This article was co-authored by Payam Daneshrad, MD and by wikiHow staff writer, Jennifer Mueller, JD. Dr. Payam Daneshrad is a board certified Otolaryngologist, a board eligible Facial Plastic Surgeon, and the Owner and Director of Daneshrad Clinic in Los Angeles, California. With over 19 years of experience, Dr. Daneshrad specializes in adult and pediatric Otolaryngology-head and neck surgery, packing-less nasal surgery, minimally invasive sinus surgery, and snoring treatment. He also uses the newest surgical ENT techniques for tonsillectomy, adenoidectomy, thyroidectomy, and parathyroidectomy. Dr. Daneshrad graduated with a BS and the highest honors from the University of California, Berkeley. He earned his Doctor of Medicine (MD) from Tulane University School of Medicine, where he was accepted into the AOA, the medical honor's society, and the Tulane University School of Public Health. Dr. Daneshrad received his medical training from the University of Southern California, where he currently serves as an Associate Clinical Professor. Dr. Daneshrad is the Otolaryngologist and Facial Plastic Surgeon for the Los Angeles Sparks and the athletic teams of Loyola Marymount University.
There are 12 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 9,652 times.
Meniere's disease is a rare inner-ear disorder that can cause vertigo, tinnitus, and hearing loss, along with a feeling of pressure in your ear. The disease can be scary because the symptoms come on suddenly and can last for several hours. However, symptoms often disappear for several years. Although there's no cure for Meniere's disease, there are medications and other treatments that can lessen the symptoms. If you experience any of the symptoms of Meniere's disease, make an appointment to see your doctor.[1]
Steps
Seeking Medical Treatment
-
1Recognize symptoms of Meniere's disease. Symptoms of Meniere's disease vary, so you may experience some or all of these symptoms. The important thing to notice is that symptoms come on suddenly. If you experience them once, you'll likely have a cluster of attacks for a few weeks. Common symptoms of Meniere's disease include:[2]
- Vertigo and dizziness for anywhere from a few minutes to several hours, with a sense of imbalance remaining for several days afterward
- Nausea and vomiting during a vertigo episode
- Pressure or fullness in one or both ears
- A ringing or buzzing in one or both ears (tinnitus)
- Difficulty hearing, especially low-pitched sounds
Tip: If you experience these symptoms, see your doctor as soon as possible. Although Meniere's disease is rare, many other conditions can also cause the same symptoms.
-
2Get hearing and balance assessments. Diagnosis of Meniere's disease requires at least 2 episodes of vertigo, hearing loss, and tinnitus or pressure in your ear. To evaluate these conditions, your doctor will ask you about your history of symptoms. They may refer you to an ear, nose, and throat specialist to conduct the following tests:[3]
- Audiometry: This hearing test evaluates how well you detect sounds at different pitches and volumes, as well as how well you can distinguish between similar sounding words.
- Videonystagmography (VNG): This test looks at your eye movement to assess your balance by looking at how well you can move your head while keeping your eyes focused on a single point.
- Rotary-chair testing: This test also measures your eye movement to assess your balance while you're sitting in a rotating chair.
- Vestibular evoked myogenic potentials (VEMP) testing: This test detects changes in your inner ear that are typical of people with Meniere's disease.
- Video head impulse test (vHIT): This test measures how well your eyes retain focus when your head is abruptly moved.
- Electrocochleography (ECoG): This test helps determine the buildup of fluid in your inner ear by evaluating how your inner ear responds to sounds.
Advertisement -
3Use blood tests and imaging scans to rule out other causes. Because the symptoms of Meniere's disease could also indicate many other conditions, your doctor will likely want to order additional tests before diagnosing Meniere's disease. Typically, another condition is more likely because Meniere's disease is so rare.[4]
- The same symptoms may also be present if you have frequent migraines, stroke, multiple sclerosis, or various heart or blood vessel diseases.[5]
- Occasionally, similar symptoms can be caused by a brain problem, such as a tumor. Although this is also rare, your doctor may order an MRI or CT scan of your brain just to rule it out before making a final diagnosis.[6]
-
4Take medication as prescribed during an attack. Your doctor or the specialist may prescribe medications that can help alleviate your symptoms during an attack. When you feel symptoms coming on, take the drug as quickly as possible.[7]
- Prochlorperazine may be prescribed if you have problems with vomiting or nausea during episodes of vertigo.
- Antihistamines may also be prescribed to treat vertigo, nausea, and vomiting.
- There's also a medication called betahistine that can reduce the frequency and severity of Meniere's attacks.
- Your doctor also may prescribe diuretics to reduce fluid retention, which can help your body regulate the volume of fluid in your inner ear.[8]
-
5Ask about middle ear injections to improve vertigo symptoms. If your symptoms don't improve with other medications, or if they get worse, your doctor can inject medication directly into your inner ear to help with vertigo. There are 2 types of treatment available:[9]
- Gentamicin: This antibiotic is toxic to your inner ear, forcing your unaffected ear to assume responsibility for balance. An injection of this drug runs the risk that you'll have further loss of hearing.
- Steroids: These drugs have helped control vertigo in some people. If they work for you, they may be preferable to gentamicin because there's a lower chance of additional hearing loss.
-
6Try a hearing aid to improve your hearing. If you have significant hearing loss, your doctor might refer you to an audiologist. The audiologist can examine your ear and perform hearing tests to find the best hearing aid for you.[10]
- Finding a hearing aid that works well for you can involve a little trial and error, so it's important to be patient. Hearing aids can also be difficult to adjust wearing if you're not accustomed to them.
-
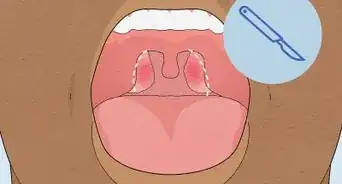
7Discuss surgery if your symptoms become severe. If your attacks become severe and debilitating and other treatments aren't helping, you might want to consider surgery. There are 3 procedures recommended for Meniere's disease:[11]
- Endolymphatic sac procedure: The endolymphatic sac is decompressed to drain excess fluid levels, which may reduce the feeling of fullness or pressure in your ear.
- Labyrinthectomy: The balance and hearing functions from the affected ear are removed completely. This procedure is generally only recommended if you already have total or near-total hearing loss.
- Vestibular nerve section: The nerve that connects the balance and movement sensors in your inner ear to your brain is cut. Usually, this procedure is successful at correcting problems with vertigo while keeping your hearing intact.
Making Lifestyle Changes
-
1Limit the amount of salt in your diet. Because salt encourages fluid retention in your body, decreasing the amount of salt you ingest may also help your body regulate the excess fluid in your ear. Avoid processed foods, which are typically high in sodium, and don't add salt to your food.[12]
- Check nutritional labels for sodium content. If you have Meniere's disease, you should eat less than 1,500 mg of sodium a day.
- People with Meniere's disease often notice improvement after simply decreasing the amount of salt in their diet.
Tip:Avoid monosodium glutamate (MSG), which contains sodium and can also contribute to fluid retention.
-
2Eat several small meals throughout the day. Eating food regularly throughout the day provides an even distribution of nutrients that can help your body regulate fluids and avoid fluid retention. Having a small amount of nutritionally balanced food every 2 or 3 hours may help decrease the fluid in your ear, leading to an improvement in your symptoms.[13]
- Try to eat at roughly the same amount of food at each meal and schedule your meals so that you're eating at the same times every day. Hunger can cause your body to retain fluid, which may worsen your symptoms.
-
3Avoid caffeine and alcohol. Caffeine and alcohol may increase the frequency or severity of your attacks. However, doctors don't know a lot about the connection between caffeine and alcohol and Meniere's disease. While these lifestyle changes may have no effect on your symptoms, they're at least worth a try for a month or two to see if you notice any difference.[14]
- If you don't want to quit caffeine and alcohol completely, at least work on minimizing your intake. For example, you might only have one cup of coffee in the morning instead of 2 or 3. If you notice improvement in your symptoms, you may want to decrease your intake further.
-
4Make a plan to quit smoking. Nicotine may cause Meniere's disease attacks to be more severe as well as more frequent. If you're a smoker, work with your doctor to craft a smoking cessation strategy that will allow you to quit in a healthy way.[15]
- Typically, it's easier to quit if you cut down gradually before quitting completely.
- Nicotine replacement therapy, such as gum, lozenges, or the patch, can also help. However, since the nicotine itself is thought to trigger attacks, you might not notice any decrease in the severity or frequency of attacks while you're on nicotine replacement therapy.
-
5Use relaxation techniques to cope with stress and anxiety. A professional therapist or counselor can help you identify stress or anxiety triggers that might be causing Meniere's attacks. Learning healthy coping mechanisms for dealing with stress and anxiety might diminish your attacks.[16]
- In some situations, a psychiatrist might recommend medication to treat anxiety or depression. These medications help reduce the frequency and severity of Meniere's attacks for some people.[17]
Trying Alternative Therapies
-
1Use sound therapy to reduce the effects of tinnitus. If you have tinnitus caused by Meniere's disease, sound therapy might help diminish this symptom. Because the effects of tinnitus tend to be more obvious in times of quiet, sound therapy fills silence with white noise and neutral sounds to distract you from the ringing or buzzing in your ear.[18]
- You can practice sound therapy at home simply by opening a window to bring in sounds from outside or leaving on a radio or television in the background. You can also use sound generators that produce natural sounds or white noise.
- There are also sound apps available for smartphones if you need to take your sound therapy on the go.[19]
Tip: Because tinnitus can be stressful, relaxation techniques such as deep-breathing exercises or practicing yoga may also help.
-
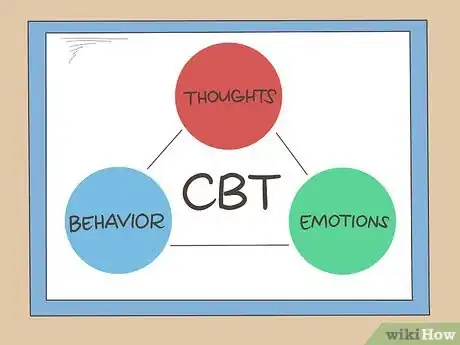
2Break the symptom cycle with cognitive behavioral therapy (CBT). The intrusive symptoms of Meniere's disease typically have a psychological impact. They may cause changes in your behavior or cause you to have negative thoughts or stress out. These thoughts and feelings, in turn, aggravate your symptoms. CBT works to break down the connection between your symptoms and your negative coping strategies.[20]
- By replacing negative coping strategies with more positive ones, you can learn to better manage attacks when they arise. Because you're better able to cope with your symptoms, you may find that they seem less severe.
-
3See a physiotherapist to improve your balance. Vestibular rehabilitation (VRT) consists of special exercises that teach you to use signals from your eyes, ankles, legs, and neck to maintain balance, rather than relying on the signals coming from the inner ear. These exercises make it easier to cope with vertigo so it has less of an impact on your life. Typically, you'll be referred to a physiotherapist who has special training in VRT.[21]
- There are also VRT booklets and videos that you can use to practice these exercises on your own. However, discuss this with your doctor before you go the self-help route.
-
4Try positive pressure therapy to improve vertigo symptoms. This therapy applies pressure to your middle ear to lessen fluid buildup using a device called a Meniett tube. The treatment is still in development and improves the symptoms of vertigo and tinnitus in some, but not all, patients.[22]
- If you and your doctor decide to try this treatment, your doctor will show you how to use the device. Then, you'll take the device home with you and perform the treatment yourself, usually for about 5 minutes 3 times a day.
References
- ↑ https://www.nhsinform.scot/illnesses-and-conditions/ears-nose-and-throat/menieres-disease
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/menieres-disease
- ↑ https://www.medstarhealth.org/services/hearing-balance-tests
- ↑ https://www.american-hearing.org/disease/menieres-disease/
- ↑ https://www.uspharmacist.com/article/menieres-disease-treatment-strategies
- ↑ https://stanfordhealthcare.org/medical-conditions/ear-nose-and-throat/menieres-disease/diagnosis.html
- ↑ https://www.nhsinform.scot/illnesses-and-conditions/ears-nose-and-throat/menieres-disease#treating-menieres-disease
- ↑ https://www.uspharmacist.com/article/menieres-disease-treatment-strategies
- ↑ https://www.nhs.uk/conditions/menieres-disease/
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/ears-menieres-disease
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/ears-menieres-disease
- ↑ https://www.uspharmacist.com/article/menieres-disease-treatment-strategies
- ↑ https://www.uspharmacist.com/article/menieres-disease-treatment-strategies
- ↑ https://www.health.harvard.edu/a_to_z/menieres-disease-a-to-z
- ↑ https://www.uspharmacist.com/article/menieres-disease-treatment-strategies
- ↑ https://www.uspharmacist.com/article/menieres-disease-treatment-strategies
- ↑ https://www.nhsinform.scot/illnesses-and-conditions/ears-nose-and-throat/menieres-disease#treating-menieres-disease
- ↑ https://www.nhsinform.scot/illnesses-and-conditions/ears-nose-and-throat/menieres-disease#treating-menieres-disease
- ↑ https://www.nhsinform.scot/illnesses-and-conditions/ears-nose-and-throat/tinnitus#treating-tinnitus
- ↑ https://www.nhsinform.scot/illnesses-and-conditions/ears-nose-and-throat/menieres-disease#treating-menieres-disease
- ↑ https://www.nhsinform.scot/illnesses-and-conditions/ears-nose-and-throat/menieres-disease#treating-menieres-disease
- ↑ https://www.cochrane.org/CD008419/ENT_positive-pressure-therapy-for-menieres-disease-or-syndrome





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...