Human fertilization
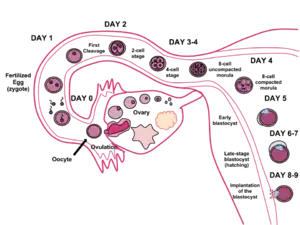
Human fertilization is the union of a human egg and sperm, occurring primarily in the ampulla of the fallopian tube.[1] The result of this union leads to the production of a fertilised egg called a zygote, initiating embryonic development. Scientists discovered the dynamics of human fertilization in the nineteenth century.[2]
| Part of a series on |
| Human growth and development |
|---|
 |
| Stages |
| Biological milestones |
|
| Development and psychology |
|
|
Developmental stage theories |
|
|
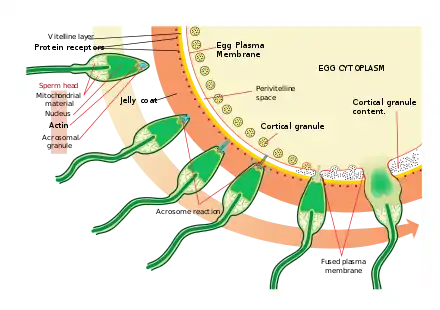


The process of fertilization involves a sperm fusing with an ovum. The most common sequence begins with ejaculation during copulation, follows with ovulation, and finishes with fertilization. Various exceptions to this sequence are possible, including artificial insemination, in vitro fertilization, external ejaculation without copulation, or copulation shortly after ovulation.[3][4] Upon encountering the secondary oocyte, the acrosome of the sperm produces enzymes which allow it to burrow through the outer shell called the zona pellucida of the egg. The sperm plasma then fuses with the egg's plasma membrane, triggering the sperm head to disconnect from its flagellum as the egg travels down the Fallopian tube to reach the uterus.
In vitro fertilization (IVF) is a process by which egg cells are fertilized by sperm outside the womb, in vitro.
History
In Antiquity, Aristotle depicted the formation of new individuals occurring through fusion of male and female fluids, with form and function emerging gradually, in a mode called by him as epigenetic.[5]
Anatomy
Ampulla
Fertilization occurs in the ampulla of the Fallopian tube, the section that curves around the ovary. Capacitated sperm are attracted to progesterone, which is secreted from the cumulus cells surrounding the oocyte.[6] Progesterone binds to the CatSper receptor on the sperm membrane and increases intracellular calcium levels, causing hyperactive motility. The sperm will continue to swim towards higher concentrations of progesterone, effectively guiding it to the oocyte.[7]
Corona radiata
The sperm binds through the corona radiata, a layer of follicle cells on the outside of the secondary oocyte. Fertilization occurs when the nucleus of both a sperm and an egg fuse to form a diploid cell, known as zygote. The successful fusion of gametes forms a new organism.
Cone of attraction and perivitelline membrane
Where the spermatozoan is about to pierce, the yolk (ooplasm) is drawn out into a conical elevation, termed the cone of attraction or reception cone. Once the spermatozoon has entered, the peripheral portion of the yolk changes into a membrane, the perivitelline membrane, which prevents the passage of additional spermatozoa.[8]
Sperm preparation
At the beginning of the process, the sperm undergoes a series of changes, as freshly ejaculated sperm is unable or poorly able to fertilize.[9] The sperm must undergo capacitation in the female's reproductive tract over several hours, which increases its motility and destabilizes its membrane, preparing it for the acrosome reaction, the enzymatic penetration of the egg's tough membrane, the zona pellucida, which surrounds the oocyte.
Zona pellucida
After binding to the corona radiata the sperm reaches the zona pellucida, which is an extracellular matrix of glycoproteins. A special complementary molecule (a receptor) on the cell surface of the sperm head binds to a ZP3 glycoprotein in the zona pellucida. This binding triggers the acrosome to burst, releasing acrosomal enzymes that help the sperm penetrate through the thick zona pellucida layer surrounding the oocyte, ultimately gaining access to the egg's cell membrane.
Some sperm cells consume their acrosome prematurely on the surface of the egg cell, facilitating the penetration by other sperm cells. As a population, mature haploid sperm cells have on average 50% genome similarity, so the premature acrosomal reactions aid fertilization by a member of the same cohort.[10] It may be regarded as a mechanism of kin selection.
Recent studies have shown that the egg is not passive during this process. In other words, they too appear to undergo changes that help facilitate such interaction. [11][12]
Cortical reaction
Once the sperm cells find their way past the zona pellucida, the cortical reaction occurs. Cortical granules inside the secondary oocyte fuse with the plasma membrane of the cell, causing enzymes inside these granules to be expelled by exocytosis to the zona pellucida. This in turn causes the glycoproteins in the zona pellucida to cross-link with each other — i.e. the enzymes cause the ZP2 to hydrolyse into ZP2f — making the whole matrix hard and impermeable to sperm. This prevents fertilization of an egg by more than one sperm. The cortical reaction and acrosome reaction are both essential to ensure that only one sperm will fertilize an egg.[13]
Fusion
After the sperm enters the cytoplasm of the oocyte, the tail and the outer coating of the sperm disintegrate and the cortical reaction takes place, preventing other sperm from fertilizing the same egg. The oocyte now undergoes its second meiotic division producing the haploid ovum and releasing a polar body. The sperm nucleus then fuses with the ovum, enabling fusion of their genetic material.
When the sperm enters the perivitelline space, a sperm-specific protein Izumo on the head binds to Juno receptors on the oocyte membrane.[14] Once it’s bound, two blocks to polyspermy then occur. After approximately 40 minutes, the other Juno receptors on the oocyte are lost from the membrane, causing it to no longer be fusogenic. Additionally, the cortical reaction will happen which is caused by ovastacin binding and cleaving ZP2 receptors on the zona pellucida.[15] These two blocks of polyspermy are what prevent the zygote from having too much DNA.
Cell membranes
The fusion of cell membranes of the secondary oocyte and sperm takes place.
Transformations
In preparation for the fusion of their genetic material both the oocyte and the sperm undergo transformations as a reaction to the fusion of cell membranes.
The oocyte completes its second meiotic division. This results in a mature ovum. The nucleus of the oocyte is called a pronucleus in this process, to distinguish it from the nuclei that are the result of fertilization.
The sperm's tail and mitochondria degenerate with the formation of the male pronucleus. This is why all mitochondria in humans are of maternal origin. Still, a considerable amount of RNA from the sperm is delivered to the resulting embryo and likely influences embryo development and the phenotype of the offspring.[16]
Replication
The pronuclei migrate toward the center of the oocyte, rapidly replicating their DNA as they do so to prepare the zygote for its first mitotic division.[17]
Mitosis
Usually 23 chromosomes from spermatozoon and 23 chromosomes from egg cell fuse (approximately half of spermatozoons carry X chromosome and the other half Y chromosome[18]). Their membranes dissolve, leaving no barriers between the male and female chromosomes. During this dissolution, a mitotic spindle forms between them. The spindle captures the chromosomes before they disperse in the egg cytoplasm. Upon subsequently undergoing mitosis (which includes pulling of chromatids towards centrioles in anaphase) the cell gathers genetic material from the male and female together. Thus, the first mitosis of the union of sperm and oocyte is the actual fusion of their chromosomes.[17]
Each of the two daughter cells resulting from that mitosis has one replica of each chromatid that was replicated in the previous stage. Thus, they are genetically identical.
Fertilization age
Fertilization is the event most commonly used to mark the beginning point in descriptions of prenatal development of the embryo or fetus. The resultant age is known as fertilization age, fertilizational age, conceptional age, embryonic age, fetal age or (intrauterine) developmental (IUD)[19] age.
Gestational age, in contrast, takes the beginning of the last menstrual period (LMP) as the start point. By convention, gestational age is calculated by adding 14 days to fertilization age and vice versa.[20] Fertilization though usually occurs within a day of ovulation, which, in turn, occurs on average 14.6 days after the beginning of the preceding menstruation (LMP).[21] There is also considerable variability in this interval, with a 95% prediction interval of the ovulation of 9 to 20 days after menstruation even for an average woman who has a mean LMP-to-ovulation time of 14.6.[22] In a reference group representing all women, the 95% prediction interval of the LMP-to-ovulation is 8.2 to 20.5 days.[21]
The average time to birth has been estimated to be 268 days (38 weeks and two days) from ovulation, with a standard deviation of 10 days or coefficient of variation of 3.7%.[23]
Fertilization age is sometimes used postnatally (after birth) as well to estimate various risk factors. For example, it is a better predictor than postnatal age for risk of intraventricular hemorrhage in premature babies treated with extracorporeal membrane oxygenation.[24]
Diseases affecting human fertility
Various disorders can arise from defects in the fertilization process. Whether that results in the process of contact between the sperm and egg, or the state of health of the biological parent carrying the zygote cell. The following are a few of the diseases that can occur and be present during the process.
- Polyspermy results from multiple sperm fertilizing an egg, leading to an offset number of chromosomes within the embryo.[25] Polyspermy, while physiologically possible in some species of vertebrates and invertebrates, is a lethal condition for the human zygote.
- Polycystic ovary syndrome is a condition in which the woman does not produce enough follicle stimulating hormone and excessively produces androgens. This results in the ovulation period between contact of the egg being postponed or excluded. [26]
- Autoimmune disorders can lead to complications in implantation of the egg in the uterus, which may be the immune system’s attack response to an established embryo on the uterine wall. [26]
- Cancer ultimately affects fertility and may lead to birth defects or miscarriages. Cancer severely damages reproductive organs, which affects fertility. [26]
- Endocrine system disorders affect human fertility by decreasing the body’s ability to produce the level of hormones needed to successfully carry a zygote. Examples of these disorders include diabetes, adrenal disorders, and thyroid disorders. [26]
- Endometriosis is a condition that affects women in which the tissue normally produced in the uterus proceeds to grow outside of the uterus. This leads to extreme amounts of pain and discomfort and may result in an irregular menstrual cycle. [26]
See also
- Spontaneous conception, the unassisted conception of a subsequent child after prior use of assisted reproductive technology
- Development of the human body
References
- Spermatogenesis — Fertilization — Contraception: Molecular, Cellular and Endocrine Events in Male Reproduction. Ernst Schering Foundation Symposium Proceedings. Springer-Verlag. 1992. ISBN 978-3-662-02817-9.
- Garrison, Fielding. An Introduction to the History of Medicine, pages 566-567 (Saunders 1921).
- "Go Ask Alice!: Pregnant without intercourse?". Archived from the original on 2011-12-22. Retrieved 2016-01-24.
- Lawyers Guide to Forensic Medicine SBN 978-1-85941-159-9 By Bernard Knight - Page 188 "Pregnancy is well known to occur from such external ejaculation ..."
- Maienschein J. 2017. The first century of cell theory: From structural units to complex living systems. In: Stadler F. (eds.), Integrated History and Philosophy of Science. Vienna Circle Institute Yearbook. Institute Vienna Circle, University of Vienna, Vienna Circle Society, Society for the Advancement of Scientific World Conceptions, vol 20. Springer, Cham. link.
- Oren-Benaroya, R.; Orvieto, R.; Gakamsky, A.; Pinchasov, M.; Eisenbach, M. (8 July 2008). "The sperm chemoattractant secreted from human cumulus cells is progesterone". Human Reproduction. 23 (10): 2339–2345. doi:10.1093/humrep/den265. PMID 18621752.
- Publicover, Steve; Barratt, Christopher (16 March 2011). "Progesterone's gateway into sperm". Nature. 471 (7338): 313–314. doi:10.1038/471313a. PMID 21412330. S2CID 205062974.
- "Fertilization of the Ovum". Gray's Anatomy. Archived from the original on 2010-12-02. Retrieved 2010-10-16.
- "Fertilization". Archived from the original on 24 June 2010. Retrieved 28 July 2010.
- Angier, Natalie (2007-06-12). "Sleek, Fast and Focused: The Cells That Make Dad Dad". The New York Times. Archived from the original on 2017-04-29.
- Suzanne Wymelenberg, Science and Babies, National Academy Press, page 17
- Richard E. Jones and Kristin H. Lopez, Human Reproductive Biology, Third Edition, Elsevier, 2006, page 238
- "Fertilization: The Cortical Reaction". Boundless. Boundless. Archived from the original on 10 April 2013. Retrieved 14 March 2013.
- Bianchi, Enrica; Wright, Gavin J (1 July 2014). "Izumo meets Juno". Cell Cycle. 13 (13): 2019–2020. doi:10.4161/cc.29461. PMC 4111690. PMID 24906131.
- Burkart, Anna D.; Xiong, Bo; Baibakov, Boris; Jiménez-Movilla, Maria; Dean, Jurrien (2 April 2012). "Ovastacin, a cortical granule protease, cleaves ZP2 in the zona pellucida to prevent polyspermy". The Journal of Cell Biology. 197 (1): 37–44. doi:10.1083/jcb.201112094. PMC 3317803. PMID 22472438.
- Jodar, Meritxell; Selvaraju, Sellappan; Sendler, Edward; Diamond, Michael P.; Krawetz, Stephen A.; Reproductive Medicine, Network. (November 2013). "The presence, role and clinical use of spermatozoal RNAs". Human Reproduction Update. 19 (6): 604–624. doi:10.1093/humupd/dmt031. PMC 3796946. PMID 23856356.
- Marieb, Elaine M. Human Anatomy and Physiology, 5th ed. pp. 1119-1122 (2001). ISBN 0-8053-4989-8
- "Five Facts about XX or XY | Gender Selection Authority". Archived from the original on 2016-10-06. Retrieved 2016-07-31.
- Wagner F, Erdösová B, Kylarová D (December 2004). "Degradation phase of apoptosis during the early stages of human metanephros development". Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 148 (2): 255–6. doi:10.5507/bp.2004.054. PMID 15744391.
- Robinson, H. P.; Fleming, J. E. E. (September 1975). "A critical evaluation of sonar 'crown‐rump length' measurements". BJOG: An International Journal of Obstetrics and Gynaecology. 82 (9): 702–710. doi:10.1111/j.1471-0528.1975.tb00710.x. PMID 1182090. S2CID 31663686.
- Geirsson, R. T. (1 May 1991). "Ultrasound instead of last menstrual period as the basis of gestational age assignment". Ultrasound in Obstetrics and Gynecology. 1 (3): 212–219. doi:10.1046/j.1469-0705.1991.01030212.x. PMID 12797075. S2CID 29063110.
- Derived from a standard deviation in this interval of 2.6, as given in: Fehring, Richard J.; Schneider, Mary; Raviele, Kathleen (May 2006). "Variability in the Phases of the Menstrual Cycle". Journal of Obstetric, Gynecologic & Neonatal Nursing. 35 (3): 376–384. doi:10.1111/j.1552-6909.2006.00051.x. PMID 16700687.
- Jukic, A.M.; Baird, D.D.; Weinberg, C.R.; McConnaughey, D.R.; Wilcox, A.J. (October 2013). "Length of human pregnancy and contributors to its natural variation". Human Reproduction. 28 (10): 2848–2855. doi:10.1093/humrep/det297. PMC 3777570. PMID 23922246.
- Jobe, Alan H (2004). "Post-conceptional age and IVH in ECMO patients". The Journal of Pediatrics. 145 (2): A2. doi:10.1016/j.jpeds.2004.07.010.
- GOULD, MEREDITH (2012). Biology of Fertilization V3: The Fertilization Response of the Egg.
- "Diseases That Cause Infertility". Center of Reproductive Medicine. Retrieved 6 March 2021.