This article was medically reviewed by Luba Lee, FNP-BC, MS. Luba Lee, FNP-BC is a Board-Certified Family Nurse Practitioner (FNP) and educator in Tennessee with over a decade of clinical experience. Luba has certifications in Pediatric Advanced Life Support (PALS), Emergency Medicine, Advanced Cardiac Life Support (ACLS), Team Building, and Critical Care Nursing. She received her Master of Science in Nursing (MSN) from the University of Tennessee in 2006.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 128,440 times.
If you have a skin fungal or ringworm infection, such as tinea corporis or tinea pedis, don’t worry. While they’re unsightly and often itchy, most fungal infections are usually straightforward to treat. The 2 primary forms of medical treatment are antifungal creams—which are applied directly to the infection—and oral drugs. It’s also important to have good skin hygiene when you’re treating a fungal infection. After consulting your doctor about your skin fungal infection, you may also opt to try a few natural remedies to accelerate the medical treatment.
Steps
Treating Infections with Medications
-
1Look for rashes, dry skin, and other symptoms of a fungal infection. Most types of fungal infections have symptoms that cause the infected skin to peel, dry out, and turn red. Most fungal infections are also itchy and can cause discomfort.[1] Some fungal rashes—like a vaginal yeast infection or vaginal candidiasis—may have little or no outward symptoms. In these kinds of cases, itching and discomfort are the primary symptoms.
- For example, ringworm on your face or body looks like 1⁄2 in (1.3 cm) circles on your skin. These circles are typically red, raised, and scaly, with raised edges. Ringworm on your feet, or athlete’s foot, manifests as itchy, peeling, dry white skin between your toes.
- Jock itch involves slightly larger red patches localized in the groin area, and is typically accompanied by severe itching.
-
2Apply an OTC antifungal cream for most skin fungal infections. Topical treatments are the most effective way to treat the majority of fungal infections. Antifungal creams should be applied directly to the infected skin, usually 2 or 3 times a day, and they’ll clear up an infection within a week. Always read the directions on the packaging closely and apply the topical cream as directed.[2]
- Visit your local pharmacy to purchase an OTC antifungal cream. Most large pharmacies have a specific “Antifungal” section.
- A few common OTC antifungal medications include Lamisil (which is safe for people over 12 years old), Desenex, and Lotrimin AF. Tinactin and Neosporin AF are good choices for treating children with fungal infections. Use these medications as directed on the packaging or by your doctor.
- Most varieties of OTC antifungal creams include drugs like miconazole, clotrimazole, and econazole.
Advertisement -
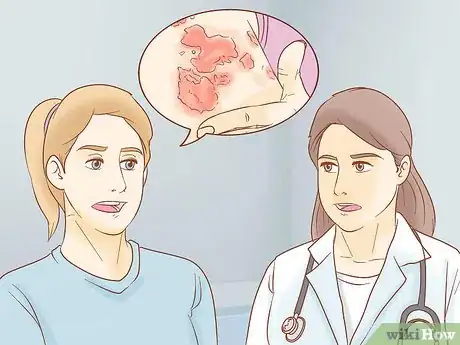
3See your doctor if the infection doesn’t clear up with topical cream. Most mild infections clear up relatively quickly with an antifungal cream. If your infection lasts more than 3 weeks—or if it grows to cover a larger area of your body—make an appointment with your general practitioner. Show them the infection and mention how long it’s lasted and whether it’s painful. Ask for a prescription to help clear up the infection.[3]
- Also schedule an appointment if you have a fungal infection on your scalp or a similarly hard-to-reach area.
-
4Agree to a laboratory diagnosis of the infected skin cells if necessary. In some cases, it’s tough to determine whether or not a rash has been caused by a fungal infection. In these instances, the doctor will collect a sample of skin from the afflicted area and send it to a medical lab for analysis. For example, the doctor will scrape skin cells off of your toes if they suspect you have athlete’s foot.[4]
- If you have a vaginal yeast infection, the doctor will take a sampling of skin cells from your vaginal walls and cervix.
-
5Take antifungal tablets for large infections or those above the jaw line. It would be impractical to apply a topical cream to, for example, your entire back or both of your legs. If you have a fungal rash that covers more than 1 square foot (0.093 m2) of your body, the best treatment option will be an oral tablet. You may also need oral medications to treat fungal infections on your face or scalp. Read the directions closely and take the oral tablets as directed.[5]
- In many cases, your doctor will ask you to continue taking oral meds for up to 2 weeks after the rash has cleared up.
- If you have a vaginal yeast infection, the doctor may prescribe soft medicated pellets that you can insert into your vagina that will clear up the infection.[6]
-
6Talk to your doctor about side effects from oral medications. Some people experience side effects from oral antifungal medications. In most cases, the side effects are relatively mild and are limited to issues like an upset stomach and irritated skin. Ask your doctor how to avoid or address these side effects.[7] For example, they may recommend Pepto-Bismol for your stomach and a medicated lotion for irritated skin.
- If you experience severe stomach pain after taking an oral antifungal medication, visit an Urgent Care or emergency room.
-
7Treat scalp infections with selenium sulfide shampoo. If you have a fungal infection of the scalp, look for a medicated shampoo containing selenium sulfide, such as Selsun Blue or Head & Shoulders. Follow the directions on the packaging or ask your doctor for advice on how to use these shampoos.[8]
- You can also use selenium sulfide shampoo to treat fungal rashes on other parts of your body, such as athlete’s foot. Apply the shampoo to the affected area in the shower and let it sit for a few minutes before rinsing it off. Your symptoms should resolve in about 4 weeks.
- If your symptoms get worse or don’t improve after a few weeks, follow up with your primary care doctor.
Taking Care of Your Skin
-
1Dry your skin thoroughly after your daily shower. If you have a fungal infection—or would like to prevent yourself from getting one—it’s best to shower once a day. After you get out of the shower, dry your skin thoroughly with a clean, dry towel. It’s especially important that you completely dry areas of skin that tend to sweat or that have folds. This includes areas like your armpits and groin.[9]
- Fungi love damp skin, so if your skin is still wet when you put your clothes on, you’ll risk contracting an infection.
- Keep your feet clean and dry and avoid sharing socks or shoes with other people.
-
2Wear loose-fitting fabric that wicks moisture away from your skin. Loose, baggy shirts made of cotton or linen are a great choice of clothing when you have a fungal infection on your skin. It’s important that your infected skin be able to dry out, and baggy clothes will facilitate this. Clothes that fit loosely will not rub and irritate the infected skin, allowing it to heal.
- Avoid wearing tight-fitting clothes and any clothing items made from fabrics that don’t breathe. Leather is a great example of a fabric to avoid.
-
3Wash your sheets, clothes, and towels weekly to remove lingering fungi. While you’re treating a skin fungal infection, it’s important to keep fabrics around you as clean as possible. Fungi can linger in any fabric material that comes into frequent contact with your body. Then, even if the infection clears up, you could re-contract the infection by, for example, sleeping on unwashed sheets.[10]
- This is also an important step in preventing the infection from spreading to other people. Fungi travel relatively easily, and you’ll risk infecting friends, roommates, and family members if you don’t keep your towels, sheets, and clothing clean.
- You can also protect your feet by wearing flip-flops in shared bathroom or shower areas, such as the showers at the gym or the area around the swimming pool.[11]
Trying Natural Remedies
-
1Rub coconut oil onto a fungal infection 2 times a day. Among its many other uses, coconut oil contains fatty acids that can kill some species of yeast and other fungal infections. Dab 2 fingers into a jar of coconut oil so that they’re covered with a thin layer of the oil. Then rub the fingers across the skin afflicted by a fungal infection until the area is fully covered.[12] Repeat this twice a day for best results.
- If you have a vaginal yeast infection, soak a tampon in warm coconut oil before inserting it.
- Coconut oil’s antifungal properties were proven in a study conducted by the U.S. National Library of Medicine.
-
2Apply crushed garlic under your nails to treat infected nail beds. It’s not uncommon for fungal infections to attack the skin just beneath your fingernails and toenails. To help treat infections in this hard-to-reach location, use the flat edge of a kitchen knife to crush up 1–2 cloves of garlic. Press the crushed garlic beneath the infected nails, and leave it there for 20–30 minutes before washing your hands or feet.[13]
- Medical studies have shown that garlic contains natural antibiotic properties which will help fight fungal infections.
-
3Drink diluted apple cider vinegar to combat fungal infections. Apple cider vinegar is full of healthy antimicrobials, which can fight off fungi and help clear up your infection. Mix apple cider vinegar and water at a 1:1 ratio and drink about 1 cup (240 mL) each day. This should help prevent your infection from spreading and will help clear up the infection quickly.[14]
- Apple cider vinegar is also full of healthy nutrients including phosphorus, potassium, and calcium. Its antifungal properties are largely anecdotal, however.
- You can purchase apple cider vinegar at any supermarket or grocery store. It may also be for sale at some large drugstores.
-
4Eat a plain yogurt with active cultures for breakfast. Yogurt with active bacteria cultures contains many probiotics, which can improve the health of the beneficial bacteria in your digestive tract. As a consequence of having a healthier gut, your body will be better able to fight off infections, including fungal infections.[15]
- You can purchase yogurt at any supermarket or grocery store. Check the yogurt’s label and make sure that it contains live Lactobacillus strains before you purchase it.
- Similarly to the apple cider vinegar, yogurt’s antifungal abilities are largely anecdotal, and come from yogurt’s ability to improve your overall gut health.
Expert Q&A
-
QuestionI have fungal infection below my breast. How can I treat this?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician You will need to see you PCP or a antifungal cream, preferably with a steroid to lessen the inflammation.
You will need to see you PCP or a antifungal cream, preferably with a steroid to lessen the inflammation.
Warnings
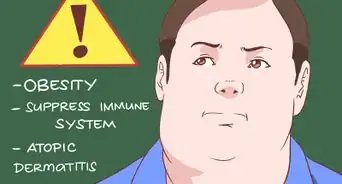
- Fungal infections of the skin can have very similar symptoms to other skin conditions, such as seborrheic dermatitis, psoriasis, atopic dermatitis, contact dermatitis, or even Lyme disease. If you have the symptoms of a fungal infection, it’s important to get an accurate diagnosis from your doctor so you can treat it appropriately.⧼thumbs_response⧽
- Fungal infections located under your fingernails or toenails are tough to treat. Even with medication, they can take up to a year to clear up.⧼thumbs_response⧽
- Don’t rely on natural remedies as a substitute for medical treatment. While natural remedies can supplement medicine, they should never be used in the place of seeing a doctor.⧼thumbs_response⧽
References
- ↑ https://childrensnational.org/choose-childrens/conditions-and-treatments/skin-disorders/fungal-infections
- ↑ https://www.bupa.co.uk/health-information/healthy-skin/fungal-skin-infections
- ↑ https://www.bupa.co.uk/health-information/healthy-skin/fungal-skin-infections
- ↑ https://www.medicalnewstoday.com/articles/317970.php
- ↑ https://www.bupa.co.uk/health-information/healthy-skin/fungal-skin-infections
- ↑ https://www.nhs.uk/conditions/antifungal-medicines/
- ↑ https://www.nhs.uk/conditions/antifungal-medicines/
- ↑ https://www.aad.org/public/diseases/a-z/seborrheic-dermatitis-self-care
- ↑ https://www.aafp.org/afp/2005/0901/p833.html
- ↑ https://www.aad.org/public/diseases/a-z/ringworm-self-care
- ↑ https://www.aad.org/public/diseases/a-z/ringworm-self-care
- ↑ https://www.health24.com/Medical/Skin/Fungal-skin/5-home-remedies-for-fungal-infections-20180322-2
- ↑ https://www.health24.com/Medical/Skin/Fungal-skin/5-home-remedies-for-fungal-infections-20180322-2
- ↑ https://www.health24.com/Medical/Skin/Fungal-skin/5-home-remedies-for-fungal-infections-20180322-2
- ↑ https://www.health24.com/Medical/Skin/Fungal-skin/5-home-remedies-for-fungal-infections-20180322-2









































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...