This article was co-authored by Timothy Sherman, RN. Timothy Sherman is a Registered Nurse (RN) based in Austin, Texas and affiliated with St. David's HealthCare. With over seven years of nursing experience, Timothy specializes in working with adults in a general medical/surgical setting, chemotherapy, and with biotherapy administration. He has also instructed Essentials of Medical Terminology and Anatomy and Physiology for Medical Assistants at Austin Community College. He received his BS in Nursing from Wichita State University in 2012.
There are 8 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 41,558 times.
Valley fever is a fungal infection that is caught in desert climates, like southwestern United States and northwestern Mexico. The fungus is found in the soil. Valley fever is difficult to diagnose because it has nonspecific symptoms. Mild cases of valley fever may need no treatment, and most infections can be treated with antifungal medication. Learn how to treat valley fever so you can get the treatment you need.
Steps
Seeking Medical Treatment
-
1See a specialist. If you have been diagnosed with valley fever, your doctor may refer you to a specialist who deals specifically with valley fever. Your doctor may do this if you have a severe case of valley fever or if you have had valley fever before and relapsed.[1]
-
2Take antifungal medication. There are no over-the-counter medications you can buy to treat valley fever. You should see your doctor if you are experiencing severe symptoms or have relapsed. Antifungal medication is prescribed to treat valley fever, and the treatment usually is given for three to six months, depending on the severity of your complications.[2]
- You may be given ketoconazole, itraconazole, or fluconazole. Another option for a severe case of valley fever is amphotericin B, which is given intravenously.
- If you develop certain other conditions due to the valley fever, such as meningitis, you may have to take antifungal medication for the rest of your life.
Advertisement -
3Treat associated conditions. Valley fever sometimes can lead to more serious conditions, especially if you have a weakened immune system. Valley fever may turn into a severe lung infection, such as pneumonia, or infections that spread to the rest of the body.[3]
- If this is the case, the doctor may put you in the hospital to treat the valley fever with antifungals while treating the other condition.
- For individuals experiencing more serious complications treatment may extend longer than six months.
-
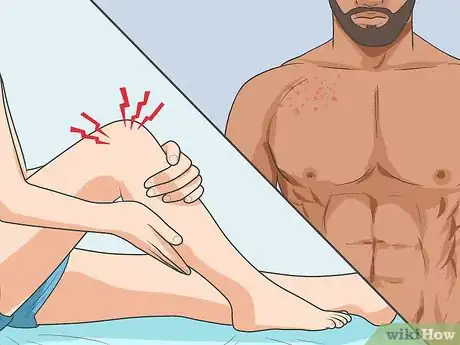
4Undergo surgery. In severe cases of valley fever, you may have to go into the hospital to get surgery to deal with the effects of valley fever. For example, if you have severe lung damage due to valley fever, you may have to have cavities in the lung surgically removed.[4]
- If the arthritis and joint inflammation associated with valley fever is severe, you may have to have the fluid or abscesses in the bones or joints drained surgically.
- Bone may need to be surgically removed if osteomyelitis has occurred.[5]
Using Natural Remedies to Treat Valley Fever
-
1Treat the flu-like symptoms. A common way to treat valley fever is to treat the flu-like symptoms. The main treatment is to get plenty of rest. Many cases of valley fever are mild. It may present like a minor cold or mild flu, so taking it easy and resting may be all you need. Make sure to drink plenty of fluids. Valley fever often goes away on its own.[6]
- Rest helps your body fight off the infection. You can stay at home to allow your body time to recover.
- Valley fever is not contagious, so you don’t have to worry about spreading it to others at work or school.
-
2Eat an antifungal diet. A diet that helps create an environment where fungi won’t grow may help kill the valley fever fungus. You should significantly reduce your intake of dairy, sugars, beer, and foods that contain yeast. These foods encourage fungus to grow and thrive inside the body.
- Try not to eat milk, cheese, or yogurt while you are trying to treat valley fever. Eliminate sugars, including those coming from honey, fruit, or fruit juice.
- Restrict intake of beer and other foods or drinks containing yeast.
- Focus on eating foods that are unprocessed or uncooked during the treatment period.
-
3Take supplements. Another way you may be able to naturally kill the fungus is through supplements. You can try taking vitamin C, E, B complex, and A-plus to help promote an environment inside your body where fungi won’t thrive. Turmeric is a common antifungal that can be taken to help kill the fungus. Garlic is an antifungal herb that can be eaten or taken as a supplement that may help kill the fungus.
- Lactobacillus acidophilus and Bifidobacterium supplements may help restore a health normal flora within the gut.
- You may also want to try aloe vera, basil, cinnamon, cloves, magnesium, manganese, oregano, thyme, wheat germ, or zinc. They all have antifungal properties that may help.
-
4Use caution with natural remedies. Always use caution when using natural remedies to treat valley fever. You should talk to your doctor or a naturopathy doctor before choosing to use a natural remedy over a medical one. Valley fever is usually mild and may respond well to natural treatments, but certain people are at a higher risk for severe symptoms or cases of valley fever.
- If you have a severe case of valley fever or have a compromised immune system, always see your doctor.
Diagnosing Valley Fever
-
1Identify the symptoms. If you have valley fever, you may develop flu-like symptoms. Common symptoms include a fever, chills, shortness of breath, and night sweats. You may have a dry cough or a cough that produces blood. You might develop headaches and feel fatigued.[7]
- Your joints or bones may start to ache, like you have arthritis.
- A rash may also appear with valley fever. The rash includes red painful bumps on the lower part of your legs. The rash may also appear on the chest, arms, or back. The bumps might turn from red to a brown color. Bumps may also have heads like pimples or form blisters.
- Many times, valley fever presents no symptoms.
-
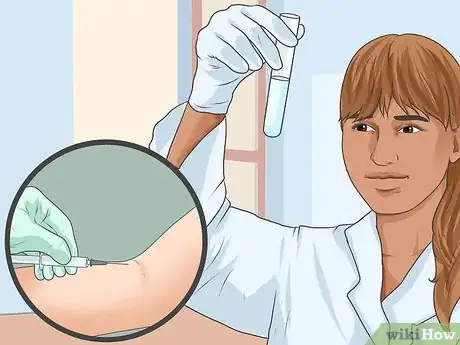
2Get a diagnosis. To get a diagnosis, you should visit your doctor. The symptoms are nonspecific, which means it’s difficult to figure out that you valley fever just from the symptoms. The doctor will run various tests to positively identify the presence of the valley fever fungus in your body.[8]
- The doctor will either do a smear culture or a blood test. These will show that the valley fever fungus is in your body.
-
3Identify where valley fever most often occurs. Valley fever can be contracted in arid desert locations in North and South America. This includes the southwestern United States and northwestern Mexico. People who live in these areas are at risk of contracting the fungus. People who visit may also get it, too.[9]
- Jobs that disturb the earth or have a person digging in the soil exponentially increase the risk of contracting the disease.
- Recreational activities where you disturb the soil or inhale dust from the soil, such as biking or riding ATVs, may increase your risk.
-
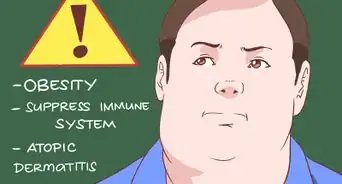
4Recognize those at high risk for a severe case of valley fever. Valley fever is pretty mild in most cases. However, some people have a higher risk of the fungus turning into a worse condition or even becoming deadly. Those who are at a higher risk include those with weakened immune systems or who are already ill.[10]
- This includes those who are HIV positive, pregnant women, diabetics, and people who take medications that make the immune system weaker.
- Certain ethnicities are at a higher risk: Filipinos, African Americans, Mexican Americans, and Native Americans.
Expert Q&A
-
QuestionHow long does this Valley Fever last if untreated?
 Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Janice Litza, MDDr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
Board Certified Family Medicine Physician Depending on overall health it can last weeks to months as a mild cold, or develop into complications as mentioned above.
Depending on overall health it can last weeks to months as a mild cold, or develop into complications as mentioned above.
References
- ↑ http://www.cdc.gov/fungal/diseases/coccidioidomycosis/treatment.html
- ↑ http://www.cdc.gov/fungal/diseases/coccidioidomycosis/treatment.html
- ↑ https://www.canada.ca/en/public-health/services/diseases/valley-fever-coccidioidomycosis/risks-valley-fever-coccidioidomycosis.html
- ↑ https://vfce.arizona.edu/valley-fever-people/faqs
- ↑ https://www.cedars-sinai.edu/Patients/Health-Conditions/Valley-Fever-or-San-Joaquin-Fever-Coccidiodomycosis.aspx
- ↑ https://health.ucdavis.edu/valley-fever/about-valley-fever/clinical-manifestations/index.html
- ↑ https://www.canada.ca/en/public-health/services/diseases/valley-fever-coccidioidomycosis/symptoms-valley-fever-coccidioidomycosis.html
- ↑ https://health.ucdavis.edu/valley-fever/about-valley-fever/clinical-use-diagnostic-testing/index.html
- ↑ https://vfce.arizona.edu/valley-fever-people/faqs



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...