This article was medically reviewed by Erik Kramer, DO, MPH and by wikiHow staff writer, Jennifer Mueller, JD. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 21 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 7,889 times.
If you've ever sat in the same position for too long and had a foot or leg "fall asleep," you're familiar with the symptoms of paresthesia, described as a prickling or tingling sensation. Paresthesia usually affects your extremities, including your legs, arms, feet, and hands, and is often no cause for concern.[1] Acute paresthesia, such as when your foot falls asleep, can usually be treated at home and will go away relatively quickly. However, chronic paresthesia might itself be a symptom of some other disease or condition. If you experience paresthesia that occurs more frequently or regularly, talk to your doctor. While there are some at-home treatments and alternative (or "complementary") therapies that can help with chronic paresthesia, the recommended treatment typically depends on the underlying cause. You'll get more effective treatment options if you're diagnosed quickly.[2]
Steps
Alleviating Acute Paresthesia
-
1Switch to a different position. The most common cause of paresthesia is pressure on a nerve. Once that pressure is gone, paresthesia typically dissipates on its own. It might help to shake the limb or move the joint around to help resume blood flow in the area.[3]
- For example, if you were sitting with your knee bent and your ankle under your other leg, your leg might have fallen asleep. Stretch out your leg and rotate your ankle to regain sensation.
Tip: Gently massaging the affected area might also help the symptoms go away. However, don't massage the area if it's painful to do so.[4]
-
2Adjust the temperature in the room. If you're unusually hot or unusually cold, you might experience paresthesia. Typically, the symptoms will resolve if you correct the temperature discrepancy.[5]
- For example, if you're cold, you might turn on a source of heat, put on a sweater, or wrap up in a blanket. If you're hot, try using an ice pack to cool down or stand in front of a fan.
Advertisement -
3Rub capsaicin cream on the affected area to alleviate pain. You can buy capsaicin creams at pharmacies and discount stores or online. The active ingredient in these creams, capsaicin, is the substance that gives chili peppers their heat. This chemical interacts with your nervous system to block nerves from sending signals to the brain.[6]
- Capsaicin cream works best if you experience pain in addition to the "pins and needles" feeling of paresthesia. It's safe to rub the cream on the affected area 3 or 4 times a day.
- When you use capsaicin cream, you may experience a burning sensation on your skin. Your skin may also become inflamed or irritated. If this becomes uncomfortable, stop using the cream.
-
4Exercise and maintain a healthy weight to improve your circulation. Getting regular exercise, particularly cardiovascular exercise, can make it less likely that you'll experience acute instances of paresthesia. If you're overweight, work with your doctor to develop a plan to lose weight. You won't have to lose much to notice a difference.[7]
- If you've lived a relatively sedentary life and are just getting started with exercise, consult your doctor first. They'll recommend some activities that are safe for you to do and put you on the road to physical fitness with less risk of injury.
- In the meantime, sit and stand in ways that relieve pressure on your limbs. For example, if you find that when you cross your legs, the one underneath often falls asleep, try sitting with your legs extended or your feet propped up on something.
Dealing with Chronic Paresthesia
-
1Seek immediate medical treatment if you have severe pain. Paresthesia that is accompanied by severe pain may indicate a more serious underlying problem with your nerves. While this situation can be scary, try to remain calm and describe your symptoms to the doctor. This will help them better understand your condition and figure out how best to proceed.[8]
- Likewise, if you experience uncontrolled movements, such as jerking or twisting of the affected limb, there might be a more serious problem that needs immediate care.
Warning: If you experience paresthesia along with slurred speech, facial drooping, or weakness, call the emergency number (911 in the US) immediately. These are symptoms of a stroke.[9]
-
2Take an anti-inflammatory medication to relieve mild symptoms. Over-the-counter anti-inflammatory medications, including aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, can help with recurring paresthesia. If you take over-the-counter medications, follow the dosage instructions on the package.[10]
- If you find that you're taking over-the-counter medications for more than 3 days in a row, contact a doctor. These medications can cause problems if you take them on a regular basis. If you need to take them frequently to manage your symptoms, there's likely a better way to do so.[11]
-
3Try acupuncture to ease neuropathic pain. If your paresthesia is chronic and painful, you might benefit from a series of acupuncture treatments. Ask your doctor or another medical professional if they think acupuncture would work for you.[12]
- You typically won't notice results until you've had several acupuncture treatments over a month or so. An acupuncture practitioner can give you a better idea of how many treatments you need based on your condition and the cause of your paresthesia.
Warning: Acupuncture is unregulated in many areas. Research practitioners thoroughly or ask your doctor or other healthcare providers for a recommendation.
-
4Use massage therapy to improve circulation and nerve functioning. Therapeutic massage of the affected limbs can help alleviate paresthesia over time. Typically, it takes several sessions with a massage therapist over the course of a few weeks to a month before you'll notice any significant change.[13]
- Tell the massage therapist that you've been experiencing paresthesia. Give them a background of your symptoms and explain the circumstances under which your episodes of paresthesia most frequently occur.
- Generally, you'll get better results if you go to a massage therapist who has experience with neuropathy massage therapy and has worked with patients who have paresthesia.
Handling Paresthesia Caused by Another Condition
-
1Evaluate your medical history for potential causes of paresthesia. Chronic paresthesia is often caused by another condition. Provide a full medical history to your doctor so they can more quickly diagnose the underlying cause. Without this diagnosis, you're likely to have more flare-ups. Potential causes of paresthesia include:[14]
- Joint conditions, such as arthritis or carpal tunnel syndrome
- Previous stroke or traumatic brain injury (TBI)
- Metabolic disorders, including diabetes mellitus and hypothyroidism
- Shingles
- Migraines
- Menopause
- History of alcoholism
- Lyme disease
- Heavy metal poisoning
Tip: Make sure you also tell your doctor about all medications and nutritional supplements you're taking, including the dosage and frequency. Some medications may cause paresthesia as a side effect.
-
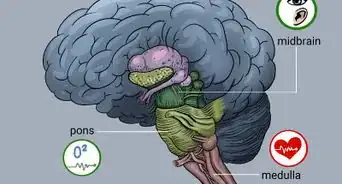
2Undergo laboratory tests to narrow down the potential causes. Generally, it's difficult to diagnose the cause of paresthesia without lab testing. Because a vitamin B deficiency can cause paresthesia,[15] your doctor may order blood tests to check your vitamin levels. In addition, you may need to get the following tests:[16]
- X-ray, MRI, or CT scan: These tests produce images that can help your doctor identify nerve damage in the area where you have paresthesia.
- Nerve conduction (EMG) studies: Your doctor uses these tests to evaluate your nerve function and determine if they're sending signals properly, which could be causing your paresthesia.
-
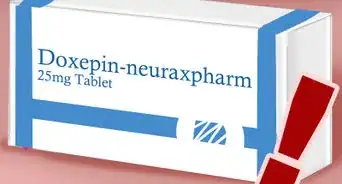
3Talk to your doctor about treatment with anti-depressive medication. Antidepressants, such as amitriptyline, may help chronic paresthesia. While the idea of taking an anti-depressant may seem worrisome, these medications are typically prescribed in much lower doses than they would be to treat depression. Although they don't decrease the pain itself, they do alter your perception of the pain so that it hurts less.[17]
- Common side effects of amitriptyline include dry mouth, dizziness, nausea, headache, and constipation.[18] Let your doctor know if you have any side effects that you find troublesome or that interfere with your normal life.
- Depending on the cause of your paresthesia, your doctor might also prescribe the immune-suppressant prednisone.[19] Some also find relief with anticonvulsant medications, such as gabapentin or Gabitril.[20]
- Other medications that may work for your paresthesia are gabapentin and lyrica.[21]
-
4Keep a food diary to determine if some foods exacerbate symptoms. If you notice that you get paresthesia after eating, there may be specific foods that are causing it. This is particularly common if you've already been diagnosed with diabetes[22] or multiple sclerosis (MS).[23] [24]
- In your food diary, write down the exact foods and quantities that you eat. If you experience paresthesia, write down the time that the symptoms occur along with a description of the specific symptoms and how they came on (suddenly or gradually).
- For example, you might write: "6:00 a.m. breakfast: 1 banana, 2 scrambled eggs, 1 slice toast." If you experienced paresthesia an hour later, you might write: "Numbness and tingling in right leg. Came on suddenly while waiting for coffee. Shaking it didn't help but feeling did return after about 5 minutes."
- After a couple of weeks, look at your food diary and see if you notice any particular triggers. Eliminate these foods from your diet and see if the paresthesia stops.
- If there's more than one food that could be a potential trigger, only eliminate one food at a time. Wait about 2 weeks before you eliminate another food. If there's no change in your paresthesia, food likely isn't the culprit.
-
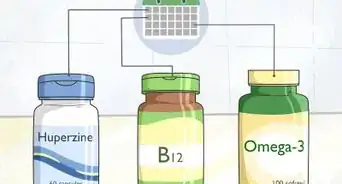
5Take vitamin supplements if you are deficient in vitamin B. Vitamin B, particularly B12, helps your nerves to function properly. Typically, you’ll have an abnormal gait, or you may lose the sense of position and vibration in your feet. If a blood test reveals that you have a vitamin B deficiency, your doctor may recommend supplements. After correcting the deficiency, you should notice fewer episodes of paresthesia.[25]
- Be careful to take vitamin supplements only as directed by your doctor. An overdose of vitamin B6 can actually cause paresthesia, so supplements might do more harm than good if not taken appropriately.[26]
- Low B12, which can cause chronic paresthesia, is common in people who have multiple sclerosis (MS). If you've been diagnosed with MS, get your vitamin levels tested frequently.[27]
- You will also need to have homocysteine and methylmalonic acid labs if you come back positive for a B12 deficiency.[28]
-
6Get physiotherapy to relieve your paresthesia and restore limb function. Some conditions, such as carpal tunnel syndrome, may limit the use of your limbs. Your doctor might recommend physiotherapy to help. A physiotherapist will evaluate your condition and develop a plan of stretches and exercises to help improve your condition.[29]
- Physiotherapy may involve other treatments in combination with exercises, depending on the specific cause of your paresthesia and the overall condition of your limbs. For example, if you have paresthesia as a result of carpal tunnel syndrome, the physiotherapist might recommend splinting your wrists while doing repetitive activities with your hands.
Warnings
- Avoid consuming alcohol if you regularly experience paresthesia. If you do drink, do so only occasionally and in moderation.[30]⧼thumbs_response⧽
- If you notice any loss of sensation, avoid potentially unsafe activities, such as cooking or driving, until sensation has returned.⧼thumbs_response⧽
References
- ↑ https://www.ninds.nih.gov/Disorders/All-Disorders/Paresthesia-Information-Page
- ↑ https://www.disabled-world.com/health/neurology/paresthesia.php
- ↑ https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=1&ContentID=58
- ↑ https://www.healthdirect.gov.au/limb-numbness
- ↑ https://www.msfocusmagazine.org/Magazine/Magazine-Items/13-Points-about-Paresthesia
- ↑ https://www.nhs.uk/conditions/peripheral-neuropathy/treatment/
- ↑ https://my.clevelandclinic.org/health/diseases/15631-autonomic-neuropathy-or-autonomic-dysfunction-syncope-information-and-instructions
- ↑ https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=1&ContentID=58
- ↑ https://www.stroke.org/en/about-stroke/stroke-symptoms
- ↑ https://www.disabled-world.com/health/neurology/paresthesia.php
- ↑ https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/medications-non-steroidal-anti-inflammatory-drugs
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5733739/
- ↑ https://www.foundationforpn.org/living-well/integrative-therapies/massage/
- ↑ https://www.disabled-world.com/health/neurology/paresthesia.php
- ↑ https://www.health.harvard.edu/blog/vitamin-b12-deficiency-can-be-sneaky-harmful-201301105780
- ↑ https://www.drugs.com/cg/paresthesia.html
- ↑ https://www.disabled-world.com/health/neurology/paresthesia.php
- ↑ https://www.frontiersin.org/articles/10.3389/fneur.2017.00307/full
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK534809/
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/in-depth/pain-medications/art-20045004
- ↑ https://www.mayoclinic.org/diseases-conditions/peripheral-neuropathy/in-depth/pain-medications/art-20045004
- ↑ https://www.hopkinsmedicine.org/health/conditions-and-diseases/diabetes/diabetic-neuropathy-nerve-problems
- ↑ https://www.msfocusmagazine.org/Magazine/Magazine-Items/13-Points-about-Paresthesia
- ↑ https://www.aafp.org/afp/2008/0615/p1678.html
- ↑ https://ssl.adam.com/content.aspx?productid=117&pid=1&gid=003206&site=makatimed.adam.com&login=MAKA1603
- ↑ https://www.disabled-world.com/health/neurology/paresthesia.php
- ↑ https://www.msfocusmagazine.org/Magazine/Magazine-Items/13-Points-about-Paresthesia
- ↑ https://www.aafp.org/afp/2003/0301/p979.html
- ↑ https://www.physio.co.uk/what-we-treat/musculoskeletal/symptoms/tingling-pins-and-needles.php
- ↑ https://my.clevelandclinic.org/health/diseases/15631-autonomic-neuropathy-or-autonomic-dysfunction-syncope-information-and-instructions



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...