1Monitor yourself for side effects. If Remicade produces side effects you should contact your doctor or nurse immediately to discuss whether the medication is right for you. Be aware that not all side effects appear immediately or they may not be side effects of the medication, but in fact part of your disease or something unrelated, such as a cold. Tell your doctor if you develop side effects even if it is days or weeks after the infusion so that she can evaluate your condition. Not everyone experiences side effects, but in some people they may be severe enough that it is necessary to stop the medication. Possible side effects include:[3]
- Stomach pain, vomiting, or nausea
- Fever, flushing, or chills
- Coughing, stuffy or runny nose, sneezing, or sore throat
- Fainting, dizziness, tiredness
- Difficulty breathing
- Chest pain
- Headache or muscle pain
- Hives or an itchy rash
-
2Tell your doctor if you think you may be pregnant or are planning to get pregnant. Ask your doctor whether this medication will be safe for you to use while carrying a child.[4]
- It is unknown whether this medication is safe for women to take while breastfeeding. There have not been enough studies done to demonstrate that it is safe. Talk to your doctor to discuss whether you should give your infant formula while on this medication.
- Some health providers list pregnancy and breastfeeding as a criteria that disqualifies patients as being eligible for Remicade.
-
3Reconsider Remicade if you develop a serious health condition. Some health conditions will prevent you from being eligible for this medication. In particular, because this medication affects your immune system, chronic or acute infections make this may make this medication unsafe for you. Talk to your doctor if you develop any of the following conditions:[5] [6]
- A current systemic infection
- Sepsis
- An abscess
- Heart failure
- Latent or active tuberculosis
- Cancer
- Chronic obstructive pulmonary disease (COPD)
Warnings
- Do not make any changes to your medications without discussing it with your doctor first.⧼thumbs_response⧽
- Tell your doctor about all other prescription medications, over-the-counter medications, vitamins, herbal remedies, and supplements that you take.⧼thumbs_response⧽
References
- ↑ https://www.drugs.com/remicade.html
- ↑ https://www.mayoclinic.org/drugs-supplements/infliximab-intravenous-route/precautions/drg-20068387
- ↑ http://www.mayoclinic.org/drugs-supplements/infliximab-intravenous-route/side-effects/drg-20068387
- ↑ http://www.mayoclinic.org/drugs-supplements/infliximab-intravenous-route/before-using/drg-20068387
- ↑ https://www.rheumatology.org/Learning-Center/Medication-Guides/Medication-Guide-Infliximab-Remicade
- ↑ http://www.mayoclinic.org/drugs-supplements/infliximab-intravenous-route/before-using/drg-20068387
About This Article
To stop Remicade treatments, first talk to your doctor to make sure you’re ready to stop taking it, since it’s possible your condition could return without medication. Once your doctor recommends you stop it, you’ll want to make a schedule to taper off the medication, which will help prevent your condition from returning. For example, you may need to start spacing your doses further apart or gradually take smaller doses. You should also ask your doctor if you will need additional treatment once you stop taking Remicade. Although stopping Remicade doesn’t produce withdrawal symptoms, you should watch to make sure symptoms of your condition don’t return, which may mean you need to take a different medication. To learn how to determine if Remicade is giving you side effects, read more from our Medical co-author.






-Step-17-Version-3.webp)


-Step-23.webp)


















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...