This article was co-authored by Trudi Griffin, LPC, MS. Trudi Griffin is a Licensed Professional Counselor in Wisconsin specializing in Addictions and Mental Health. She provides therapy to people who struggle with addictions, mental health, and trauma in community health settings and private practice. She received her MS in Clinical Mental Health Counseling from Marquette University in 2011.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 17 testimonials and 94% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 305,276 times.
A mental health treatment plan is a document that details a client's current mental health problems and outlines the goals and strategies that will assist the client in overcoming mental health issues. To obtain the information needed to complete a treatment plan, a mental health worker must interview the client. The information gathered during the interview is used to write the treatment plan.
Steps
Conducting a Mental Health Assessment
-
1Gather information. A psychological evaluation is a fact-gathering session in which a mental health worker (counselor, therapist, social worker, psychologist or psychiatrist) interviews a client about current psychological problems, past mental health issues, family history and current and past social problems with work, school and relationships. A psychosocial evaluation can also examine past and current substance abuse problems as well as any psychiatric drugs the client has used or is currently on.
- The mental health worker may also consult a client's medical and mental health records during the evaluation process. Make sure appropriate releases of information (ROI documents) have been signed.
- Make sure you also appropriately explain the limits to confidentiality. Tell the client that what you talk about is confidential, but the exceptions are if the client intends to harm himself, someone else, or is aware of abuse occurring in the community.[1]
- Be prepared to halt the evaluation if it becomes apparent the client is in crisis. For example, if the client has suicidal or homicidal ideations, you will need to switch gears and follow crisis intervention procedures immediately.[2]
-
2Follow the sections of the evaluation. Most mental health facilities provide the mental health worker with an evaluation template or form to complete during the interview.[3] An example of sections for a mental health assessment include (in order):[4] [5]
-
Reason for referral
- Why is the client coming in to treatment?
- How was he referred?
-
Current symptoms and behaviors
- Depressed mood, anxiety, change in appetite, sleep disturbance, etc.
-
History of the problem
- When did the problem begin?
- What is the intensity/frequency/duration of the problem?
- What, if any, attempts have been made to solve the problem?
-
Impairments in life functioning
- Issues with home, school, work, relationships
-
Psychological/psychiatric history
- Such as previous treatment, hospitalizations, etc.
-
Current risk and safety concerns
- Thoughts of harming self or others.
- If the patient raises these concerns, stop the assessment and follow crisis intervention procedures.
-
Current and previous medication, psychiatric or medical
- Include the name of the medication, the dosage level, the length of time the client has been taking the medication and whether he is using it as prescribed.
-
Current substance use and substance use history
- Abuse or use of alcohol and other drugs.
-
Family background
- Socioeconomic level
- Parent's occupations
- Parent's marital status (married/separated/divorced)
- Cultural background
- Emotional/medical history
- Family relationships
-
Personal history
- Infancy – developmental milestones, amount of contact with parents, toilet training, early medical history
- Early and middle childhood — adjustment to school, academic achievement, peer relationships, hobbies/activities/interests
- Adolescence — early dating, reaction to puberty, presence of acting out
- Early and middle adulthood — career/occupation, satisfaction with life goals, interpersonal relationships, marriage, economic stability, medical/emotional history, relationship with parents
- Late adulthood —medical history, reaction to declining abilities, economic stability
-
Mental status
- Grooming and hygiene, speech, mood, affect, etc.
-
Miscellaneous
- Self-concept (like/dislike), happiest/saddest memory, fears, earliest memory, noteworthy/reoccurring dreams
-
Summary and clinical impression
- A short summary of the client's problems and symptoms should be written in narrative form. In this section, the counselor can include observations about how the patient looked and acted during the evaluation.
-
Diagnosis
- Use the information collected to form a (DSM-V or descriptive) diagnosis.
-
Recommendations
- Therapy, referral to psychiatrist, drug treatment, etc. This should be guided by the diagnosis and clinical impression. An effective treatment plan will lead to discharge.
Advertisement -
Reason for referral
-
3Note behavioral observations. The counselor will conduct a mini-mental-status exam (MMSE) which involves observing the client's physical appearance and his or her interactions with the staff and other clients at the facility. The therapist will also make a decision about the client's mood (sad, angry, indifferent) and affect (the client's emotional presentation, which can range from expansive, showing a great deal of emotion, to flat, showing no emotion). These observations assist the counselor in making a diagnosis and writing an appropriate treatment plan. Examples of subjects to cover on the mental status exam include:[6]
- Grooming and hygiene (clean or disheveled)
- Eye contact (avoidant, little, none, or normal)
- Motor activity (calm, restless, rigid, or agitated)
- Speech (soft, loud, pressured, slurred)
- Interactional style (dramatic, sensitive, cooperative, silly)
- Orientation (does the person know the time, date, and situation he is in)
- Intellectual functioning (unimpaired, impaired)
- Memory (unimpaired, impaired)
- Mood (euthymic, irritable, tearful, anxious, depressed)
- Affect (appropriate, labile, blunted, flat)
- Perceptual disturbances (hallucinations)
- Thought process disturbances (concentration, judgment, insight)
- Thought content disturbances (delusions, obsessions, suicidal thoughts)
- Behavioral disturbances (aggression, impulse control, demanding)
-
4Make a diagnosis. The diagnosis is the main problem. Sometimes a client will have multiple diagnoses such as both Major Depressive Disorder and Alcohol Use. All diagnoses must be made before a treatment plan can be completed.[7]
- A diagnosis is chosen based on the client's symptoms and how they fit with the criteria outlined in the DSM. The DSM is the diagnostic classification system created by the American Psychiatric Association (APA). Use the most recent version of the Diagnostic and Statistical Manual (DSM-5) to locate the correct diagnosis.
- If you don’t own a DSM-5, borrow one from a supervisor or colleague. Do not rely on online resources for a correct diagnosis.
- Use the main symptoms the client is experiencing in order to come to a diagnosis.
- If you are unsure about the diagnosis or you need expert assistance, speak to your clinical supervisor or consult with an experienced clinician.
Developing Goals
-
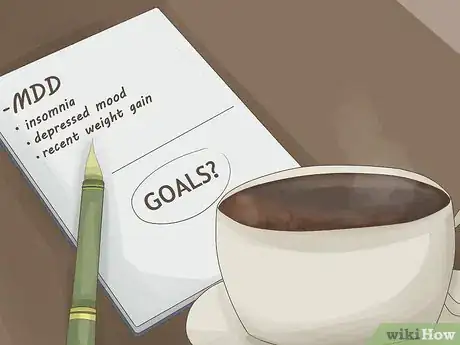
1Identify possible goals. Once you have completed the initial assessment and made a diagnosis, you will want to think about what interventions and goals you might want to create for treatment. Typically, clients will need some help identifying goals so it helps if you are prepared before having the discussion with your client.
- For example, if your client has Major Depressive Disorder, a likely goal will be to reduce the symptoms of MDD.
- Think about possible goals for the symptoms the client is experiencing. Perhaps your client has insomnia, depressed mood, and recent weight gain (all possible symptoms of MDD). You could create a separate goal for each of these prominent issues.
-
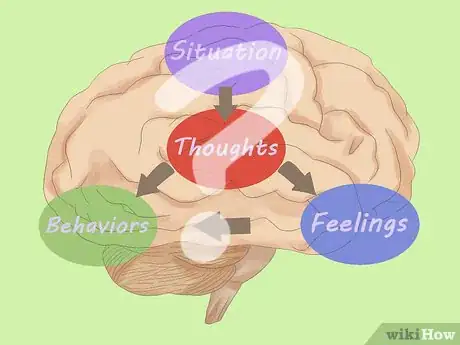
2Think of interventions. The interventions are the meat of change in therapy. Your therapeutic interventions are what will ultimately evoke change in your client.
- Identify types of treatment, or interventions, you might use such as: activity scheduling, cognitive-behavioral therapy and cognitive restructuring, behavioral experiments, assigning homework, and teaching coping skills such as relaxation techniques, mindfulness and grounding.
- Make sure you stick to what you know. Part of being an ethical therapist is about doing what you are competent in so that you do not cause harm to the client. Don’t try to attempt a therapy you are not trained in unless you have plenty of clinical supervision with an expert.
- If you are a beginner, try using a model or workbook in the type of therapy you choose. This can help keep you on track.
-
3Discuss goals with the client. After the initial assessment is conducted, the therapist and client will collaborate to create appropriate goals for treatment. This discussion needs to occur before the treatment plan is made.
- A treatment plan should include direct input from the client. The counselor and client decide, together, what goals should be included in the treatment plan and the strategies that will be used to reach them.
- Ask the client what he would like to work on in treatment. He may say something like, “I want to feel less depressed.” Then, you can offer suggestions on what goals might be helpful to reduce his symptoms of depression (such as engaging in CBT).
- Try using a form found online for creating goals.[8]
You can ask your client these questions:
- What is one goal you have for therapy? What would you like to be different?
- What steps can you take to make this happen? Offer suggestions and ideas if the client gets stuck.
- On a scale of zero to ten with zero being totally not achieved and ten being totally achieved, how far along the scale are you with regard to this goal? This helps make the goals measurable.
-
4Make concrete goals for treatment. Goals for treatment are what drive the therapy. The goals are also what make up a large component of the treatment plan. Try using a SMART goals approach:
- Specific – Be as clear as possible, such as reducing severity of depression, or reducing nights with insomnia.
- Measurable – How will you know when you have achieved your goal? Make sure it’s quantifiable, such as reducing depression from 9/10 severity to 6/10. Another option would be to reduce insomnia from three nights per week to one night per week.
- Achievable – Make sure the goals are attainable and not too high. For example, reducing insomnia from seven nights per week to zero nights per week, might be a difficult goal to achieve in a short period of time. Consider changing it to four nights per week. Then, once you achieve four you can create a new goal of zero.
- Realistic and Resourced - Is this achievable with the resources you have? Are there any other resources you need before you can, or to help you, achieve your goal? How can you access these resources?
- Time-limited – Set a time limit for each goal such as three months or six months.[9]
- A fully formed goal might look like: Client will reduce insomnia from three nights per week to one night per week in the next three months.
Creating the Treatment Plan
-
1Record the treatment plan's components. The treatment plan will consist of the goals that the counselor and therapist has decided on. Many facilities have a treatment plan template or form that the counselor will fill out. Part of the form may require that the counselor check boxes that describe the client's symptoms. A basic treatment plan will have the following information:[10]
- Name of client and diagnosis.
- Long term goal (such as client stating, “I want to heal my depression.”)
- Short terms goals or objectives (Client will reduce depression severity from 8/10 to 5/10 within six months). A good treatment plan will have at least three goals.
- Clinical interventions/Type of services (individual, group therapy, Cognitive-behavioral therapy, etc)
- Client involvement (what the client agrees to do such as attend therapy once per week, complete therapy homework assignments, and practice coping skills learned in treatment)
- Dates and signatures of therapist and client
-
2Record the goals. Your goals need to be as clear and concise as possible. Remember the SMART goals plan and make each goal specific, measurable, achievable, realistic, and time-limited.
- The form may have you record each goal separately, along with the interventions you will use toward that goal, and then what the client agrees to do.[11]
-
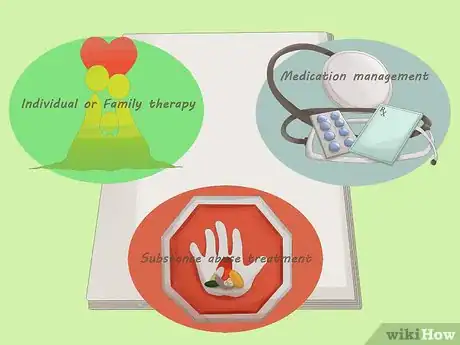
3Express specific interventions you will use. The counselor will include treatment strategies the client has agreed to. The form of therapy that will be used to accomplish these goals can be indicated here, such as individual or family therapy, substance abuse treatment and medication management.
-
4Sign the treatment plan. Both the client and the counselor sign the treatment plan to show that there is an agreement on what to focus on in treatment.
- Make sure this is done as soon as you have completed the treatment plan. You want the dates on the form to be accurate and you want to show that your client agrees with the treatment plan goals.
- If you do not get the treatment plan signed, insurance companies may not pay for services rendered.
-
5Review and improve as needed. You will be expected to complete goals and make new ones as the client progresses in treatment. The treatment plan should include dates in the future that the client and counselor will review the progress the client is making. Decisions to continue the current treatment plan or to make changes will be made at that time.
- You may want to check in with the client’s goals on a weekly or monthly basis in order to identify progress. Ask questions such as, “How many times did you experience insomnia this week?” Once your client has met his goal, say of experiencing insomnia only once per week, you can move on to another goal (perhaps getting it to zero times per week, or improving sleep quality overall).
Things You'll Need
- Evaluation template or form
- Medical and mental health records
- Treatment plan template or form
References
- ↑ http://www.counseling.org/resources/library/vistas/vistas12/Article_10.pdf
- ↑ http://www.counseling.org/resources/library/vistas/vistas12/Article_10.pdf
- ↑ http://file.lacounty.gov/dmh/cms1_159895.pdf
- ↑ http://file.lacounty.gov/dmh/cms1_159895.pdf
- ↑ https://books.google.com/books?id=ajwZjaBxmxQC&printsec=frontcover&source=gbs_ge_summary_r&cad=0#v=onepage&q&f=false
- ↑ http://file.lacounty.gov/dmh/cms1_159895.pdf
- ↑ http://www.counseling.org/resources/library/vistas/vistas12/Article_10.pdf
- ↑ http://www.getselfhelp.co.uk/docs/TherapyGoals.pdf
- ↑ http://www.getselfhelp.co.uk/docs/SMARTgoals.pdf
About This Article
When writing a mental health treatment plan, you should identify a client’s major symptoms and set goals for treating them. Start by listing your client’s specific symptoms, like insomnia, depressed mood, and weight gain. Then, work with your client to come up with possible treatments for their major symptoms. For example, for social anxiety, you might prescribe Cognitive Behavioral Therapy. To help you prioritize treatment of their symptoms, ask the client questions like, “What is one goal you have for therapy? What would you like to change?” For each method of treatment, set an actionable goal by using the Smart method. Each goal should be Specific, Measurable, Achievable, Realistic and resourced, and Time-Limited. For more tips from our Counseling co-author, including how to layout your mental health treatment plan on the page, read on!



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...