Childhood obesity
Childhood obesity is a condition where excess body fat negatively affects a child's health or well-being. As methods to determine body fat directly are difficult, the diagnosis of obesity is often based on BMI. Due to the rising prevalence of obesity in children and its many adverse health effects it is being recognized as a serious public health concern.[1] The term 'overweight' rather than 'obese' is often used when discussing childhood obesity, as it is less stigmatizing, although the term 'overweight' can also refer to a different BMI category.[2] The prevalence of childhood obesity is known to differ by sex and gender.[3]
| Childhood obesity | |
|---|---|
 | |
| Children with varying degrees of body fat | |
| Specialty | Endocrinology, pediatrics, bariatrics |
| Part of a series on |
| Human body weight |
|---|
Classification
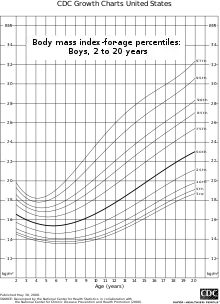 BMI for age percentiles for boys 2 to 20 years of age. |
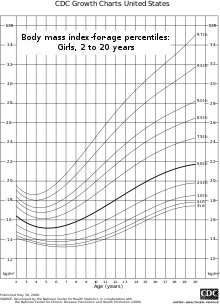 BMI for age percentiles for girls 2 to 20 years of age. |
Body mass index (BMI) is acceptable for determining obesity for children two years of age and older.[4] It is determined by the ratio of weight to height.[5]
The normal range for BMI in children vary with age and sex. While a BMI above the 85th percentile is defined as overweight, a BMI greater than or equal to the 95th percentile is defined as obesity by Centers for Disease Control and Prevention. It has published tables for determining this in children.[6]
The US Preventive Service Task Force reported that not all children with a high BMI need to lose weight though. High BMI can identify a possible weight problem, but does not differentiate between fat or lean tissue.[7] Additionally, BMI may mistakenly rule out some children who do have excess adipose tissue. It is therefore beneficial to supplement the reliability of a BMI diagnosis with additional screening tools such as adipose tissue or skin fold measurements.[8]
Effects on health
Psychological
The first problems to occur in obese children are usually emotional or psychological.[9] Obese children often experience bullying by their peers.[10][11] Some are harassed or discriminated against by their own family.[11] Stereotypes abound and may lead to low self-esteem and depression.[12]
Physical
Childhood obesity however can also lead to life-threatening conditions including diabetes, high blood pressure, heart disease, sleep problems, cancer, and other disorders.[13][14] Some of the other disorders would include liver disease, early puberty or menarche, eating disorders such as anorexia and bulimia, skin infections, and asthma and other respiratory problems.[15]
The early physical effects of obesity in adolescence include, almost all of the child's organs being affected, gallstones, hepatitis, sleep apnoea and increased intracranial pressure.[16] Overweight children are also more likely to grow up to be overweight adults.[14] Obesity during adolescence has been found to increase mortality rates during adulthood.[17]
A 2008 study has found that children who are obese have carotid arteries which have prematurely aged by as much as thirty years as well as abnormal levels of cholesterol.[18]
|
System |
Condition |
System |
Condition |
|---|---|---|---|
| Endocrine |
|
Cardiovascular |
|
| Gastroentestinal | Respiratory | ||
| Musculoskeletal |
|
Neurological | |
| Psychosocial |
|
Skin |
Long-term effects
Children who are obese are likely to be obese as adults. Thus, they are more at risk for adult health problems such as heart disease, type 2 diabetes, stroke, several types of cancer, and osteoarthritis. One study showed that children who became obese as early as age 2 were more likely to be obese as adults.[22] According to an article in The New York Times all of these health effects are contributing to a shorter lifespan of five years for these obese children. It is the first time in two centuries that the current generation of children in America may have a shorter lifespan than their parents.[23]
Causes
Childhood obesity can be brought on by a range of factors which often act in combination.[24][25][26][27][28] "Obesogenic environment" is the medical term set aside for this mixture of elements.[29] The greatest risk factor for child obesity is the obesity of both parents. This may be reflected by the family's environment and genetics.[30] Other reasons may also be due to psychological factors and the child's body type.
A 2010 review stated that childhood obesity likely is the result of the interaction of natural selection favouring those with more parsimonious energy metabolism and today's consumerist society with easy access to energy dense cheap foods and less energy requirements in daily life.[31]
Factors include the increase in use of technology, increase in snacks and portion size of meals, and the decrease in the physical activity of children. A study found kids that use electronic devices 3 or more hours a day had between a 17- 44% increased risk of being overweight, or a 10- 61% increased risk of obese (Cespedes 2011).
Childhood obesity is common among children from, low-income, African American and Hispanic communities. This is mainly because minority children spend less time playing outside the house and staying active. Some contributors to childhood obesity is that parents would rather have their children stay inside the home because they fear that gang, drug violence, and other dangers might harm them.[32]
Genetics
Childhood obesity is often the result of an interplay between many genetic and environmental factors. Polymorphisms in various genes controlling appetite and metabolism predispose individuals to obesity when sufficient calories are present. Over 200 genes affect weight by determining activity level, food preferences, body type, and metabolism.[33] Having two copies of the allele called FTO increases the likelihood of both obesity and diabetes.[34]
As such, obesity is a major feature of a number of rare genetic conditions that often present in childhood:
- Prader–Willi syndrome with an incidence between 1 in 12,000 and 1 in 15,000 live births is characterized by hyperphagia and food preoccupations which leads to rapid weight gain in those affected.
- Bardet–Biedl syndrome
- MOMO syndrome
- Leptin receptor mutations
- Congenital leptin deficiency
- Melanocortin receptor mutations
In children with early-onset severe obesity (defined by an onset before ten years of age and body mass index over three standard deviations above normal), 7% harbor a single locus mutation.[35][36]
One study found that 80% of the offspring of two obese parents were obese in contrast to less than 10% of the offspring of two parents who were of normal weight.[1][37] The percentage of obesity that can be attributed to genetics varies from 6% to 85% depending on the population examined.[38]
Family practices
In the recent decades, family practices have significantly changed, and several of these practices greatly contribute to childhood obesity:[5]
- With a decreasing number of mothers who breast-feed, more infants become obese children as they grow up and are reared on infant formula instead.[39]
- Less children go outside and engage in active play as technology, such as television and video games, keep children indoors.
- Rather than walking or biking to a bus-stop or directly to school, more school-age children are driven to school by their parents, reducing physical activity.
- As family sizes decrease, the children's pester power, their ability to force adults to do what they want, increases. This ability enables them to have easier access to calorie-packed foods, such as candy and soda drinks.
- The social context around family meal-time plays a role in rates of childhood obesity
Social policies

Different communities and nations have adopted varying social practices and policies that are either beneficial or detrimental to children's physical health. These social factors include:[5]
- the quality of school lunches
- the emphasis of schools on physical activity
- access to vending machines and fast-food restaurants
- prevalence of and access to parks, bike paths, and sidewalks
- government subsidies for corn oil and sugar
- advertising of fast-food restaurants and candy
- prices of healthy and unhealthy foods
- access to fresh, healthy, and affordable food[40]
Advertising
Advertising of unhealthy foods correlates with childhood obesity rates.[5] In some nations, advertising of candy, cereal, and fast-food restaurants is illegal or limited on children's television channels.[41] The media defends itself by blaming the parents for yielding to their children's demands for unhealthy foods.[5]
Socioeconomic status
It is much more common for young people who come from a racial or ethnic minority, or for those who have a lower socioeconomic status, to be overweight and to engage in less healthy behaviors and sedentary activities.[42]
Prevention
.jpg.webp)
Schools play a large role in preventing childhood obesity by providing a safe and supporting environment with policies and practices that support healthy behaviors.[43] At home, parents can help prevent their children from becoming overweight by changing the way the family eats and exercises together. The best way children learn is by example, so parents should lead by example by living a healthy lifestyle.[44] Screening for obesity is recommended in those over the age of six.[45] Both physical activity and diet can help to reduce the risk of obesity in children from 0 to 5 years old; meanwhile, exclusive physical activity can reduce the risk of obesity for children aged from 6 to 12 years old, and adolescents aged from 13 to 18 years old.[46] The implementation of strategies to improve childcare services such as preschools, nurseries, daycare, and kindergarten on healthy eating, physical activity, and obesity prevention shows little effect on a child's diet, physical activity, and weight status.[47]
Maternal Body Mass Index
Maternal body mass index (BMI) is an important predictor of childhood obesity. Mothers with pre-pregnancy obesity, as defined by BMI ≥30 kg/m2, are known to have children that have higher growth rates and more likely to have obesity.[48]
Dietary
The effects of eating habits on childhood obesity are difficult to determine. A three-year randomized controlled study of 1,704 3rd grade children which provided two healthy meals a day in combination with an exercise program and dietary counsellings failed to show a significant reduction in percentage body fat when compared to a control group. This was partly due to the fact that even though the children believed they were eating less their actual calorie consumption did not decrease with the intervention. At the same time observed energy expenditure remained similar between the groups. This occurred even though dietary fat intake decreased from 34% to 27%.[49] A second study of 5,106 children showed similar results. Even though the children ate an improved diet there was no effect found on BMI.[50] Why these studies did not bring about the desired effect of curbing childhood obesity has been attributed to the interventions not being sufficient enough. Changes were made primarily in the school environment while it is felt that they must occur in the home, the community, and the school simultaneously to have a significant effect.[37]
A Cochrane review of a lower fat diet in children (30% or less of total energy) to prevent obesity found the existing evidence of very low to moderate quality, and firm conclusions could not be made.[51]
Calorie-rich drinks and foods are readily available to children. Consumption of sugar-laden soft drinks may contribute to childhood obesity. In a study of 548 children over a 19-month period the likelihood of obesity increased 1.6 times for every additional soft drink consumed per day.[52][53]
Calorie-dense, prepared snacks are available in many locations frequented by children. As childhood obesity has become more prevalent, snack vending machines in school settings have been reduced by law in a small number of localities. Some research suggests that the increase in availability of junk foods in schools can account for about one-fifth of the increase in average BMI among adolescents over the last decade.[54] Eating at fast food restaurants is very common among young people with 75% of 7th to 12th grade students consuming fast food in a given week.[55] The fast food industry is also at fault for the rise in childhood obesity. This industry spends about $4.2 billion on advertisements aimed at young children. McDonald's alone has thirteen websites that are viewed by 365,000 children and 294,000 teenagers each month. In addition, fast food restaurants give out toys in children's meals, which helps to entice children to buy the fast food. According to a 2010 report, 40% of children aged 2 to 11 asked their parents to take them to McDonald's at least once a week, and 15%of preschoolers asked to go every day.[56][57] To make matters worse, out of 3000 combinations created from popular items on children's menus at fast food restaurants, only 13 meet the recommended nutritional guidelines for young children.[58] Some literature has found a relationship between fast food consumption and obesity.[59] Including a study which found that fast food restaurants near schools increases the risk of obesity among the student population.[60]
Whole milk consumption verses 2% milk consumption in children of one to two years of age had no effect on weight, height, or body fat percentage. Therefore, whole milk continues to be recommended for this age group. However the trend of substituting sweetened drinks for milk has been found to lead to excess weight gain.[61]
Legal
Some jurisdictions use laws and regulations in an effort to steer children and parents towards making healthier food choices. Two examples are calorie count laws and banning soft drinks from sale at vending machines in schools.[62] In the United Kingdom the Obesity Health Alliance has called on whichever party wins the general election to take measures to reduce childhood obesity, for example by banning advertisements for unhealthy foods before 9:00 pm and banning sports sponsorship by manufacturers of unhealthy foods. The failure of the present UK government to cut sugar, fat and salt content in foods has been criticised.[63] Health experts, the health select committee and campaigners described Conservative plans over childhood obesity as, "weak" and "watered down".[64]
Physical activity

Physical inactivity of children has also shown to be a serious cause, and children who fail to engage in regular physical activity are at greater risk of obesity. Researchers studied the physical activity of 133 children over a three-week period using an accelerometer to measure each child's level of physical activity. They discovered the obese children were 35% less active on school days and 65% less active on weekends compared to non-obese children.
Physical inactivity as a child could result in physical inactivity as an adult. In a fitness survey of 6,000 adults, researchers discovered that 25% of those who were considered active at ages 14 to 19 were also active adults, compared to 2% of those who were inactive at ages 14 to 19, who were now said to be active adults.[65] Staying physically inactive leaves unused energy in the body, most of which is stored as fat. Researchers studied 16 men over a 14-day period and fed them 50% more of their energy required every day through fats and carbohydrates. They discovered that carbohydrate overfeeding produced 75–85% excess energy being stored as body fat and fat overfeeding produced 90–95% storage of excess energy as body fat.[66]
Many children fail to exercise because they spend long periods of time engaging in sedentary activities such as computer usage, playing video games or watching television. Technology has a large factor on the children's activeness. Researchers provided a technology questionnaire to 4,561 children, ages 14, 16, and 18. They discovered children were 21.5% more likely to be overweight when watching 4+ hours of TV per day, 4.5% more likely to be overweight when using a computer one or more hours per day, and unaffected by potential weight gain from playing video games.[66] A randomized trial showed that reducing TV viewing and computer use can decrease age-adjusted BMI; reduced calorie intake was thought to be the greatest contributor to the BMI decrease.[67]
Technological activities are not the only household influences of childhood obesity. Low-income households can affect a child's tendency to gain weight. Over a three-week period researchers studied the relationship of socioeconomic status (SES) to body composition in 194 children, ages 11–12. They measured weight, waist girth, stretch stature, skinfolds, physical activity, TV viewing, and SES; researchers discovered clear SES inclines to upper class children compared to the lower class children.[68]
Childhood inactivity is linked to obesity in the United States with more children being overweight at younger ages. In a 2009 preschool study 89% of a preschoolers' day was found to be sedentary while the same study also found that even when outside, 56 percent of activities were still sedentary. One factor believed to contribute to the lack of activity found was little teacher motivation,[69] but when toys, such as balls were made available, the children were more likely to play.[69]
Home environment
Children's food choices are also influenced by family meals. Researchers provided a household eating questionnaire to 18,177 children, ranging in ages 11–21, and discovered that four out of five parents let their children make their own food decisions. They also discovered that compared to adolescents who ate three or fewer meals per week, those who ate four to five family meals per week were 19% less likely to report poor consumption of vegetables, 22% less likely to report poor consumption of fruits, and 19% less likely to report poor consumption of dairy foods. Adolescents who ate six to seven family meals per week, compared to those who ate three or fewer family meals per week, were 38% less likely to report poor consumption of vegetables, 31% less likely to report poor consumption of fruits, and 27% less likely to report poor consumption of dairy foods.[70] The results of a survey in the UK published in 2010 imply that children raised by their grandparents are more likely to be obese as adults than those raised by their parents.[71] An American study released in 2011 found the more mothers work the more children are more likely to be overweight or obese.[72]
Developmental factors
Various developmental factors may affect rates of obesity. Breast-feeding for example may protect against obesity in later life with the duration of breast-feeding inversely associated with the risk of being overweight later on.[73] A child's body growth pattern may influence the tendency to gain weight. Researchers measured the standard deviation (SD [weight and length]) scores in a cohort study of 848 babies. They found that infants who had an SD score above 0.67 had catch up growth (they were less likely to be overweight) compared to infants who had less than a 0.67 SD score (they were more likely to gain weight).[74] Additionally, breastfeeding for less than 6 months, compared to 6 months or more, has been shown to result in a higher growth rate and higher zBMI at 18, 36, and 72 months of age.[48]
A child's weight may be influenced when he/she is only an infant. Researchers also did a cohort study on 19,397 babies, from their birth until age seven and discovered that high weight babies at four months were 1.38 times more likely to be overweight at seven years old compared to normal weight babies. High weight babies at the age of one were 1.17 times more likely to be overweight at age seven compared to normal weight babies.[75]
Medical illness
Cushing's syndrome (a condition in which the body contains excess amounts of cortisol) may also influence childhood obesity. Researchers analyzed two isoforms (proteins that have the same purpose as other proteins, but are programmed by different genes) in the cells of 16 adults undergoing abdominal surgery. They discovered that one type of isoform created oxo-reductase activity (the alteration of cortisone to cortisol) and this activity increased 127.5 pmol mg sup when the other type of isoform was treated with cortisol and insulin. The activity of the cortisol and insulin can possibly activate Cushing's syndrome.[76]
Hypothyroidism is a hormonal cause of obesity, but it does not significantly affect obese people who have it more than obese people who do not have it. In a comparison of 108 obese patients with hypothyroidism to 131 obese patients without hypothyroidism, researchers discovered that those with hypothyroidism had only 0.077 points more on the caloric intake scale than did those without hypothyroidism.[77]
Psychological factors
Researchers surveyed 1,520 children, ages 9–10, with a four-year follow up and discovered a positive correlation between obesity and low self-esteem in the four-year follow up. They also discovered that decreased self-esteem led to 19% of obese children feeling sad, 48% of them feeling bored, and 21% of them feeling nervous. In comparison, 8% of normal weight children felt sad, 42% of them felt bored, and 12% of them felt nervous.[78]
Stress can influence a child's eating habits. Researchers tested the stress inventory of 28 college females and discovered that those who were binge eating had a mean of 29.65 points on the perceived stress scale, compared to the control group who had a mean of 15.19 points.[79] This evidence may demonstrate a link between eating and stress.
Feelings of depression can cause a child to overeat. Researchers provided an in-home interview to 9,374 adolescents, in grades seven through 12 and discovered that there was not a direct correlation with children eating in response to depression. Of all the obese adolescents, 8.2% had said to be depressed, compared to 8.9% of the non-obese adolescents who said they were depressed.[80] Antidepressants, however, seem to have very little influence on childhood obesity. Researchers provided a depression questionnaire to 487 overweight/obese subjects and found that 7% of those with low depression symptoms were using antidepressants and had an average BMI score of 44.3, 27% of those with moderate depression symptoms were using antidepressants and had an average BMI score of 44.7, and 31% of those with major depression symptoms were using antidepressants and had an average BMI score of 44.2.[81]
Several studies have also explored the connection between Attention-deficit Hyperactivity Disorder (ADHD) and obesity in children. A study in 2005 concluded that within a subgroup of children who were hospitalized for obesity, 57.7% had co-morbid ADHD.[82] This relationship between obesity and ADHD may seem counter-intuitive, as ADHD is typically associated with higher level of energy expenditure, which is thought of as a protective factor against obesity.[83] However, these studies determined that children exhibited more signs of predominantly inattentive-type ADHD rather than combined-type ADHD. It is possible, however, that the symptoms of hyperactivity typically present in individuals with combined-type ADHD are simply masked in obese children with ADHD due to their decreased mobility.[82] The same correlation between obesity and ADHD is also present in adult populations.[84] Existing underlying explanations for the relationship between ADHD and obesity in children include but are not limited to abnormalities in the hypo-dopaminergic pathway, ADHD creating abnormal eating behaviors which leads to obesity, or impulsivity associated with binge eating leading to ADHD in obese patients.[84][85] A systematic review of the literature on the relationship between obesity and ADHD concluded that all reviewed studies reported ADHD patients were heavier than expected.[85] However, the same systematic review also claimed that all the evidence supporting this connection was still limited and further research is still necessary to learn more about this connection.[85] Given the prevalence rates of both obesity and ADHD in children, understanding the possible relationship between the two is important for public health, particularly when exploring treatment and management options.
Direct intervention for psychological treatment of childhood obesity has become more prevalent in recent years. A meta-analysis of the psychological treatment of obesity in children and adolescents found family-based behavioral treatment (FBT) and Parent-Only Behavior treatment to be the most effective practices in treating obesity in children within a psychological framework.[86]
Management

Obesity in children is treated with dietary changes and physical activity. Dieting and missing meals should; however, be discouraged.[87] The benefit of tracking BMI and providing counselling around weight is minimal.[88]
Lifestyle
Exclusive breast-feeding is recommended in all newborn infants for its nutritional and other beneficial effects.[73] Parents changing the diet and lifestyle of their offspring by offering appropriate food portions, increasing physical activity, and keeping sedentary behaviors at a minimum may also decrease the obesity levels in children.[89]
If children were more mobile and less sedentary, the rate of obesity would decrease. Parents should recognize the signs and encourage their children to be more physically active. By walking or riding a bike, instead of using motorised transport or watching television, will reduce sedentary activity.[90]
Medications
There are no medications currently approved for the treatment of obesity in children. The American Academy of Pediatrics recommends medications for obesity be discourage.[87] Orlistat and sibutramine may be helpful in managing moderate obesity in adolescence.[73] Metformin is minimally useful.[91] A Cochrane review in 2016 concluded that medications might reduce BMI and bodyweight to a small extent in obese children and adolescents. This conclusion was based only on low quality evidence.[92]
Surgery
As of 2015 there is not good evidence comparing surgery to lifestyle change for obesity in children, though there are a number of high quality ongoing studies looking at this issue.[93] Bariatric surgical procedures are increasingly used amongst adolescents with severe adolescent obesity to promote weight loss.[94]
Epidemiology
From 1980 to 2013, the prevalence of overweight and obesity in children increased by nearly 50%.[95] Currently 10% of children worldwide are either overweight or obese.[2] In 2014, the World Health Organization established a high-level commission to end childhood obesity.[96]
With more than 42 million overweight children around the world, childhood obesity is increasing worldwide.[5] Since 1980, the number of obese children has doubled in all three North American countries, Mexico, the United States, and Canada.[97] Although the rate of childhood obesity in the United States has stopped increasing, the current rate remains high. In 2010, 32.6 percent of 6- to 11-year-olds were overweight, and 18 percent of 6- to 9-year-olds were obese.[97]
Canada
The rate of overweight and obesity among Canadian children has increased dramatically in recent years. In boys, the rate increased from 11% in the 1980s to 30% in the 1990s.[98]
Brazil
The rate of overweight and obesity in Brazilian children increased from 4% in the 1980s to 14% in the 1990s.[98] In 2007 the prevalence of children overweight and childhood obesity was 11.1% and 2.7% in girls, 8.2% and 1.5% in boys, respectively.[99]
United States
The rate of obesity among children and adolescents in the United States has nearly tripled between the early 1980s and 2000. It has however not changed significantly between 2000 and 2006 with the most recent statistics showing a level just over 17 percent.[100] In 2008, the rate of overweight and obese children in the United States was 32%, and had stopped climbing.[101] In 2011, a national cohort study of infants and toddlers found that nearly one-third of US children were overweight or obese at 9 months and 2 years old.[102] In a follow-up study, infant weight status (healthy and obese) was strongly associated with preschool weight status.[103]
Australia
Since the onset of the 21st century, Australia has found that childhood obesity has followed trend with the United States. Information garnered has concluded that the increase has occurred in the lower socioeconomic areas where poor nutritional education has been blamed.
Research
A study of 1800 children aged 2 to 12 in Colac, Australia tested a program of restricted diet (no carbonated drinks or sweets) and increased exercise. Interim results included a 68% increase in after school activity programs, 21% reduction in television viewing, and an average of 1 kg weight reduction compared to a control group.[104]
A survey carried out by the American Obesity Association into parental attitudes towards their children's weight showed the majority of parents think that recess should not be reduced or replaced. Almost 30% said that they were concerned with their child's weight. 35% of parents thought that their child's school was not teaching them enough about childhood obesity, and over 5% thought that childhood obesity was the greatest risk to their child's long-term health.[105]
A Northwestern University study indicates that inadequate sleep has a negative impact on a child's performance in school, their emotional and social welfare, and increases their risk of being overweight. This study was the first nationally represented, longitudinal investigation of the correlation between sleep, Body Mass Index (BMI) and overweight status in children between the ages of 3 and 18. The study found that an extra hour of sleep lowered the children's risk of being overweight from 36% to 30%, while it lessened older children's risk from 34% to 30%.[106]
A 2018 Cochrane review on the impact of physical activity, diet and other behavioral interventions for improving cognition and school achievement in children and adolescents found that school and community-based programs as part of an overall prevention program were beneficial.[107]
Obese children and adolescents are more likely to become obese as adults. For example, one study found that approximately 80% of children who were overweight at aged 10–15 years were obese adults at age 25 years. Another study found that 25% of obese adults were overweight as children. The latter study also found that if overweight begins before 8 years of age, obesity in adulthood is likely to be more severe.[108]
A study has also found that tackling childhood obesity will not necessarily lead to eating disorders later in life.[109]
A review of secular trends in the number of overweight or obese children have come to the conclusion that prevalence had increased during the past two decades in the most industrialised countries, apart from Russia and Poland, and in several low-income countries, especially in urban areas. Prevalence doubled or tripled between the early 1970s and late 1990s in Australia, Brazil, Canada, Chile, Finland, France, Germany, Greece, Japan, the UK, and the USA. By 2010, more than 40% of children in the North American and eastern Mediterranean WHO regions, 38% in Europe, 27% in the western Pacific, and 22% in southeast Asia were predicted to be overweight or obese. However, that 2006 review pre-dates recent data, which, although still too soon to be certain, suggest that the increase in childhood obesity in the US, the UK, and Sweden might be abating.3–5 [110]
A British longitudinal study has found that obesity restricted to childhood has minimal influence on adult outcomes at age 30. The study also found that, while obesity that continues into adulthood has little influence on men's outcomes, it makes women less likely to have ever been employed or to currently have a romantic partner.[111]
A 2017 National Bureau of Economic Research paper found that childhood obesity in the United States increases medical costs by $1,354 a year (in 2013 dollars).[112]
See also
- International Journal of Pediatric Obesity
- Task Force on Childhood Obesity
- Classification of childhood obesity
- Obesity and the environment
- Social influences on fitness behavior
- Social stigma of obesity
- Sugary drink tax
- EPODE International Network
Transport:
- Active mobility
- Children's street culture
- Children's street games
- Cycling mobility
- Home zone / Play street
- Obesity and walking
- Student transport
- Walking bus
Footnotes
- Kopelman, Peter G (2005). Clinical obesity in adults and children: In Adults and Children. Blackwell Publishing. p. 493. ISBN 978-1-4051-1672-5.
- Bessesen DH (June 2008). "Update on obesity". J. Clin. Endocrinol. Metab. 93 (6): 2027–34. doi:10.1210/jc.2008-0520. PMID 18539769.
- Shah, Bindra; Cost, Katherine Tombeau; Fuller, Anne; Birken, Catherine S.; Anderson, Laura N. (8 September 2020). "Sex and gender differences in childhood obesity: contributing to the research agenda". BMJ Nutrition, Prevention & Health. 3 (2): 387–390. doi:10.1136/bmjnph-2020-000074. ISSN 2516-5542. PMC 7841817. PMID 33521549. Retrieved 30 November 2020.
- Deurenberg P, Weststrate JA, Seidell JC (March 1991). "Body mass index as a measure of body fatness: age- and sex-specific prediction formulas". Br. J. Nutr. 65 (2): 105–14. doi:10.1079/BJN19910073. PMID 2043597.
- Berger, Kathleen Stassen (2014). Invitation to the Life Span, Second Edition. New York: Worth Publishers. p. 247. ISBN 978-1464172052.
- "Healthy Weight: Assessing Your Weight: BMI: About BMI for Children and Teens". CDC.
- "Experts Available to Discuss Childhood Obesity, Role of BMI". Business Wire ExpertSource Group. 2005. Archived from the original on 22 March 2018. Retrieved 15 December 2013.
- Javed, A.; Jumean, M.; Murad, M. H.; Okorodudu, D.; Kumar, S.; Somers, V. K.; Sochor, O.; Lopez-Jimenez, F. (2015). "Diagnostic performance of body mass index to identify obesity as defined by body adiposity in children and adolescents: a systematic review and meta-analysis". Pediatric Obesity. 10 (3): 234–244. doi:10.1111/ijpo.242. PMID 24961794. S2CID 1079629.
- Great Britain Parliament House of Commons Health Committee (May 2004). Obesity - Volume 1 - HCP 23-I, Third Report of session 2003-04. Report, together with formal minutes. London, UK: TSO (The Stationery Office). ISBN 978-0-215-01737-6. Retrieved 2007-12-17.
- Janssen I, Craig WM, Boyce WF, Pickett W (2004). "Associations between overweight and obesity with bullying behaviors in school-aged children". Pediatrics. 113 (5): 1187–94. doi:10.1542/peds.113.5.1187. PMID 15121928.
- Obesity.Org
- "SRTS Guide: Health Risks". Archived from the original on 2011-03-21. Retrieved 2011-07-04.
- Childhood obesity - CNN
- "Childhood Obesity". Archived from the original on 2015-09-24. Retrieved 2006-09-14.
- Childhood obesity: Complications - MayoClinic.com
- Must, A; Strauss, R S (1999-04-01). "Risks and consequences of childhood and adolescent obesity". Nature. 23: S2–S11. doi:10.1038/sj.ijo.0800852. PMID 10340798.
- Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH (November 1992). "Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935". The New England Journal of Medicine. 327 (19): 1350–5. doi:10.1056/NEJM199211053271904. PMID 1406836.
- "Obese kids have arteries of 45-year-olds: study". CTV News. 11 November 2008. Retrieved 2008-11-11.
- Polotsky AJ, Hailpern SM, Skurnick JH, Lo JC, Sternfeld B, Santoro N (April 2010). "Association of adolescent obesity and lifetime nulliparity—the Study of Women's Health Across the Nation (SWAN)". Fertil. Steril. 93 (6): 2004–11. doi:10.1016/j.fertnstert.2008.12.059. PMC 2891509. PMID 19185860.
- Cornette R (2008). "The emotional impact of obesity on children". Worldviews Evid Based Nurs. 5 (3): 136–41. doi:10.1111/j.1741-6787.2008.00127.x. PMID 19076912.
- Uptodate.com|http://www.uptodate.com/online/content/topic.do?topicKey=pedigast/13911#25 Archived 2009-02-03 at the Wayback Machine
- https://www.cdc.gov/healthyyouth/obesity/facts.htm Archived 2018-03-17 at the Wayback Machine, Adolescent and school health, CDC
- Belluck, Pam (17 March 2005). "Children's Life Expectancy Being Cut Short by Obesity". The New York Times.
- Ebbeling CB, Pawlak DB, Ludwig DS (2002). "Childhood obesity: public-health crisis, common sense cure". Lancet. 360 (9331): 473–82. doi:10.1016/S0140-6736(02)09678-2. PMID 12241736. S2CID 6374501.
- Dietz WH (1998). "Health consequences of obesity in youth: childhood predictors of adult disease". Pediatrics. 101 (3 Pt 2): 518–25. doi:10.1542/peds.101.S2.518. PMID 12224658. S2CID 8306697.
- Speiser PW, Rudolf MC, Anhalt H, et al. (2005). "Childhood obesity". J. Clin. Endocrinol. Metab. 90 (3): 1871–87. doi:10.1210/jc.2004-1389. PMID 15598688.
- Kimm SY, Obarzanek E (2002). "Childhood obesity: a new pandemic of the new millennium". Pediatrics. 110 (5): 1003–7. doi:10.1542/peds.110.5.1003. PMID 12415042.
- Miller J, Rosenbloom A, Silverstein J (2004). "Childhood obesity". J. Clin. Endocrinol. Metab. 89 (9): 4211–8. doi:10.1210/jc.2004-0284. PMID 15356008.
- McBride, D. (2010). Childhood obesity. Practice Nurse, 39(11), 40-45
- Cole T.J. (2006). Early Causes of Childhood Obesity and Implications for Prevention. Retrieved December 1, 2011, from http://discovery.ucl.ac.uk/14548/1/14548.pdf Archived 2018-07-23 at the Wayback Machine
- Han JC, Lawlor DA, Kimm SY (2010). "Childhood obesity". Lancet. 375 (9727): 1737–1748. doi:10.1016/S0140-6736(10)60171-7. PMC 3073855. PMID 20451244.
- Seipel, M. M.; Shafer, K (2013). "The effect of prenatal and postnatal care on childhood obesity". Social Work. 58 (3): 241–52. doi:10.1093/sw/swt025. PMID 24032305.
- Gluckman, Peter; Hanson, Mark A. (2006). Developmental origins of health and disease. Cambridge University Press. doi:10.1017/CBO9780511544699. ISBN 9780511544699.
- Frayling, Timothy M. (May 11, 2007). "A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity". Science. 316 (5826): 889–894. Bibcode:2007Sci...316..889F. doi:10.1126/science.1141634. PMC 2646098. PMID 17434869.
- Farooqi, I. Sadaf; O'Rahilly, Stephen (2006). "Genetics of Obesity in Humans". Endocrine Reviews. 27 (7): 710–718. doi:10.1210/er.2006-0040. PMID 17122358.
- Farooqi IS (September 2005). "Genetic and hereditary aspects of childhood obesity". Best Practirce Resesearch: Clinical Endocrinology & Metabolism. 19 (3): 359–74. doi:10.1016/j.beem.2005.04.004. PMID 16150380.
- Kolata G (2007). Rethinking Thin: The new science of weight loss — and the myths and realities of dieting. Picador. ISBN 978-0-312-42785-6.
- Yang W, Kelly T, He J (2007). "Genetic epidemiology of obesity". Epidemiol Rev. 29: 49–61. doi:10.1093/epirev/mxm004. PMID 17566051.
- Melnik, Bodo C. (2012-01-01). "Excessive Leucine-mTORC1-Signalling of Cow Milk-Based Infant Formula: The Missing Link to Understand Early Childhood Obesity". Journal of Obesity. 2012: 197653. doi:10.1155/2012/197653. ISSN 2090-0716. PMC 3317169. PMID 22523661.
- Howlett, Elizabeth; Davis, Cassandra; Burton, Scot (2015). "From Food Desert to Food Oasis: The Potential Influence of Food Retailers on Childhood Obesity Rates". Journal of Business Ethics. 139 (2): 215–224. doi:10.1007/s10551-015-2605-5. S2CID 154755082.
- Lobstein, Tim; Dibb, Sue (2005). "Evidence of a possible link between obesogenic food advertising and child overweight". Obesity Reviews. 6 (3): 203–208. doi:10.1111/j.1467-789x.2005.00191.x. PMID 16045635. S2CID 31485597.
- Delva Jorge; O'Malley Patrick M.; Johnston Lloyd D. (2006). "Racial/Ethnic and Socioeconomic Status Differences in Overweight and Health-Related Behaviors among American Students: National Trends 1986-2003". Journal of Adolescent Health. 39 (4): 536–45. doi:10.1016/j.jadohealth.2006.02.013. PMID 16982389.
- "Adolescent and School Health". Archived from the original on 2018-03-17. Retrieved 2017-09-09.
- "Which BMI standards to use in practice?". Public Health Nutrition. 15 (8A): 1541–1542. 2012. doi:10.1017/s136898001200167x.
- US Preventive Services Task, Force.; Grossman, DC; Bibbins-Domingo, K; Curry, SJ; Barry, MJ; Davidson, KW; Doubeni, CA; Epling JW, Jr; Kemper, AR; Krist, AH; Kurth, AE; Landefeld, CS; Mangione, CM; Phipps, MG; Silverstein, M; Simon, MA; Tseng, CW (20 June 2017). "Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement". JAMA. 317 (23): 2417–2426. doi:10.1001/jama.2017.6803. PMID 28632874.
- Brown T, Moore TH, Hooper L, Gao Y, Zayegh A, Ijaz S, Elwenspoek M, Foxen SC, Magee L, O'Malley C, Waters E, Summerbell CD (23 July 2019). "Interventions for preventing obesity in children". Cochrane Database of Systematic Reviews. 2019 (7): CD001871. doi:10.1002/14651858.CD001871.pub4. PMC 6646867. PMID 31332776.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Wolfenden L, Barnes C, Jones J, Finch M, Wyse RJ, Kingsland M, Tzelepis M, Grady A, Hodder RK, Booth D, Yoong SL (10 February 2020). "Strategies to Improve the Implementation of Healthy Eating, Physical Activity and Obesity Prevention Policies, Practices or Programmes Within Childcare Services". Cochrane Database of Systematic Reviews. 2020 (2): CD011779. doi:10.1002/14651858.CD011779.pub3. PMC 7008062. PMID 32036618.
- Eny, Karen M.; Chen, Shiyi; Anderson, Laura N.; Chen, Yang; Lebovic, Gerald; Pullenayegum, Eleanor; Parkin, Patricia C.; Maguire, Jonathon L.; Birken, Catherine S.; Collaboration, TARGet Kids! (1 April 2018). "Breastfeeding duration, maternal body mass index, and birth weight are associated with differences in body mass index growth trajectories in early childhood". The American Journal of Clinical Nutrition. 107 (4): 584–592. doi:10.1093/ajcn/nqx081. ISSN 0002-9165. PMID 29635496. Retrieved 30 November 2020.
- Caballero B, Clay T, Davis SM, et al. (November 2003). "Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren". Am. J. Clin. Nutr. 78 (5): 1030–8. doi:10.1093/ajcn/78.5.1030. PMC 4863237. PMID 14594792.
- Nader PR, Stone EJ, Lytle LA, et al. (July 1999). "Three-year maintenance of improved diet and physical activity: the CATCH cohort. Child and Adolescent Trial for Cardiovascular Health". Arch Pediatr Adolesc Med. 153 (7): 695–704. doi:10.1001/archpedi.153.7.695. PMID 10401802.
- Naude, Celeste E.; Visser, Marianne E.; Nguyen, Kim A.; Durao, Solange; Schoonees, Anel (5 July 2018). "Effects of total fat intake on bodyweight in children". The Cochrane Database of Systematic Reviews. 7: CD012960. doi:10.1002/14651858.CD012960.pub2. ISSN 1469-493X. PMC 6513603. PMID 29974953.
- Emmett, Pauline M.; Jones, Louise R. (2015-10-01). "Diet, growth, and obesity development throughout childhood in the Avon Longitudinal Study of Parents and Children". Nutrition Reviews. 73 Suppl 3: 175–206. doi:10.1093/nutrit/nuv054. ISSN 1753-4887. PMC 4586450. PMID 26395342.
- James J, Kerr D (2005). "Prevention of childhood obesity by reducing soft drinks". Int J Obes (Lond). 29 (Suppl 2): S54–7. doi:10.1038/sj.ijo.0803062. PMID 16385753.
- "Federal Reserve Bank of Chicago, Reading, Writing, and Raisinets: Are School Finances Contributing to Children's Obesity?, October 2004" (PDF). Archived from the original (PDF) on 2012-10-21. Retrieved 2013-02-04.
- French SA, Story M, Neumark-Sztainer D, Fulkerson JA, Hannan P (2001). "Fast food restaurant use among adolescents: associations with nutrient intake, food choices and behavioral and psychosocial variables". Int. J. Obes. Relat. Metab. Disord. 25 (12): 1823–33. doi:10.1038/sj.ijo.0801820. PMID 11781764.
- Huget, Jennifer LaRue (11 August 2010). "Kids get an eyeful of fast-food marketing". The Washington Post. Retrieved 1 June 2022.
- "Fast Food Restaurants Dish Up Unhealthy Marketing to Youth; Researchers Release Unprecedented Report on Fast Food Nutrition and Marketing". YaleNews. 2010-11-08. Retrieved 2022-06-01.
- Tracy, Ben. "Fast Food Restaurants Not Fighting Child Obesity - CBS Evening News - CBS News." Breaking News Headlines: Business, Entertainment & World News - CBS News. CBS Evening News, 8 Nov. 2010. Web. 22 Nov. 2010. <http://www.cbsnews.com/stories/2010/11/08/eveningnews/main7035550.shtml>.
- Thompson OM, Ballew C, Resnicow K, et al. (2004). "Food purchased away from home as a predictor of change in BMI z-score among girls". Int. J. Obes. Relat. Metab. Disord. 28 (2): 282–9. doi:10.1038/sj.ijo.0802538. PMID 14647177.
- Davis B, Carpenter C (December 2008). "Proximity of Fast-Food Restaurants to Schools and Adolescent Obesity". Am J Public Health. 99 (3): 505–10. doi:10.2105/AJPH.2008.137638. PMC 2661452. PMID 19106421.
- Allen RE, Myers AL (November 2006). "Nutrition in toddlers". American Family Physician. 74 (9): 1527–32. PMID 17111891.
- Reinehr T, Wabitsch M (2011). "Childhood Obesity". Current Opinion in Lipidology. 22 (1): 21–25. doi:10.1097/MOL.0b013e32833f9c37. PMID 20871401. S2CID 11863960.
- UK must get tough on childhood obesity, says top doctors The Guardian
- General election 2017: Labour proposes junk food ad ban BBC
- Ortega FB, Ruiz JR, Castillo MJ, Sjöström M (2007). "Physical fitness in childhood and adolescence: a powerful marker of health". Int J Obes (Lond). 32 (1): 1–11. doi:10.1038/sj.ijo.0803774. PMID 18043605.
- Horton TJ, Drougas H, Brachey A, Reed GW, Peters JC, Hill JO (1995). "Fat and carbohydrate overfeeding in humans: different effects on energy storage". Am. J. Clin. Nutr. 62 (1): 19–29. doi:10.1093/ajcn/62.1.19. PMID 7598063.
- Epstein LH, Roemmich JN, Robinson JL, et al. (March 2008). "A randomized trial of the effects of reducing television viewing and computer use on body mass index in young children". Arch Pediatr Adolesc Med. 162 (3): 239–45. doi:10.1001/archpediatrics.2007.45. PMC 2291289. PMID 18316661.
- Lluch A, Herbeth B, Méjean L, Siest G (2000). "Dietary intakes, eating style and overweight in the Stanislas Family Study". Int. J. Obes. Relat. Metab. Disord. 24 (11): 1493–9. doi:10.1038/sj.ijo.0801425. PMID 11126347.
- "The Inactivity Of Preschoolers Amid Rising Childhood Obesity". Medical News Today. February 2009. Archived from the original (Summarized from Child Development, Vol. 80, Issue 1, Social and Environmental Factors Associated with Preschoolers' Non-sedentary Physical Activity by Brown, WH (University of South Carolina), Pfeiffer, KA (Michigan State University), McIver, KL (East Carolina University), Dowda, M, Addy, CL, and Pate, RR (University of South Carolina).) on February 11, 2009. Retrieved September 25, 2010.
- Videon TM, Manning CK (2003). "Influences on adolescent eating patterns: the importance of family meals". J Adolesc Health. 32 (5): 365–73. doi:10.1016/S1054-139X(02)00711-5. PMID 12729986.
- Wilkinson, Emma (2010-02-15). "Grandparents 'boost obesity risk'". BBC News. Retrieved 2010-04-28.
- "Childhood obesity risk tied to amount of work mother does lineup announced". Sydney Morning Herald. 8 February 2011. Retrieved 8 February 2011.
- "North American Society for Pediatric Gastroenterology, Hepatology and Nutrition" (PDF). Archived from the original (PDF) on 2016-03-03. Retrieved 2008-08-27.
- Ong KK, Ahmed ML, Emmett PM, et al. (2000). "Association between postnatal catch-up growth and obesity in childhood: prospective cohort study". BMJ. 320 (7240): 967–71. doi:10.1136/bmj.320.7240.967. PMC 27335. PMID 10753147.
- Stettler N, Zemel BS, Kumanyika S, Stallings VA (2002). "Infant weight gain and childhood overweight status in a multicenter, cohort study". Pediatrics. 109 (2): 194–9. doi:10.1542/peds.109.2.194. PMID 11826195.
- Bujalska IJ, Kumar S, Stewart PM (1997). "Does central obesity reflect "Cushing's disease of the omentum"?". Lancet. 349 (9060): 1210–3. doi:10.1016/S0140-6736(96)11222-8. PMID 9130942. S2CID 24643796.
- Tagliaferri M, Berselli ME, Calò G, et al. (2001). "Subclinical hypothyroidism in obese patients: relation to resting energy expenditure, serum leptin, body composition, and lipid profile". Obes. Res. 9 (3): 196–201. doi:10.1038/oby.2001.21. PMID 11323445.
- Strauss RS (2000). "Childhood obesity and self-esteem". Pediatrics. 105 (1): e15. doi:10.1542/peds.105.1.e15. PMID 10617752.
- Ogg EC, Millar HR, Pusztai EE, Thom AS (1997). "General practice consultation patterns preceding diagnosis of eating disorders". Int J Eat Disord. 22 (1): 89–93. doi:10.1002/(SICI)1098-108X(199707)22:1<89::AID-EAT12>3.0.CO;2-D. PMID 9140741.
- Goodman E, Whitaker RC (2002). "A prospective study of the role of depression in the development and persistence of adolescent obesity". Pediatrics. 110 (3): 497–504. doi:10.1542/peds.110.3.497. PMID 12205250.
- Dixon JB, Dixon ME, O'Brien PE (2003). "Depression in association with severe obesity: changes with weight loss". Arch. Intern. Med. 163 (17): 2058–65. doi:10.1001/archinte.163.17.2058. PMID 14504119.
- Agranat-Meged, Anat N.; Deitcher, Chane; Goldzweig, Gil; Leibenson, Lilach; Stein, Magda; Galili-Weisstub, Esti (May 2005). "Childhood obesity and attention deficit/hyperactivity disorder: A newly described comorbidity in obese hospitalized children". International Journal of Eating Disorders. 37 (4): 357–359. doi:10.1002/eat.20096. PMID 15856493.
- Holtkamp, K; Konrad, K; Müller, B; Heussen, N; Herpertz, S; Herpertz-Dahlmann, B; Hebebrand, J (16 March 2004). "Overweight and obesity in children with Attention-Deficit/Hyperactivity Disorder". International Journal of Obesity. 28 (5): 685–689. doi:10.1038/sj.ijo.0802623. PMID 15024399.
- Pagoto, Sherry L.; Curtin, Carol; Lemon, Stephenie C.; Bandini, Linda G.; Schneider, Kristin L.; Bodenlos, Jamie S.; Ma, Yunsheng (March 2009). "Association Between Adult Attention Deficit/Hyperactivity Disorder and Obesity in the US Population". Obesity. 17 (3): 539–544. doi:10.1038/oby.2008.587. PMC 3221303. PMID 19131944.
- Cortese, Samuele; Angriman, Marco; Maffeis, Claudio; Isnard, Pascale; Konofal, Eric; Lecendreux, Michel; Purper-Ouakil, Diane; Vincenzi, Brenda; Bernardina, Bernardo Dalla; Mouren, Marie-Christine (28 May 2008). "Attention-Deficit/Hyperactivity Disorder (ADHD) and Obesity: A Systematic Review of the Literature". Critical Reviews in Food Science and Nutrition. 48 (6): 524–537. doi:10.1080/10408390701540124. PMID 18568858. S2CID 9268010.
- Altman, Myra; Wilfley, Denise E. (2015-01-01). "Evidence update on the treatment of overweight and obesity in children and adolescents". Journal of Clinical Child and Adolescent Psychology. 44 (4): 521–537. doi:10.1080/15374416.2014.963854. ISSN 1537-4424. PMID 25496471. S2CID 24927561.
- Golden, N. H.; Schneider, M.; Wood, C. (August 2016). "Preventing Obesity and Eating Disorders in Adolescents". Pediatrics. 138 (3): e20161649. doi:10.1542/peds.2016-1649. PMID 27550979.
- Sim, LA; Lebow, J; Wang, Z; Koball, A; Murad, MH (October 2016). "Brief Primary Care Obesity Interventions: A Meta-analysis". Pediatrics. 138 (4): e20160149. doi:10.1542/peds.2016-0149. PMID 27621413.
- Han JC, Lawlor DA, Kimm SY (May 2010). "Childhood obesity". Lancet. 375 (9727): 1737–48. doi:10.1016/S0140-6736(10)60171-7. PMC 3073855. PMID 20451244.
- "Management and prevention of obesity and its complications in children and adolescents | Obesity Hub". obesity hub. Archived from the original on 2016-03-04. Retrieved 2015-09-04.
- McDonagh, MS; Selph, S; Ozpinar, A; Foley, C (Feb 2014). "Systematic review of the benefits and risks of metformin in treating obesity in children aged 18 years and younger". JAMA Pediatrics. 168 (2): 178–84. doi:10.1001/jamapediatrics.2013.4200. PMID 24343296.
- Mead, E; Atkinson, G; Richter, B; Metzendorf, MI; Baur, L; Finer, N; Corpeleijn, E; O'Malley, C; Ells, LJ (29 November 2016). "Drug interventions for the treatment of obesity in children and adolescents" (PDF). The Cochrane Database of Systematic Reviews. 11: CD012436. doi:10.1002/14651858.CD012436. PMC 6472619. PMID 27899001. Archived from the original (PDF) on 21 July 2018. Retrieved 2 August 2018.
- Ells, LJ; Mead, E; Atkinson, G; Corpeleijn, E; Roberts, K; Viner, R; Baur, L; Metzendorf, MI; Richter, B (24 June 2015). "Surgery for the treatment of obesity in children and adolescents" (PDF). The Cochrane Database of Systematic Reviews. 6 (6): CD011740. doi:10.1002/14651858.CD011740. PMID 26104326. S2CID 37383758.
- Inge, Thomas H.; Coley, R. Yates; Bazzano, Lydia A.; Xanthakos, Stavra A.; McTigue, Kathleen; Arterburn, David; Williams, Neely; Wellman, Rob; Coleman, Karen J.; Courcoulas, Anita; Desai, Nirav K. (2018). "Comparative effectiveness of bariatric procedures among adolescents: the PCORnet bariatric study". Surgery for Obesity and Related Diseases. 14 (9): 1374–1386. doi:10.1016/j.soard.2018.04.002. PMC 6165694. PMID 29793877.
- Ng, Marie; Fleming, Tom; Robinson, Margaret; Thomson, Blake; Graetz, Nicholas; Margono, Christopher; Mullany, Erin C; Biryukov, Stan; Abbafati, Cristiana; Abera, Semaw Ferede; Abraham, Jerry P; Abu-Rmeileh, Niveen M E; Achoki, Tom; Albuhairan, Fadia S; Alemu, Zewdie A; Alfonso, Rafael; Ali, Mohammed K; Ali, Raghib; Guzman, Nelson Alvis; Ammar, Walid; Anwari, Palwasha; Banerjee, Amitava; Barquera, Simon; Basu, Sanjay; Bennett, Derrick A; Bhutta, Zulfiqar; Blore, Jed; Cabral, Norberto; Nonato, Ismael Campos; et al. (May 29, 2014). "Global, regional, and national prevalence of overweight and obesity in children and adults during 1980—2013: a systematic analysis for the Global Burden of Disease Study 2013". The Lancet. 384 (9945): 766–781. doi:10.1016/S0140-6736(14)60460-8. hdl:2027.42/150584. PMC 4624264. PMID 24880830.
- Cheng, Maria (May 29, 2014). "UW study: 30 percent of world is now fat, no country immune". Seattle Times. Associated Press. Retrieved 13 November 2014.
- Ogden, Cynthia L.; Carroll, Margaret D.; Dommarco, Juan A. Rivera; Carroll, Margaret; Shields, Margot; Flegal, Katherine (2012). "Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010". Journal of the American Medical Association. 307 (5): 483–90. doi:10.1001/jama.2012.40. PMC 6362452. PMID 22253364.
- Flynn MA, McNeil DA, Maloff B, et al. (February 2006). "Reducing obesity and related chronic disease risk in children and youth: a synthesis of evidence with 'best practice' recommendations". Obes Rev. 7 (Suppl 1): 7–66. doi:10.1111/j.1467-789X.2006.00242.x. PMID 16371076. S2CID 5992031.
- Guedes DP, Rocha GD, Silva AJ, Carvalhal IM, Coelho EM,"Effects of social and environmental determinants on overweight and obesity among Brazilian schoolchildren from a developing region.", Rev Panam Salud Publica., October 30, 2011
- Ogden CL, Carroll MD, Flegal KM (May 2008). "High body mass index for age among US children and adolescents, 2003–2006". JAMA. 299 (20): 2401–5. doi:10.1001/jama.299.20.2401. PMID 18505949.
- U.S. Childhood Obesity Rates Level Off
- Moss, B.G.; Yeaton, W.H. (Jan 2011). "Young children's weight trajectories and associated risk factors: Results from the ECLS-B". American Journal of Health Promotion. 25 (3): 190–198. doi:10.4278/ajhp.090123-QUAN-29. PMID 21192749. S2CID 30422884.
- Moss, B.G.; Yeaton, W.H. (Jan 2012). "U.S. children's preschool weight status trajectories: Patterns from 9 month, 2 year, and 4 year ECLS-B data". American Journal of Health Promotion. 26 (3): 172–175. doi:10.4278/ajhp.100304-ARB-73. PMID 22208415. S2CID 207525747.
- "Obesity study bears fruit", Jamie Oliver, 24 August 2006.
- Survey on parents' perceptions of their children's weight Archived 2007-10-17 at the Wayback Machine, American Obesity Association. August, 2000. Retrieved 2006-11-21.
- Snell E, Adam EK, Duncan GJ (January–February 2007). "Sleep and the Body Mass Index and Overweight Status of Children and Adolescents". Child Development. 78 (1): 309–23. doi:10.1111/j.1467-8624.2007.00999.x. PMID 17328707.
- Martin, Anne; Booth, Josephine N.; Laird, Yvonne; Sproule, John; Reilly, John J.; Saunders, David H. (3 February 2018). "Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight". The Cochrane Database of Systematic Reviews. 2018 (3): CD009728. doi:10.1002/14651858.CD009728.pub4. ISSN 1469-493X. PMC 5865125. PMID 29499084.
- Childhood Overweight and Obesity, The Centers for Disease Control and Prevention. March, 2011. Retrieved 4/18/2011.
- "How To Deal With Overweight/Obese Children". Sydney Morning Herald. 19 October 2010. Retrieved 20 October 2010.
- Han, Joan; Debbie Lawor; Sue YS Kimm (6 May 2010). "Child Obesity". The Lancet. 375 (9727): 1737–1748. doi:10.1016/s0140-6736(10)60171-7. PMC 3073855. PMID 20451244.
- Viner, RM; Cole, TJ (11 June 2005). "Adult socioeconomic, educational, social, and psychological outcomes of childhood obesity: a national birth cohort study". BMJ (Clinical Research Ed.). 330 (7504): 1354. doi:10.1136/bmj.38453.422049.e0. PMC 558281. PMID 15901644.
- Biener, Adam I.; Cawley, John; Meyerhoefer, Chad (August 2017). "The Medical Care Costs of Youth Obesity: An Instrumental Variables Approach". NBER Working Paper No. 23682. doi:10.3386/w23682.
Further reading
- Laura Dawes, Childhood Obesity in America: Biography of an Epidemic. Cambridge, MA: Harvard University Press, 2014.
External links
- "North American Society for Pediatric Gastroenterology, Hepatology and Nutrition" (PDF). Archived from the original (PDF) on 2016-03-03. Retrieved 2008-08-27.