This article was medically reviewed by Erik Kramer, DO, MPH and by wikiHow staff writer, Christopher M. Osborne, PhD. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 10 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 17,188 times.
A radiation burn, also called a cutaneous radiation injury (CRI), is a serious medical condition, but thankfully also a rare one. Patients are often unaware of their radiation exposure and develop unexplained burn symptoms, which should be treated medically like other types of serious skin burns. While not technically CRIs, cancer patients who undergo radiation therapy are likely to develop skin damage in the treatment area that can resemble skin burns. If this happens to you, follow your care team’s advice and take practical measures to avoid further skin irritation.
Steps
Treating a Cutaneous Radiation Injury (CRI)
-
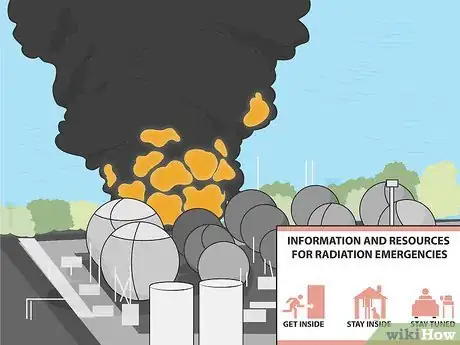
1Follow official health and safety orders during a radiation emergency. If you get caught up in a radiation emergency, such as a nuclear accident, an act of war or terrorism, or some other serious radiation event, quick action is essential. In many cases, any symptoms of acute radiation syndrome (ARS) won’t be immediate, but it’s critical that you follow governmental and/or medical orders right away.[1]
- You may, for example, be advised to remove and bag up any clothing, shower thoroughly, and seal yourself indoors. You may also be ordered to evacuate with very short notice.
- Any burns that appear immediately due to a radiation emergency are likely to be thermal burns rather than radiation burns. These should be treated like serious burns in general—by removing clothing that isn’t burned in place, applying cool, damp coverings to the wound, and getting emergency help as soon as possible.
-
2Seek emergency medical care for burns that appear with no known cause. The first signs of a radiation burn often don’t appear for several days after exposure, meaning the cause isn’t always obvious. If you show unexplained signs of a burn like swelling, redness, pain, bleeding, and/or ulceration, seek medical help right away.[2]
- While radiation burns can occur due to acute radiation exposure, they’re often caused by beta radiation or low energy X-rays. These sources of radiation tend not to penetrate as deeply into the body, meaning you may not be immediately aware that you were exposed to radiation.
- Radiation burns may be diagnosed through a process of elimination that rules out other sources of burns, along with medical investigation of the likely radiation source.
Advertisement -
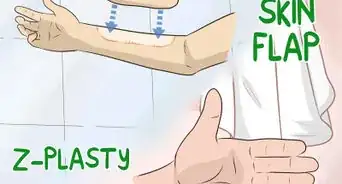
3Undergo the burn care measures devised by your medical team. Radiation burn care is in many cases the same as that for other types of burns. Depending on the extent and severity of the burn, you may need to be hospitalized. Treatments can range from wound care and pain management to skin grafting or other significant surgical procedures.[3]
- A person suffering from radiation burns typically does not pose a threat of radiation contamination. However, depending on the circumstances, quarantine measures may be utilized.
-
4Continue all recommended treatment measures at home. Once your medical team gets your burn care under control, they’ll advise you on the measures you need to take at home. Listen carefully, ask questions as needed, and follow their instructions to the letter. You might, for example:[4]
- Be prescribed oral pain medications.
- Be given antibiotics to reduce your risk of infection.
- Be instructed to clean and cover the burn in a specific fashion.
-
5Accept that you may experience long-term symptom recurrence. While cutaneous radiation injuries are similar in many ways to other types of skin burns, the symptoms are more likely to appear and reappear over a period of weeks, months, or even years. In each instance, you’ll need to follow the care routine recommended by your medical team.
- CRI symptoms often appear in fairly mild form within a few days of exposure, then disappear for several days or even a few weeks. They may then reappear in more or less severe forms on-and-off for weeks or months. In some cases, symptoms will appear for years after exposure.
Warning: Permanent changes in skin appearance, texture, and sensations are possible in some cases, as is an increased likelihood of developing skin cancer in the area.
Caring for Skin Damage from Radiation Therapy
-
1Discuss the risks and possible severity of skin reactions with your care team. Radiation therapy is a key element of treatment for many types of cancer. However, skin reactions in the treatment area occur in about 85% of patients, so it’s important to discuss this likelihood and how to respond to it with your cancer care team.[5]
- Skin reactions vary widely, ranging from mild irritation or redness to open wounds or ulcers. The location and intensity of your radiation treatments may impact how your skin responds.
- Skin damage may be one of the many challenges you’ll face during your cancer battle. Talk openly with your care team and your loved ones about your concerns, fears, and questions. Always remember that you’re not facing this fight alone.
Tip: The management of radiation dermatitis depends on the severity of your skin damage. For example, grade 1 radiation dermatitis may only require general skin care measures, grades 2-3 may require soft, absorbent bandages and antibiotics, and grade 4 may require surgical debridement.[6]
-
2Follow the care team’s advice on using moisturizers or topical creams. You may, for example, be advised to apply aloe vera or a particular moisturizing lotion to your treatment area one or more times each day. Or, you may be prescribed a topical corticosteroid or other medicated cream to apply to the area prior to treatment to help prevent severe radiation dermatitis and minimize discomfort and itching. In any case, follow the instructions provided by your care team.[7]
- There isn’t a great deal of strong evidence at present to support any one particular topical treatment over others. You may be advised to try different alternatives one at a time to determine which works best for you.
-
3Wash the treatment area gently with warm water and mild soap. Avoid harsh soaps, hot water, and vigorous scrubbing. Dampen your hand or a soft cloth to apply a gentle skin cleanser, rinse with tepid or cool water, and pat the area dry with another soft cloth. Wash the area once daily unless otherwise advised by your care team.[8]
- Keeping the area clean is important to reduce the risk of infection should you end up with broken skin or lesions. Just make sure to be gentle!
-
4Stop using antiperspirants, talc products, and other products noted by your team. Talcum powders and starch-based products should be avoided because they may increase the risk of infection. Meanwhile, products with metallic contents (such antiperspirants, which often include aluminum) can increase the dose of radiation absorbed by the skin.[9]
- Ask for advice on which brands of deodorants and other skin care products you can use. Your care team may be able to provide you with a list.
-
5Leave the treatment area unshaven to reduce the risk of skin irritation. This can be a challenge if you typically shave the treatment area, but shaving always causes at least a small amount of skin irritation. Your best bet is to simply let any hair in the treatment area grow until your care team says it’s OK to start shaving again.[10]
- An electric shaver or trimmer is less likely to cause irritation than a razor, but the best option is to avoid hair removal altogether.
-
6Use fragrance-free body products and laundry products. Fragrances and other additives may cause irritation, especially to the sensitive skin in the treatment area. Use laundry products marketed for sensitive skin and limit or avoid using fragrances like perfumes and scented lotions.[11]
-
7Wear loose, soft clothing over the treatment area. Tight or rough clothing will likely cause chafing and redness in the treatment area. Opt instead for soft fabrics, like cotton, and loose garments, like sweatpants instead of leggings.[12]
- Prioritize comfort over fashion while you’re undergoing radiation therapy!
- It’s important to avoid friction for 2-4 weeks following treatment, so make sure that you avoid any skin-on-skin contact. Wear clothing that is loose-fitting, but that also covers areas where there might be friction, such as in your underarm area.[13]
-
8Limit skin exposure to both sunlight and extreme temperatures. Hot weather, cold weather, and direct sunlight can all irritate your skin, especially when it’s already sensitive in the treatment area. Bundle up for or stay out of the cold, and stay indoors during the hottest parts of warm days. Use sun protection measures recommended by your care team, which may include:[14]
- Wearing an SPF 30 or higher broad spectrum sunscreen that is appropriate for your sensitive skin.
- Wearing long, loose clothing and a broad-brimmed hat.
- Staying indoors during the middle of the day, when the sun’s rays are most intense.
-
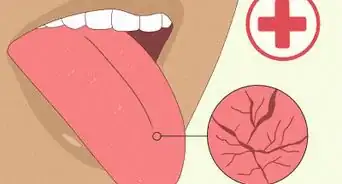
9Treat open wounds or sores in the treatment area as directed. Most likely, you’ll deal with redness and irritation in the treatment area. In some cases, though, you may develop open wounds, sores, or ulcers that require active treatment. Get instructions from your care team before attempting to treat any of these conditions.[15]
- You’ll get specific instructions for cleaning and covering any open wounds. Avoid using adhesive tapes or bandages right on the sensitive skin in the treatment area.
- You may be given topical or oral medications to reduce your risk of infection. Use these as directed.
References
- ↑ https://www.cdc.gov/nceh/radiation/emergencies/contamination.htm
- ↑ https://www.cdc.gov/nceh/radiation/emergencies/cri.htm
- ↑ https://www.cdc.gov/nceh/radiation/emergencies/criphysicianfactsheet.htm
- ↑ https://www.cdc.gov/nceh/radiation/emergencies/criphysicianfactsheet.htm
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2913836/
- ↑ https://dermnetnz.org/topics/radiation-dermatitis
- ↑ https://www.cdc.gov/nceh/radiation/emergencies/criphysicianfactsheet.htm
- ↑ https://www.cdc.gov/nceh/radiation/emergencies/selfdecon_wash.htm
- ↑ https://www.aad.org/public/diseases/skin-cancer/types/common/melanoma/radiation-care
- ↑ https://www.aad.org/diseases/skin-cancer/skin-care-after-radiation-therapy
- ↑ https://www.aad.org/diseases/skin-cancer/skin-care-after-radiation-therapy
- ↑ https://www.hopkinsmedicine.org/kimmel_cancer_center/patient_and_family_services/patient_information/education/side_effects/skin_care.html
- ↑ https://www.breastcancer.org/treatment/radiation-therapy/side-effects
- ↑ https://www.hopkinsmedicine.org/kimmel_cancer_center/patient_and_family_services/patient_information/education/side_effects/skin_care.html
- ↑ https://www.aad.org/diseases/skin-cancer/skin-care-after-radiation-therapy





































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...