Follicular phase
The follicular phase, also known as the preovulatory phase or proliferative phase,[1] is the phase of the estrous cycle (or, in primates[2] for example, the menstrual cycle) during which follicles in the ovary mature from primary follicle to a fully mature graafian follicle. It ends with ovulation. The main hormones controlling this stage are secretion of gonadotropin-releasing hormones, which are follicle-stimulating hormones and luteinising hormones. They are released by pulsatile secretion.[1] The duration of the follicular phase can differ depending on the length of the menstrual cycle, while the luteal phase is usually stable, does not really change and lasts 14 days.
| Follicular phase | |
|---|---|
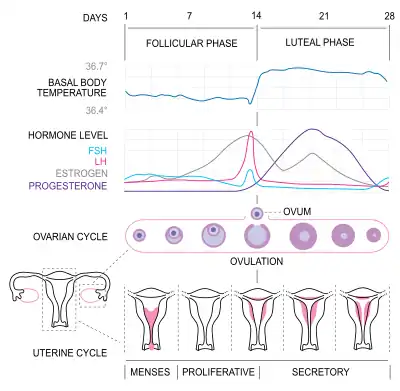 Figure 1. Menstrual cycle illustrating hormone levels, follicle development and uterine cycle | |
| Biological system | Urogenital system(reproductive) |
Hormonal events
Protein secretion
Due to the increase of FSH, the protein inhibin B will be secreted by the granulosa cells. Inhibin B will eventually blunt the secretion of FSH toward the end of the follicular phase. Inhibin B levels will be highest during the LH surge before ovulation and will quickly decrease after.[1]
Follicle recruitment

Follicle-stimulating hormone (FSH) is secreted by the anterior pituitary gland (Figure 2). FSH secretion begins to rise in the last few days of the previous menstrual cycle,[3] and is the highest and most important during the first week of the follicular phase[4] (Figure 1). The rise in FSH levels recruits five to seven tertiary-stage ovarian follicles (this stage follicle is also known as a Graafian follicle or antral follicle) for entry into the menstrual cycle. These follicles, that have been growing for the better part of a year in a process known as folliculogenesis, compete with each other for dominance.[5]
FSH induces the proliferation of granulosa cells in the developing follicles, and the expression of luteinizing hormone (LH) receptors on these granulosa cells (Figure 1). Under the influence of FSH, aromatase and p450 enzymes are activated, causing the granulosa cells to begin to secrete estrogen. This increased level of estrogen stimulates production of gonadotropin-releasing hormone (GnRH), which increases production of LH.[4] LH induces androgen synthesis by thecal cells, stimulates proliferation, differentiation, and secretion of follicular thecal cells and increases LH receptor expression on granulosa cells.[4]
Throughout the entire follicular phase, rising estrogen levels in the blood stimulates growth of the endometrium and myometrium of the uterus.[6] It also causes endometrial cells to produce receptors for progesterone,[6] which helps prime the endometrium to respond to rising levels of progesterone during the late proliferative phase and throughout the luteal phase.
Estrogen surge
Two or three days before LH levels begin to increase,[7] usually by day seven of the cycle,[8] one (or occasionally two) of the recruited follicles has emerged as dominant. Many endocrinologists believe that the estrogen secretion of the dominant follicle has increased to a level that GnRH production is suppressed, which lowers the levels of LH and FSH. This slowdown in LH and FSH production leads to the atresia (death) of most of the recruited follicles, though the dominant follicle continues to mature. Estrogen levels will continue to increase for several days (on average, six days, but this varies widely).[7]
These high estrogen levels initiate the formation of a new layer of endometrium in the uterus, histologically identified as the proliferative endometrium. Crypts in the cervix are also stimulated to produce fertile cervical mucus.[7] This mucus reduces the acidity of the vagina, creating a more hospitable environment for sperm.[9] It also has a characteristic texture that helps guide sperm through the cervix[10] and to the fallopian tubes, where they wait for ovulation. In addition, basal body temperature may lower slightly under the influence of high estrogen levels.[11]
LH surge and ovulation
Estrogen levels are highest right before the LH surge begins (Figure 1). The short-term drop in steroid hormones between the beginning of the LH surge and the event of ovulation may cause mid-cycle spotting or bleeding.[12] Under the influence of the preovulatory LH surge, the first meiotic division of the oocytes is completed. The surge also initiates luteinization of thecal and granulosa cells.[4] Ovulation normally occurs 30 (± 2) hours after the beginning of the LH surge (when LH is first detectable in urine).[13]
Follicular waves
Follicular waves are best described as the phase when follicles have matured sufficiently and rupture, leading to ovulation. Recent findings into the menstrual cycle in mammals has discovered that 2 or more follicles can develop but only one of the follicles fully matures to release the egg.[14][15] This follicular wave involves multiple surges in the levels of FSH to initiate follicular development. A study has found that 68% of women tended to display two follicular wave developments before ovulation while the remaining had three waves.[16]
References
- Carol N. Monis; Maggie Tetrokalashvili. (2019). "Menstrual Cycle Proliferative And Follicular Phase". Treasure Island (FL): StatPearls Publishing. PMID 31194386.
{{cite journal}}: CS1 maint: uses authors parameter (link) This article incorporates text available under the CC BY 4.0 license.
This article incorporates text available under the CC BY 4.0 license. - "Primate | Definition, Biology, & Facts | Britannica".
- Reed, Beverly G.; Carr, Bruce R. (2000). "The Normal Menstrual Cycle and the Control of Ovulation". In De Groot, Leslie J.; Chrousos, George; Dungan, Kathleen; Feingold, Kenneth R.; Grossman, Ashley; Hershman, Jerome M.; Koch, Christian; Korbonits, Márta; McLachlan, Robert (eds.). Endotext. South Dartmouth (MA): MDText.com, Inc. PMID 25905282.
- Dee Unglaub Silverthorn (2004). Human physiology: an integrated approach (Third ed.). San Francisco: Pearson/Benjamin Cummings. Chapter 26: Reproduction and Development, and Chapter 23 Endocrine control of growth and metabolism. ISBN 0-13-102015-3.
- McGee, E.A., & Hsueh, A.J. (2000). Initial and cyclic recruitment of ovarian follicles. Endocrine Reviews, 200-214, 21(2). doi: 10.1210/edrv.21.2.0394
- Strang, Eric P. Widmaier, Hershel Raff, Kevin T. (2006). Vander's human physiology the mechanisms of body function (10th ed.). Boston: McGraw-Hill. p. 678. ISBN 0-07-111677-X.
- Weschler, Toni (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. pp. 359–361. ISBN 0-06-093764-5.
- Stenchever Droegemuller Herbst Mishell (2001). Comprehensive Gynecology (Fourth ed.). St. Louise, Missouri: Mosby. p. 87. ISBN 0-323-01402-X.
- Weschler (2002), p.57
- Weschler (2002), illustrations p.59 and p.3 of color insert
- Weschler (2002), pp.54,306,310
- Weschler (2002), p.65
- Susan B. Bullivant; Sarah A. Sellergren; Kathleen Stern; et al. (February 2004). "Women's sexual experience during the menstrual cycle: identification of the sexual phase by noninvasive measurement of luteinizing hormone". Journal of Sex Research. 41 (1): 82–93. doi:10.1080/00224490409552216. PMID 15216427. S2CID 40401379.
- Evans, A. C.; Duffy, P.; Hynes, N.; Boland, M. P. (February 2000). "Waves of follicle development during the estrous cycle in sheep". Theriogenology. 53 (3): 699–715. doi:10.1016/S0093-691X(99)00268-X. ISSN 0093-691X. PMID 10735037.
- Boer, H. M. T.; Röblitz, S.; Stötzel, C.; Veerkamp, R. F.; Kemp, B.; Woelders, H. (December 2011). "Mechanisms regulating follicle wave patterns in the bovine estrous cycle investigated with a mathematical model". Journal of Dairy Science. 94 (12): 5987–6000. doi:10.3168/jds.2011-4400. ISSN 1525-3198. PMID 22118087.
- Baerwald, Angela R.; Adams, Gregg P.; Pierson, Roger A. (2003-09-01). "Characterization of Ovarian Follicular Wave Dynamics in Women1". Biology of Reproduction. 69 (3): 1023–1031. doi:10.1095/biolreprod.103.017772. ISSN 0006-3363. PMID 12748128.