This article was co-authored by Mental Health America and by wikiHow staff writer, Jennifer Mueller, JD. Mental Health America is the nation's leading community-based nonprofit dedicated to addressing the needs of those living with mental illness and promoting overall mental health for all. Their work is guided by the Before Stage 4 philosophy – that mental health conditions should be treated long before they reach the most critical points in the disease process.
There are 28 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 2,384 times.
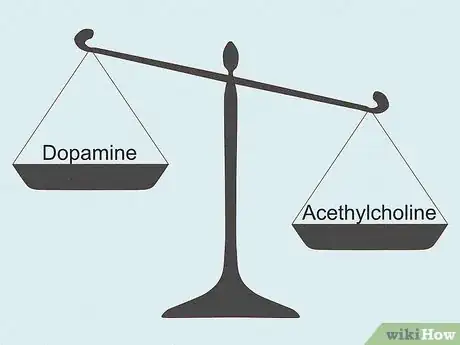
Acetylcholine might not get talked about as much as neurotransmitters like dopamine and serotonin, but it actually plays an exciting role in your body—quite literally. Acetylcholine's primary role is excitatory, meaning it causes action. It was also the first neurotransmitter ever discovered, and the one scientists know the most about.[1] Here, you'll learn all you need to know about the fascinating role this neurotransmitter plays in your body, as well as what scientists are learning about how it affects your brain functioning and mental health.
Steps
Expert Q&A
-
QuestionHow does acetylcholine play a role in mental illness?
 Kirsten Thompson, MDDr. Kirsten Thompson is a Board Certified Psychiatrist, Clinical Instructor at UCLA, and the Founder of Remedy Psychiatry. She specializes in helping patients with mental health conditions such as major depressive disorder, anxiety, ADHD, bipolar disorder, OCD, PTSD, and postpartum depression. Dr. Thompson holds a BS in Operations Research Industrial Engineering from Cornell University and an MD from The State University of New York, Downstate College of Medicine.
Kirsten Thompson, MDDr. Kirsten Thompson is a Board Certified Psychiatrist, Clinical Instructor at UCLA, and the Founder of Remedy Psychiatry. She specializes in helping patients with mental health conditions such as major depressive disorder, anxiety, ADHD, bipolar disorder, OCD, PTSD, and postpartum depression. Dr. Thompson holds a BS in Operations Research Industrial Engineering from Cornell University and an MD from The State University of New York, Downstate College of Medicine.
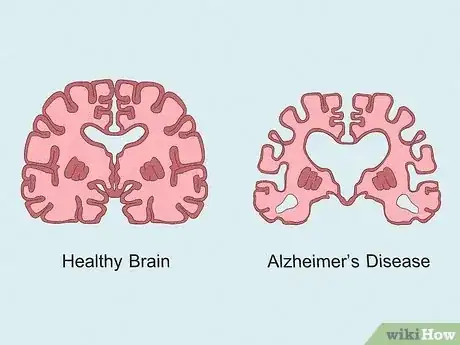
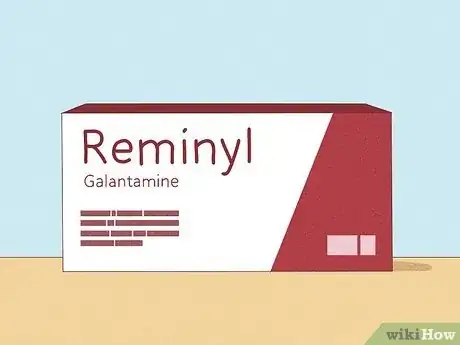
Board Certified Psychiatrist Too much or too little acetylcholine can lead to neurological issues since it affections emotions, memory, and cognition. Too little acetylcholine can result in conditions like Alzheimer's disease and Parkinson's disease; on the other hand, too much acetylcholine can be linked to symptoms of anxiety and depression.
Too much or too little acetylcholine can lead to neurological issues since it affections emotions, memory, and cognition. Too little acetylcholine can result in conditions like Alzheimer's disease and Parkinson's disease; on the other hand, too much acetylcholine can be linked to symptoms of anxiety and depression. -
QuestionWhat are the most common treatments for ADHD?
 George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
Licensed Psychologist Common treatment options for adults with ADHD include medication as well as coaching or therapy. Coaching or therapy focus not only on the executive functioning issues like organizing, planning, and decision-making, but they also focus on impulsivity and any of the emotional factors that come with ADHD like depression, anxiety or shame.
Common treatment options for adults with ADHD include medication as well as coaching or therapy. Coaching or therapy focus not only on the executive functioning issues like organizing, planning, and decision-making, but they also focus on impulsivity and any of the emotional factors that come with ADHD like depression, anxiety or shame. -
QuestionDoes CBT work for ADHD?
 George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
George Sachs, PsyDGeorge Sachs is a Licensed Psychologist and the Owner of Sachs Center based in New York, New York. With over ten years of experience, Dr. Sachs specializes in treating ADD/ADHD and Autism Spectrum Disorders in children, teens, and adults. He holds a BS in Psychology from Emory University. Dr. Sachs earned his Doctorate of Psychology (PsyD) from the Illinois School of Professional Psychology, Chicago. He completed his clinical training in Chicago at Cook County Hospital, Mt. Sinai Hospital, and the Child Study Center. Dr. Sachs completed his internship and postdoctoral work at the Children’s Institute in Los Angeles, where he supervised and trained therapists in Trauma-Focused Cognitive Behavioral Therapy (TFCBT). He has been trained as a Gestalt Therapist and certified by the Gestalt Associates Training Program of Los Angeles. Dr. Sachs is the author of The Adult ADD Solution, Helping the Traumatized Child, and Helping Your Husband with Adult ADD. He has appeared on the Huffington Post, NBC Nightly News, CBS, and WPIX discussing his holistic approach to ADD/ADHD treatment.
Licensed Psychologist Absolutely! Cognitive Behavioral Therapy works really well for adults that are diagnosed with ADHD.
Absolutely! Cognitive Behavioral Therapy works really well for adults that are diagnosed with ADHD.
References
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7226243/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK557825/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK11143/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK11143/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK557825/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK557825/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127047/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2659740/
- ↑ https://www.frontiersin.org/articles/10.3389/fnbeh.2012.00024/full
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3642390/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4487649/
- ↑ https://www.nature.com/articles/npp2013274
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK557825/
- ↑ https://www.nature.com/articles/s41401-020-0380-z
- ↑ https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Myasthenia-Gravis-Fact-Sheet
- ↑ https://www.mda.org/disease/lambert-eaton-myasthenic-syndrome
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127047/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127047/
- ↑ https://www.health.harvard.edu/blog/common-anticholinergic-drugs-like-benadryl-linked-increased-dementia-risk-201501287667
- ↑ https://www.health.harvard.edu/blog/common-anticholinergic-drugs-like-benadryl-linked-increased-dementia-risk-201501287667
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK557791/
- ↑ https://psychnews.psychiatryonline.org/doi/10.1176/pn.38.22.0025
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK555893/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK11143/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3648782/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK534798/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK534798/
- ↑ https://www.rch.org.au/clinicalguide/guideline_index/Anticholinergic_Syndrome/
- ↑ https://www.rch.org.au/clinicalguide/guideline_index/Anticholinergic_Syndrome/
- ↑ https://www.rch.org.au/clinicalguide/guideline_index/Anticholinergic_Syndrome/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK534798/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK534798/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK534798/
- ↑ https://pubmed.ncbi.nlm.nih.gov/7752065/
- ↑ https://ods.od.nih.gov/factsheets/Choline-HealthProfessional/
- ↑ https://uncnri.org/2017/06/01/know-your-neurotransmitters-acetylcholine/
- ↑ https://uncnri.org/2017/06/01/know-your-neurotransmitters-acetylcholine/
- ↑ https://www.nccih.nih.gov/health/using-dietary-supplements-wisely
- ↑ https://pubmed.ncbi.nlm.nih.gov/11090296/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4137276/
- ↑ https://pubmed.ncbi.nlm.nih.gov/23772955/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3659552/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK482433/
- ↑ https://www.ncbi.nlm.nih.gov/books/NBK11143/