RTS,S
RTS,S/AS01 (trade name Mosquirix) is a recombinant protein-based malaria vaccine. In October 2021, the vaccine was endorsed by the World Health Organization (WHO) for "broad use" in children, making it the first malaria vaccine candidate, and first vaccine to address parasitic infection, to receive this recommendation.[3][4][5]
| Vaccine description | |
|---|---|
| Target | P. falciparum; to a lesser extent Hepatitis B |
| Vaccine type | Protein subunit |
| Clinical data | |
| Trade names | Mosquirix |
| Routes of administration | intramuscular injection (0.5 mL)[1] |
| Legal status | |
| Legal status |
|

The RTS,S vaccine was conceived of and created in the late 1980s by scientists working at SmithKline Beecham Biologicals (now GlaxoSmithKline (GSK) Vaccines) laboratories in Belgium.[6] The vaccine was further developed through a collaboration between GSK and the Walter Reed Army Institute of Research in the U.S. state of Maryland[7] and has been funded in part by the PATH Malaria Vaccine Initiative and the Bill and Melinda Gates Foundation. Its efficacy ranges from 26 to 50% in infants and young children.
In July 2015, the vaccine received a positive scientific opinion by the European Medicines Agency (EMA) for use outside the European Union ,[1] it is the world's first licensed malaria vaccine and also the first vaccine licensed for use against a human parasitic disease of any kind.[8] On 23 October 2015, WHO's Strategic Advisory Group of Experts on Immunization (SAGE) and the Malaria Policy Advisory Committee (MPAC) jointly recommended a pilot implementation of the vaccine in Africa.[9] This pilot project for vaccination was launched on 23 April 2019 in Malawi, on 30 April 2019 in Ghana, and on 13 September 2019 in Kenya.[10][11]
Background
Potential malaria vaccines have been an intense area of research since the 1960s.[12] SPf66 was tested extensively in endemic areas in the 1990s, but clinical trials showed it to be insufficiently effective.[13] Other vaccine candidates, targeting the blood-stage of the malaria parasite's life cycle, have also been insufficient on their own.[14] Among several potential vaccines under development that target the pre-erythrocytic stage of the disease, RTS,S has shown the most promising results so far.[15]
Approval history
RTS,S vaccine received a positive scientific opinion in July 2015, with a recommendation that it be used in Africa for babies at risk of getting malaria. RTS,S was the world's first malaria vaccine to get "approval" for this use.[16][8] Preliminary research suggests that delayed fractional dosing could increase the vaccine's efficacy up to 86%.[17][18]
On 17 November 2016, WHO announced that the RTS,S vaccine would be rolled out in pilot projects in three countries in sub-Saharan Africa. The pilot program, coordinated by WHO, will assess the extent to which the vaccine's protective effect shown in advanced clinical trials can be replicated in real-life settings. Specifically, the programme will evaluate the feasibility of delivering the required four doses of the vaccine; the impact of the vaccine on lives saved; and the safety of the vaccine in the context of routine use.[19]
Vaccinations by the ministries of health of Malawi, Ghana, and Kenya began in April and September 2019 and target 360,000 children per year in areas where vaccination would have the highest impact. The results are planned to be used by the World Health Organization to advise about a possible future deployment of the vaccine.[10][11][20] In 2021 it was reported that the vaccine together with other anti-malaria medication when given at the most vulnerable season could reduce deaths and illness from the disease by 70%.[21][22]
Funding
RTS,S has been funded, most recently, by the non-profit PATH Malaria Vaccine Initiative (MVI) and GlaxoSmithKline with funding from the Bill and Melinda Gates Foundation.[23] The RTS,S-based vaccine formulation had previously been demonstrated to be safe, well tolerated, immunogenic, and to potentially confer partial efficacy in both malaria-naive and malaria-experienced adults as well as children.[24]
Components and mechanism
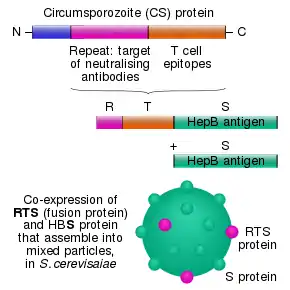
The RTS,S vaccine is based on a protein construct first developed by GlaxoSmithKline in 1986. It was named RTS because it was engineered using genes from the repeat ('R') and T-cell epitope ('T') of the pre-erythrocytic circumsporozoite protein (CSP) of the Plasmodium falciparum malaria parasite together with a viral surface antigen ('S') of the hepatitis B virus (HBsAg).[7] This protein was then mixed with additional HBsAg to improve purification, hence the extra "S".[7] Together, these two protein components assemble into soluble virus-like particles similar to the outer shell of a hepatitis B virus.[25]
A chemical adjuvant (AS01, specifically AS01E) was added to increase the immune system response.[26] Infection is prevented by inducing humoral and cellular immunity, with high antibody titers, that block the parasite from infecting the liver.[27]
The T-cell epitope of CSP is O-fucosylated in Plasmodium falciparum[28][29] and Plasmodium vivax,[30] while the RTS,S vaccine produced in yeast is not.[31]
References
- "Mosquirix H-W-2300". European Medicines Agency (EMA). Retrieved 4 March 2021.
- "RTS,S Malaria Vaccine: 2019 Partnership Award Honoree". YouTube. Global Health Technologies Coalition. Retrieved 6 October 2021.
- Davies L (6 October 2021). "WHO endorses use of world's first malaria vaccine in Africa". The Guardian. Retrieved 6 October 2021.
- Drysdale C, Kelleher K. "WHO recommends groundbreaking malaria vaccine for children at risk" (Press release). Geneva: World Health Organization. Retrieved 6 October 2021.
- Mandavilli A (6 October 2021). "A 'Historical Event': First Malaria Vaccine Approved by W.H.O." New York Times. Retrieved 6 October 2021.
- "HYBRID PROTEIN BETWEEN CS FROM PLASMODIUM AND HBsAG".
- Heppner DG, Kester KE, Ockenhouse CF, Tornieporth N, Ofori O, Lyon JA, et al. (March 2005). "Towards an RTS,S-based, multi-stage, multi-antigen vaccine against falciparum malaria: progress at the Walter Reed Army Institute of Research". Vaccine. 23 (17–18): 2243–50. doi:10.1016/j.vaccine.2005.01.142. PMID 15755604. S2CID 22824901. Archived from the original on 23 July 2018.
- Walsh F (24 July 2015). "Malaria vaccine gets 'green light'". BBC News. Archived from the original on 21 July 2020. Retrieved 25 July 2015.
- Stewart S (23 October 2015). "Pilot implementation of first malaria vaccine recommended by WHO advisory groups" (Press release). Geneva: World Health Organization. Archived from the original on 19 September 2021.
- Alonso P (19 June 2019). "Letter to partners – June 2019" (Press release). Wuxi: World Health Organization. Retrieved 22 October 2019.
- "Malaria vaccine launched in Kenya: Kenya joins Ghana and Malawi to roll out landmark vaccine in pilot introduction" (Press release). Homa Bay: World Health Organization. 13 September 2019. Retrieved 22 October 2019.
- Hill AV (October 2011). "Vaccines against malaria". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 366 (1579): 2806–14. doi:10.1098/rstb.2011.0091. PMC 3146776. PMID 21893544.
- Graves P, Gelband H (April 2006). Graves PM (ed.). "Vaccines for preventing malaria (SPf66)". The Cochrane Database of Systematic Reviews (2): CD005966. doi:10.1002/14651858.CD005966. PMC 6532709. PMID 16625647.
- Graves P, Gelband H (October 2006). Graves PM (ed.). "Vaccines for preventing malaria (blood-stage)". The Cochrane Database of Systematic Reviews (4): CD006199. doi:10.1002/14651858.CD006199. PMC 6532641. PMID 17054281.
- Graves P, Gelband H (October 2006). Graves PM (ed.). "Vaccines for preventing malaria (pre-erythrocytic)". The Cochrane Database of Systematic Reviews (4): CD006198. doi:10.1002/14651858.CD006198. PMC 6532586. PMID 17054280.
- "First malaria vaccine receives positive scientific opinion from EMA". European Medicines Agency. 24 July 2015. Retrieved 24 July 2015.
- Birkett A (16 September 2016). "A vaccine for malaria elimination?". PATH. Archived from the original on 15 July 2017. Retrieved 7 November 2016.
- Regules JA, Cicatelli SB, Bennett JW, Paolino KM, Twomey PS, Moon JE, et al. (September 2016). "Fractional Third and Fourth Dose of RTS,S/AS01 Malaria Candidate Vaccine: A Phase 2a Controlled Human Malaria Parasite Infection and Immunogenicity Study". The Journal of Infectious Diseases. 214 (5): 762–71. doi:10.1093/infdis/jiw237. PMID 27296848.
- "Malaria: The malaria vaccine implementation programme (MVIP)".
- "WHO | MVIP countries: Ghana, Kenya and Malawi". Archived from the original on 22 April 2019.
- Chandramohan D, Zongo I, Sagara I, Cairns M, Yerbanga RS, Diarra M, et al. (September 2021). "Seasonal Malaria Vaccination with or without Seasonal Malaria Chemoprevention". The New England Journal of Medicine. 385 (11): 1005–1017. doi:10.1056/NEJMoa2026330. PMID 34432975.
- Roxby P (26 August 2021). "Trial suggests malaria sickness could be cut by 70%". BBC News. Archived from the original on 3 October 2021. Retrieved 26 August 2021.
- Stein R (18 October 2011). "Experimental malaria vaccine protects many children, study shows". Washington Post.
- Regules JA, Cummings JF, Ockenhouse CF (May 2011). "The RTS,S vaccine candidate for malaria". Expert Review of Vaccines. 10 (5): 589–99. doi:10.1586/erv.11.57. PMID 21604980. S2CID 20443829.
- Rutgers T, Gordon D, Gathoye AM, Hollingdale M, Hockmeyer W, Rosenberg M, De Wilde M (September 1988). "Hepatitis B Surface Antigen as Carrier Matrix for the Repetitive Epitope of the Circumsporozoite Protein of Plasmodium Falciparum". Nature Biotechnology. 6 (9): 1065–1070. doi:10.1038/nbt0988-1065. S2CID 39880644.
- RTS,S Clinical Trials Partnership (July 2015). "Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial". Lancet. 386 (9988): 31–45. doi:10.1016/S0140-6736(15)60721-8. PMC 5626001. PMID 25913272.
- Foquet L, Hermsen CC, van Gemert GJ, Van Braeckel E, Weening KE, Sauerwein R, et al. (January 2014). "Vaccine-induced monoclonal antibodies targeting circumsporozoite protein prevent Plasmodium falciparum infection". The Journal of Clinical Investigation. 124 (1): 140–4. doi:10.1172/JCI70349. PMC 3871238. PMID 24292709.
- Swearingen KE, Lindner SE, Shi L, Shears MJ, Harupa A, Hopp CS, et al. (April 2016). "Interrogating the Plasmodium Sporozoite Surface: Identification of Surface-Exposed Proteins and Demonstration of Glycosylation on CSP and TRAP by Mass Spectrometry-Based Proteomics". PLOS Pathogens. 12 (4): e1005606. doi:10.1371/journal.ppat.1005606. PMC 4851412. PMID 27128092.
- Lopaticki S, Yang AS, John A, Scott NE, Lingford JP, O'Neill MT, et al. (September 2017). "Protein O-fucosylation in Plasmodium falciparum ensures efficient infection of mosquito and vertebrate hosts". Nature Communications. 8 (1): 561. Bibcode:2017NatCo...8..561L. doi:10.1038/s41467-017-00571-y. PMC 5601480. PMID 28916755.
- Swearingen KE, Lindner SE, Flannery EL, Vaughan AM, Morrison RD, Patrapuvich R, et al. (July 2017). "Proteogenomic analysis of the total and surface-exposed proteomes of Plasmodium vivax salivary gland sporozoites". PLOS Neglected Tropical Diseases. 11 (7): e0005791. doi:10.1371/journal.pntd.0005791. PMC 5552340. PMID 28759593.
- Goddard-Borger, Ethan D; Boddey, Justin A (1 May 2018). "Implications of Plasmodium glycosylation on vaccine efficacy and design". Future Microbiology. 13 (6): 609–612. doi:10.2217/fmb-2017-0284. ISSN 1746-0913.
Further reading
- Agnandji ST, Lell B, Fernandes JF, Abossolo BP, Methogo BG, Kabwende AL, et al. (December 2012). "A phase 3 trial of RTS,S/AS01 malaria vaccine in African infants". N Engl J Med. 367 (24): 2284–95. doi:10.1056/NEJMoa1208394. PMID 23136909.
- Asante KP, Abdulla S, Agnandji S, Lyimo J, Vekemans J, Soulanoudjingar S, et al. (October 2011). "Safety and efficacy of the RTS,S/AS01E candidate malaria vaccine given with expanded-programme-on-immunisation vaccines: 19 month follow-up of a randomised, open-label, phase 2 trial". The Lancet. Infectious Diseases. 11 (10): 741–9. doi:10.1016/S1473-3099(11)70100-1. PMID 21782519.
- Wilby KJ, Lau TT, Gilchrist SE, Ensom MH (March 2012). "Mosquirix (RTS,S): a novel vaccine for the prevention of Plasmodium falciparum malaria". The Annals of Pharmacotherapy. 46 (3): 384–93. doi:10.1345/aph.1AQ634. PMID 22408046. S2CID 32412123.