This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
This article has been viewed 17,272 times.
Diabetic retinopathy is a disease in which the blood vessels in the retina (which is located in the back of the eye) are weakened due to an imbalance in your blood sugar. This imbalance and weakening is caused by uncontrolled diabetes and it can result in blood and other fluids leaking into the eye, resulting in difficulty with vision and even loss of vision in severe cases. In order to treat diabetic retinopathy you will need to identify the condition, consult with a physician, and then follow your physician's suggestions for treatment.[1] The sooner you detect retinopathy, the better. It can be diagnosed and treated early with annual eye exams.
Steps
Getting Medical Treatment
-
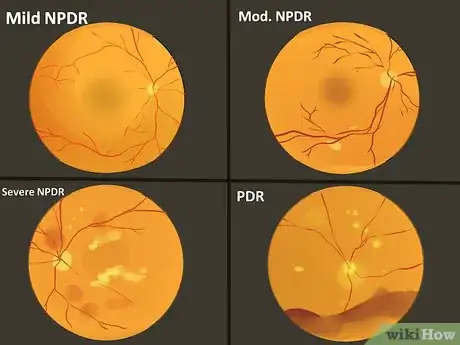
1Find out how serious your diabetic retinopathy is. There are four stages of diabetic retinopathy, with the first being the least severe and the fourth being the most severe. When you visit your optometrist, tell them that you have diabetes. They can perform a basic dilated eye exam. They may refer you to a more specialized eye doctor, an ophthalmologist, who can let you know how serious your condition is. Knowing what stage you are will help you to understand the severity of your condition and what steps will need to be taken to get your condition under control.[2] The stages are:[3]
- Mild nonproliferative diabetic retinopathy: At this stage there are small areas of weakness and bulging in the blood vessels. These are called microaneurysms. These microaneurysms may allow fluid to leak into the retina.
- Moderate nonproliferative retinopathy: At this stage the blood vessels are bulging and distorting. They may also become blocked or no longer move blood around the eye.
- Severe nonproliferative retinopathy: At this stage there are numerous blood vessels that have ruptured or are blocked. This causes a lack of blood supply to areas of the eye. When this occurs, the areas lacking blood supply begin to signal that new blood vessels should be established. However, these new blood vessels will grow weakly and in inappropriate areas, further damaging vision.
- Proliferative diabetic retinopathy (PDR): This is the advanced stage of diabetic retinopathy in which the eye begins growing replacement blood vessels that are not strong and located in areas that can impact your vision negatively. This usually includes the inside surface of the retina. At this stage there is usually excessive scar tissue, which can cause the retina to detach. This detachment can cause permanent blindness.
-
2Consult with your primary care physician. If you are having trouble maintaining your blood sugar and you are concerned that it might be affecting your vision, you should make an appointment with your doctor, in addition to your eye doctor. Getting your diabetes in control is an important part of treating diabetic retinopathy.
- Your primary care physician will help you to address the difficulty you are having with maintaining your blood sugar levels.
- Controlling your blood sugar is the best way to prevent diabetic retinopathy from occurring in the first place.
Advertisement -
3Control your blood sugar. Even if you and your doctor make a good plan for how you will control your blood sugar in the future, it is up to you to do so on a daily basis. Controlling your blood sugar include both taking your medication when you should and also maintaining a lifestyle that promotes a healthy blood-sugar level.[4]
- Lifestyle changes that you may need to make include changing your diet to eliminate spikes in your blood-sugar level, losing weight, and increasing the amount of exercise that you do.
-
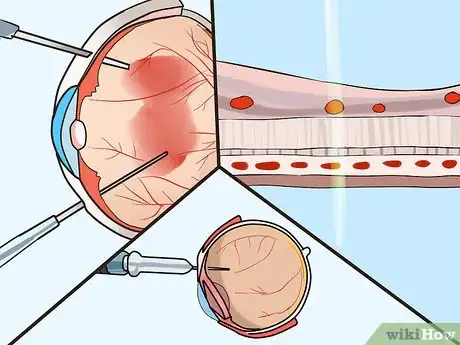
4Consider surgical treatment. If your diabetic retinopathy is advanced and affecting your vision, you may need to get surgery to save your eye sight. There are several types of surgery that may be suggested to you. Your eye doctor will suggest the treatment they think will be most helpful for your specific condition. The surgical procedures used to treat diabetic retinopathy include:[5]
- Medication injections: With this treatment, medication is injected straight into the back of the eye. This medication, usually a steroid, stops the eye from growing new weak and abnormal blood vessels. The procedure is done in a doctor's office and requires that the eye is dilated and numbed with anesthesia.
- Laser surgery: Laser surgery is used to shrink abnormal blood vessels and reduce swelling. It is usually done as an outpatient procedure in a doctor's office.
- Vitrectomy surgery: This type of surgery is done to remove scar tissue and blood vessels that have formed on the surface of the retina. This allows light into the retina, which in turn improves vision. This is a more invasive surgery than laser surgery and it needs to be performed in a surgical room or hospital. However, it usually done on an outpatient basis or with just a short hospital stay.
Identifying Diabetic Retinopathy
-
1Find out if you have diabetes. Diabetic retinopathy is a condition that only afflicts diabetics. If you are concerned about it, then the first step is to find out if you have diabetes. Go to your doctor and have them do a blood test to find out if you have diabetes. If you do not have diabetes, then you do not have diabetic retinopathy.[6]
- However, if you are having trouble with your sight you should see an eye doctor, no matter what your diabetic status is.
-
2Identify symptoms. Diabetic retinopathy affects your ability to see in a variety of ways. The fluid that builds up in the retina can blur your vision, it can cause you to see spots or floating shapes, and it can create a dark or empty space in the middle of your vision that you cannot see anything in. Also, diabetic retinopathy can make it difficult for you to see at night.[7]
- These symptoms could signal a variety of medical problems in your eyes. If you have any of them, you should make an appointment with an eye doctor to get checked out.
- Cataracts are also more common in people with diabetes. These can be detected early with an annual eye exam.
-
3Take your blood sugar level into consideration. If you know that you have diabetes and you are having problems with your sight, it is more likely to be diabetic retinopathy if you are having a hard time controlling your blood sugar.[8]
- Long periods of high blood sugar can cause fluid to build up in the eyes.
-
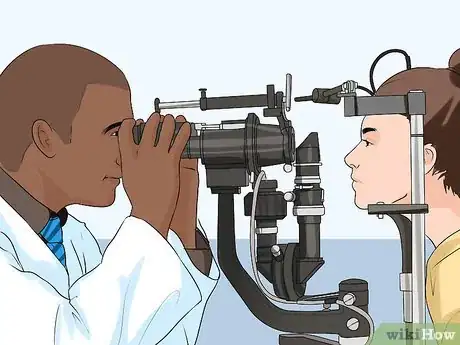
4See an eye doctor. If you are having trouble with your vision, you should make an appointment with an eye doctor immediately. They will discuss your symptoms with you, do a visual acuity test, measure the pressure in your eyes, inspect your eyes when they are dilated, and they may even do imaging tests of your eyes. These tests will allow them to diagnose, or rule out, diabetic retinopathy.[9]
- Everyone with diabetes should get an annual vision checkup that includes getting the eyes dilated. This lets the doctor see to the back of the eye, which allows them to inspect the retina and the optic nerve.
References
- ↑ http://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/diabetic-retinopathy?sso=y
- ↑ https://nei.nih.gov/health/diabetic/retinopathy
- ↑ https://www.nhs.uk/conditions/diabetic-retinopathy/stages/
- ↑ http://www.diabetes.org/living-with-diabetes/recently-diagnosed/living-with-type-1-diabetes.html?loc=lwd-slabnav
- ↑ https://www.aao.org/eye-health/diseases/diabetic-retinopathy-treatment
- ↑ http://www.diabetes.org/diabetes-basics/diagnosis/
- ↑ http://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/diabetic-retinopathy?sso=y
- ↑ http://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/diabetic-retinopathy?sso=y
- ↑ https://nei.nih.gov/health/diabetic/retinopathy































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...