Myoglobinuria
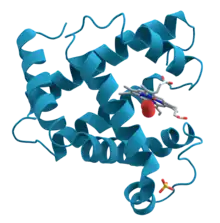
Myoglobinuria is the presence of myoglobin in the urine, which usually results from rhabdomyolysis or muscle injury.[1] Myoglobin is present in muscle cells as a reserve of oxygen.
| Myoglobinuria | |
|---|---|
 | |
| Urine from a person with rhabdomyolysis showing the characteristic brown discoloration as a result of myoglobinuria | |
| Specialty | Nephrology |
Signs and symptoms
Signs and symptoms of myoglobinuria are usually nonspecific and needs some clinical prudence. Therefore, among the possible signs and symptoms to look for would be:[2]
- Swollen and painful muscles
- Fever, nausea
- Delirium (elderly individuals)
- Myalgia
- Dark urine
- Calcium ion loss
Causes
Trauma, vascular problems, malignant hyperthermia, certain drugs and other situations can destroy or damage the muscle, releasing myoglobin to the circulation and thus to the kidneys. Under ideal situations myoglobin will be filtered and excreted with the urine, but if too much myoglobin is released into the circulation or in case of kidney problems, it can occlude the kidneys' filtration system leading to acute tubular necrosis and acute kidney injury.
Other causes of myoglobinuria include:
- McArdle's disease
- Phosphofructokinase deficiency[3]
- Carnitine palmitoyltransferase II deficiency
- Malignant hyperthermia
- Polymyositis
- Lactate dehydrogenase deficiency
- Adenosine monophosphate deaminase deficiency type 1
- Thermal or electrical burn
Pathophysiology
Myoglobinuria pathophysiology consists of a series of metabolic actions in which damage to muscle cells affect calcium mechanisms, thereby increasing free ionized calcium in the cytoplasm of the myocytes (concurrently decreasing free ionized calcium in the bloodstream). This, in turn, affects several intracellular enzymes that are calcium-dependent, thereby compromising the cell membrane, which in turn causes the release of myoglobin.[4][5]
Diagnosis
After centrifuging, the urine of myoglobinuria is red, where the urine of hemoglobinuria after centrifuge is pink to clear.
Treatment
Hospitalization and IV hydration should be the first step in any patient suspected of having myoglobinuria or rhabdomyolysis. The goal is to induce a brisk diuresis to prevent myoglobin precipitation and deposition, which can cause acute kidney injury. Mannitol can be added to assist with diuresis. Adding sodium bicarbonate to the IV fluids will cause alkalinization of the urine, believed to reduce the breakdown of myoglobin into its nephrotoxic metabolites, thus preventing renal damage. Often, IV normal saline is all that is needed to induce diuresis and alkalinize the urine.
See also
- Pigmenturia
References
- Prasad Devarajan, MD, FAAP (2020-02-19). "Myoglobinuria: Background, Pathophysiology, Etiology". Medscape Reference. Retrieved 2020-07-13.
Myoglobinuria is usually the result of rhabdomyolysis or muscle destruction. When excreted into the urine, myoglobin, a monomer containing a heme molecule similar to hemoglobin, can precipitate, causing tubular obstruction and acute kidney injury.
{{cite web}}: CS1 maint: multiple names: authors list (link) - "Rhabdomyolysis and Other Causes of Myoglobinuria". Patient. EMIS Group. Retrieved 10 September 2015.
- Toscano A, Musumeci O (October 2007). "Tarui disease and distal glycogenoses: clinical and genetic update". Acta Myol. 26 (2): 105–7. PMC 2949577. PMID 18421897.
- "Myoglobinuria". eMedicine. Medscare. Retrieved 10 September 2015.
- Giannoglou, George D.; Chatzizisis, Yiannis S.; Misirli, Gesthimani (2007). "The syndrome of rhabdomyolysis: Pathophysiology and diagnosis". European Journal of Internal Medicine. Elsevier BV. 18 (2): 90–100. doi:10.1016/j.ejim.2006.09.020. ISSN 0953-6205. PMID 17338959.
Further reading
- Pedley, edited by Lewis P. Rowland, Timothy A. (2010). Merritt's neurology (12th ed.). Philadelphia, PA: Lippincott Williams & Wilkins. p. 885. ISBN 978-0781791861. Retrieved 10 September 2015.
{{cite book}}:|first1=has generic name (help) - Nyhan, edited by Georg F. Hoffmann, Johannes Zschocke, William L. (2010). Inherited metabolic diseases : a clinical approach. Heidelberg: Springer. p. 165. ISBN 978-3-540-74722-2. Retrieved 10 September 2015.
{{cite book}}:|first1=has generic name (help)
External links
- Overview on the Neuromuscular disease center website.