This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 31 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 84% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 94,888 times.
Research shows that post-herpetic neuralgia (PHN) is an extremely painful condition that sometimes occurs following the herpes zoster (shingles) virus.[1] This PHN pain occurs in the areas on the body where the shingles rash was present. Generally, this pain follows a nerve’s path on one side of the body. While a painful, itchy blistering rash is the main characteristic of shingles, this nerve pain may precede its appearance. Quite frequently, the earliest symptom of shingles is a burning or tingling sensation on the skin. Experts note that the best way to treat this nerve pain is to heal your shingles, control your pain, and decrease your risk of complications.[2]
Steps
Reducing Pain and Itching
-
1Try to keep from scratching at your blisters. As difficult as it may be, leave your blisters alone and avoid scratching. They will crust over and then fall off on their own. If you scratch them, they will open up and become more susceptible to infection.[3]
- You will also spread bacteria with your hands if you scratch at the blisters. If this does happen inadvertently, always wash your hands afterward to stay hygienic.
-
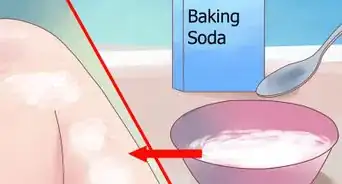
2Use a baking soda paste to reduce irritation. Baking soda has a pH greater than 7 (making it alkaline), giving it the ability to neutralize the chemical that creates the itching sensation. The chemical creating the itching sensation is acidic with a pH that is less than 7.[4]
- Apply a paste made of 3 teaspoons baking soda mixed with 1 teaspoon of water. This relieves itching and helps the blisters dry out quicker.
- You can apply this paste as often as needed to relieve the itching.
Advertisement -
3Apply a cold compress to your blisters. Use a cool, moist compress to ease discomfort. You can apply this compress for up to 20 minutes at a time, several times a day.[5]
- You can make a cold compress by wrapping an ice block in a clean towel and pressing it against your skin. Alternatively, you can use a bag of frozen vegetables. Just make sure not to put it directly on your skin and not to keep it on your skin for more than 20 minutes at a time as both of these conditions can lead to tissue damage.
-
4Spread Benzocaine cream on your blisters after you remove the cold compress. Apply a topical cream, such as nonprescription benzocaine cream, directly after your cool compress application. Benzocaine works as an anesthetic, numbing the nerve endings in the skin.[6]
- As an alternative, talk to your doctor about prescription 5% Lidocaine patches. You can apply the patch to the area where you're experiencing the pain, as long as your skin is intact. You can apply as many as 3 patches at once. You can wear your patches for up to 12 hours in a 24 hour period.
Dealing with Infected Sores
-
1Look out for signs that your sores are infected. Infected sores are bad news, so if you think that your sores may be infected, you should contact your doctor immediately.[7] Signs that your sores are infected include:
- A fever
- An increase in inflammation that causes additional pain
- The sore feels warm to the touch
- The sore is shiny and smooth
- Your symptoms are getting worse
-
2Soak your infected sores in Burow’s solution. You can soak any infected sores in Burow’s solution (commercial name, Domeboro) or tap water. This helps to decrease oozing, clean away any crusting and soothe the skin.[8]
- Burow’s solution has antibacterial and astringent properties. You can purchase it without a prescription at your local pharmacy.
- Instead of soaking your sores, you can also apply the Burow’s solution directly onto your sores via the cold compress. You can apply the compress for up to 20 minutes, several times a day.
-
3Apply capsaicin cream after your blister has crusted over. Once a lesion has crusted over, you can apply capsaicin cream (e.g. Zostrix) to it. You can apply the capsaicin cream up to 5 times a day in order to promote healing.[9]
Taking Medications After the Blisters are Gone
-
1Use a lidocaine patch. After the blisters have healed, you can apply a 5% lidocaine patch to your skin to reduce nerve pain. The lidocaine patch provides effective pain relief without the risk of negative side effects.[10]
- These are available at most pharmacies and online. Stronger patches may be available through your doctor.
-
2Take non-steroidal, anti-inflammatory drugs to ease your pain. Non-steroidal anti-inflammatory medications (NSAIDs) are often prescribed in addition to other narcotic medications in order to boost pain relief. They are inexpensive and odds are you already have at least one in your bathroom cabinet.[11]
- Examples of NSAIDs include acetaminophen, ibuprofen or indomethacin. These medications can be taken up to three times per day – just be sure to follow the label for instructions on the appropriate dosage for you.
-
3Try corticosteroids to relieve your nerve pain. Corticosteroids are often prescribed for relatively healthy elderly people who present with moderate to severe nerve pain. The corticosteroids are often prescribed in addition to antiviral medications.[12]
- Talk to your doctor about this option. Effective (that is, stronger) corticosteroids are available by prescription only.
-
4Talk to your doctor about taking narcotic analgesics. Narcotic analgesics are sometimes prescribed to treat severe nerve pain caused by shingles. However, narcotics only provide symptomatic relief – they do not treat the cause of the pain.[13]
- In addition, narcotics are addictive substances which the patient can quickly become dependent on. Therefore their use must be carefully monitored by a physician.
-
5Get a prescription for tricyclic antidepressants. Sometimes tricyclic antidepressants are prescribed to treat specific types of nerve pain caused by shingles. Although their exact mechanism is unknown, they work by blocking pain receptors in the body.[14]
-
6Take anti-epileptic drugs to treat nerve pain. Antiepileptic drugs are widely used in pain clinics to treat neuropathic pain. There are many types of antiepileptic drugs, such as phenytoin, carbamazepine, lamotrigine and gabapentin, any of which may be prescribed to treat nerve pain in shingles patients.[15]
- For the above two steps, your doctor will know if these are viable treatments for you. In general, these two are reserved for more serious cases of nerve pain.
Treating Nerve Pain with Surgical Procedures
-
1Get an alcohol or phenol injection. One of the simplest surgical techniques for relieving nerve pain is an injection of alcohol or phenol into the peripheral branch of the nerve. This causes permanent damage to the nerve, thus helping to prevent pain.[16]
- This is a procedure done by a medical professional. Your health history and condition will determine if this is a suitable route to pursue.
-
2Try transcutaneous electrical nerve stimulation (TENS). This treatment involves the placement of electrodes over the nerves that are causing the pain. These electrodes deliver tiny, painless electrical impulses to nearby nerve pathways.[17]
- Exactly how these impulses relieve pain is uncertain. One theory is that the impulses stimulate the production of endorphins, your body’s natural painkillers.
- Unfortunately, this treatment doesn’t work for everyone, but it tends to be more effective if it is given in conjunction with a drug called pregabalin.
-
3Consider spinal cord or peripheral nerve stimulation. These devices are similar to TENS, but are implanted ‘’underneath’’ the skin. Like TENS units, you can turn these units on and off as needed to control pain.[18]
- Before the device is surgically implanted, doctors do a trial first using a thin wire electrode. The trial is done to ensure that the stimulator will provide effective pain relief.
- The electrode is inserted through your skin into the epidural space over the spinal cord for a spinal cord stimulator, or under your skin above a peripheral nerve in the case of a peripheral nerve stimulator.
-
4Talk to your doctor about pulsed radiofrequency lesioning (PRF). This a very safe and effective form of pain relief that uses radiofrequency to modulate pain at a molecular level. After a single treatment, the pain relief can last for up to 12 weeks.
Combating Shingles Before It Appears
-
1Know the symptoms of shingles. Shingles first presents as pain, itching and tingling of the skin. Sometimes these initial symptoms are followed by confusion, fatigue, fever, headache, memory loss, an upset stomach and/or stomach pain.[19]
- Up to five days after the appearance of these initial symptoms, a painful rash may appear on one side of the face or body.
-
2Visit your doctor within 24 to 48 hours if you think you have shingles. If you think you have shingles, visit your physician within 24 to 48 hours. Antiviral drugs like famciclovir, valtrex and acyclovir can be used to effectively treat the symptoms of shingles, but only if they are started within 48 hours of onset.[20] [21] [22]
- If you begin taking your antiviral medication after 48 hours, it may not be as effective. Additionally, keep in mind that your antivirals won't prevent PHN.
-
3Use a topical medication to clear the shingles up before they get worse. In addition to antiviral medications, your physician may prescribe a topical medication, such as caladryl. Caladryl may help your already open lesions by reducing pain and itching.
- Caladryl works by interfering with the pain signals the nerves send to the brain and is available in gel, lotion, spray or stick form.
- Caladryl may be applied every 6 hours, up to 4 times a day. You need to wash and dry the affected area prior to application.
- As another option, ask your doctor about prescription 5% Lidocaine (Lipoderm) adhesive patches. You can apply the patches to intact skin to help manage your pain.
- For an over-the-counter option, use capsaicin cream (Zostrix, Zostrix HP). Apply the cream to intact skin 3 to 4 times per day. The cream may cause a burning or stinging sensation when you apply it, but this side effect should go away. If it doesn't, stop using the cream. Be sure to wash and dry your hands thoroughly after you apply the cream.[23]
-
4Talk to your doctor about oral medications for PHN. Your doctor can prescribe gabapentin (Neurontin) or pregabalin (Lyrica) to help manage your PHN symptoms. You can use the medication for up to 6 months, though your doctor will taper you off early if your symptoms go away before the 6 month mark. Do not stop taking the medication suddenly. Your doctor will help you taper off of it.
- All drugs have side effects. Possible side effects of these medications include memory issues, sedation, electrolyte imbalances, and liver issues. Talk to your doctor if you experience any side effects.[24]
-
5Ask your doctor if corticosteroid therapy is right for you. If you have moderate to severe pain caused by your outbreak, your doctor may prescribe the oral corticosteroid prednisone, along with acyclovir. Corticosteroid therapy may reduce your nerve pain, but it doesn't work for everyone.[25]
- Your doctor will only prescribe corticosteroids if you aren't taking medications that interact with them. Make sure you tell your doctor about any other medications you are taking.
- For example, your doctor might prescribe up to 60 mg of prednisone for up to 10-14 days, tapering you off before you stop taking the medication.
Expert Q&A
Did you know you can get expert answers for this article?
Unlock expert answers by supporting wikiHow
-
QuestionCan a heat pad/source help?
 Luba Lee, FNP-BC, MSLuba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
Luba Lee, FNP-BC, MSLuba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
Board-Certified Family Nurse Practitioner
-
QuestionHow do I prevent getting shingles a second time?
 Luba Lee, FNP-BC, MSLuba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
Luba Lee, FNP-BC, MSLuba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
Board-Certified Family Nurse Practitioner Anyone who has experienced one or more shingles breakout is at risk for another one. Your immunity from the virus diminishes over time, so your risk remains. Getting a Zoster vaccine can provide added protection, so ask your doctor when the right time to get vaccinated is. There is no specified time to get vaccinated after a breakout, so your doctor will make a recommendation based on your medical history.
Anyone who has experienced one or more shingles breakout is at risk for another one. Your immunity from the virus diminishes over time, so your risk remains. Getting a Zoster vaccine can provide added protection, so ask your doctor when the right time to get vaccinated is. There is no specified time to get vaccinated after a breakout, so your doctor will make a recommendation based on your medical history.
Warnings
- If you suspect you may have shingles, it is essential that you speak with your physician and get your pain managed as soon as possible. Doing so could prevent nerve damage. The nerve damage is what causes the pain that continues for months or even years.⧼thumbs_response⧽
References
- ↑ https://www.nhs.uk/conditions/post-herpetic-neuralgia/
- ↑ https://my.clevelandclinic.org/health/diseases/12093-postherpetic-neuralgia#management-and-treatment
- ↑ https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=uh3267
- ↑ https://myhealth.alberta.ca/Health/aftercareinformation/pages/conditions.aspx?hwid=uh3267
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/shingles
- ↑ https://www.northshore.org/healthresources/encyclopedia/encyclopedia.aspx?DocumentHwid=hw75433
- ↑ https://my.clevelandclinic.org/health/diseases/11036-shingles
- ↑ https://emedicine.medscape.com/article/1132465-treatment#d7
- ↑ https://dermnetnz.org/topics/capsaicin
- ↑ https://medlineplus.gov/druginfo/meds/a603026.html
- ↑ https://www.aafp.org/pubs/afp/issues/2005/0915/p1082.html
- ↑ https://www.aafp.org/pubs/afp/issues/2000/0415/p2437.html
- ↑ https://www.aafp.org/pubs/afp/issues/2000/0415/p2437.html
- ↑ https://www.aafp.org/pubs/afp/issues/2000/0415/p2437.html
- ↑ https://www.aafp.org/pubs/afp/issues/2000/0415/p2437.html
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK525978/
- ↑ https://my.clevelandclinic.org/health/treatments/15840-transcutaneous-electrical-nerve-stimulation-tens
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK539703/
- ↑ https://www.cdc.gov/shingles/about/symptoms.html
- ↑ http://reference.medscape.com/drug/valtrex-valacyclovir-342631
- ↑ http://reference.medscape.com/drug/zovirax-acyclovir-342601
- ↑ http://reference.medscape.com/drug/famvir-famciclovir-342611
- ↑ https://www.aafp.org/afp/2000/0415/p2437.html
- ↑ https://www.aafp.org/afp/2000/0415/p2437.html
- ↑ https://www.aafp.org/afp/2000/0415/p2437.html
- MacFarlane BV, Wright A, O'Callaghan J, Benson HA. Chronic neuropathic pain and its control by drugs. Pharmacol Ther. 1997; 75:1–19.
- Rowbotham MC, Davies PS, Verkempinck C, Galer BS. Lidocaine patch: Double blind controlled study of a new treatment method for post-herpetic neuralgia. Pain. 1996; 65:39–44.
- AE Yakovlev, A. P. (2007 Oct;). Peripheral nerve stimulation in treatment of intractable postherpetic neuralgia. Neuromodulation. , 10(4):373-5. doi: 10.1111/j.1525-1403.2007.00126.x.
- Arora, D. B. (2000). Textook of Microbiology. DELHI: CBS Publishers .
- Davies, P., & Galer, B. ( 2004). Review of lidocaine patch 5% studies in the treatment of postherpetic neuralgia. Drugs , 64(9):937-47.
- Haslet, C., Chivlers, E. R., Boon, N. A., & Colledge, N. R. (2002). Davidson's Principles and Practice of Medicine. london: Churchill Livingstone.
- Longo, D. L., Kasper, D. L., Jameson, J. L., Fauci, A. S., Hauser, S. L., & Loscalzo, J. (2012). Harrison's Principles Of Medicine. new york: McGraw-Hill.
- M Barbarisi, M. P. ( 2010 Sep). Pregabalin and transcutaneous electrical nerve stimulation for postherpetic neuralgia treatment. Clin J Pain. , 26(7):567-72. doi: 10.1097/AJP.0b013e3181dda1ac.
- Ryder, S.-A., & Stannard, C. F. (2005). Treatment of chronic pain: antidepressant, antiepileptic and antiarrhythmic drugs. Contin Educ Anaesth Crit Care Pain , 5 (1): 18-21.
- Saru Singh, R. G. (2013 ). Post-herpetic neuralgia: A review of current management strategies. Indian J Pain [serial online] , 27:12-21.
- Tripathi, K. (2001). Essentials of Medical Pharmacology. NEW DELHI: Jaypee Brothers Medical Publishers.
About This Article
If your shingles has caused nerve pain, there are several ways you can control your discomfort and itching. As hard as it may be, avoid scratching your blisters, which will open them up and make them more susceptible to infection. To reduce irritation and itching, make a paste out of 3 tablespoons of baking soda mixed with 1 teaspoon of water. Apply the paste as often as needed to your blisters or any itchy areas. You can also apply a cool, moist compress to your blisters for up to 20 minutes at a time, several times a day. After you remove the cold compress, spread benzocaine cream on your blisters. This will act as an anesthetic, numbing the nerve endings in the skin. For more tips from our Medical co-author, including how to deal with infected sores, keep reading!























-Step-13.webp)






















































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...