Leukoaraiosis
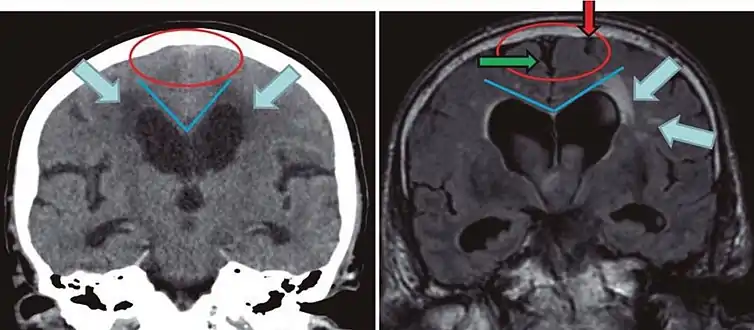
Leukoaraiosis is a particular abnormal change in appearance of white matter near the lateral ventricles. It is often seen in aged individuals, but sometimes in young adults.[1][2] On MRI, leukoaraiosis changes appear as white matter hyperintensities (WMHs) in T2 FLAIR images.[3][4] On CT scans, leukoaraiosis appears as hypodense periventricular white-matter lesions.[5]


.jpg.webp)
The term "leukoaraiosis" was coined in 1986[6][7] by Hachinski, Potter, and Merskey as a descriptive term for rarefaction ("araiosis") of the white matter, showing up as decreased density on CT and increased signal intensity on T2/FLAIR sequences (white matter hyperintensities) performed as part of MRI brain scans.
These white matter changes are also commonly referred to as periventricular white matter disease, or white matter hyperintensities (WMH), due to their bright white appearance on T2 MRI scans. Many patients can have leukoaraiosis without any associated clinical abnormality. However, underlying vascular mechanisms are suspected to be the cause of the imaging findings. Hypertension, smoking, diabetes,[3] hyperhomocysteinemia, and heart diseases are all risk factors for leukoaraiosis.
Leukoaraiosis has been reported to be an initial stage of Binswanger's disease but this evolution does not always happen.
Causes
White matter hyperintensities can be caused by a variety of factors, including ischemia, micro-hemorrhages, gliosis, damage to small blood vessel walls, breaches of the barrier between the cerebrospinal fluid and the brain, or loss and deformation of the myelin sheath.[8][9] Multiple small vessel infarcts in the subcortical white matter can cause the condition, often the result of chronic hypertension leading to lipohyalinosis of the small vessels. Patients may develop cognitive impairment and dementia.[10][11]
Special cases
- Ischaemic leukoaraiosis has been defined as the leukoaraiosis present after a stroke.[12]
- Diabetes-associated leukoaraiosis has been reported[13]
- CuRRL syndrome: increased Cup: Disc Ratio, Retinal GanglionCell Complex thinning, Radial Peripapillary Capillary Network Density Reduction and Leukoaraiosis[2]
- CADASIL is a hereditary cerebrovascular disorder associated with T2-hyperintense white matter lesions that have a greater extent and earlier age of onset than age-related leukoaraiosis.
References
- Putaala J., Kurkinen M., Tarvos V., Salonen O., Kaste M., Tatlisumak T. (2009). "Silent brain infarcts and leukoaraiosis in young adults with first-ever ischemic stroke". Neurology. 72 (21): 1823–1829. doi:10.1212/WNL.0b013e3181a711df. PMID 19470964. S2CID 593328.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Aik Kah, Tan (2018). "CuRRL Syndrome: A Case Series" (PDF). Acta Scientific Ophthalmology. 1 (3): 9–13.
- Habes M, Erus G, Toledo JB, Zhang T, Bryan N, Launer LJ, Rosseel Y, Janowitz D, Doshi J, Van der Auwera S, von Sarnowski B, Hegenscheid K, Hosten N, Homuth G, Völzke H, Schminke U, Hoffmann W, Grabe H, Davatzikos C (2016). "White matter hyperintensities and imaging patterns of brain ageing in the general population". Brain. 139 (Pt 4): 1164–79. doi:10.1093/brain/aww008. PMC 5006227. PMID 26912649.
- Yan, Shenqiang; Wan, Jinping; Zhang, Xuting; Tong, Lusha; Zhao, Song; Sun, Jianzhong; Lin, Yuehan; Shen, Chunhong; Lou, Min (2014). "Increased Visibility of Deep Medullary Veins in Leukoaraiosis: A 3-T MRI Study". Frontiers in Aging Neuroscience. 6: 144. doi:10.3389/fnagi.2014.00144. PMC 4074703. PMID 25071553.
- Kobari M, Meyer JS, Ichijo M, Oravez WT (1990). "Leukoaraiosis: correlation of MR and CT findings with blood flow, atrophy, and cognition". AJNR Am J Neuroradiol. 11 (2): 273–81. PMC 8334682. PMID 2107711.
- Hachinski, VC; Potter, P; Merskey, H (1986). "Leuko-araiosis: An ancient term for a new problem". The Canadian Journal of Neurological Sciences. 13 (4 Suppl): 533–34. doi:10.1017/S0317167100037264. PMID 3791068. S2CID 38151019.
- Hachinski, V. C.; Potter, P.; Merskey, H. (1987). "Leuko-Araiosis". Archives of Neurology. 44 (1): 21–23. doi:10.1001/archneur.1987.00520130013009. PMID 3800716.
- Raz N, Yang Y, Dahle CL, Land S (2012). "Volume of white matter hyperintensities in healthy adults: contribution of age, vascular risk factors, and inflammation-related genetic variants". Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease. 1822 (3): 361–69. doi:10.1016/j.bbadis.2011.08.007. PMC 3245802. PMID 21889590.
- Lin, Jing; Wang, Dilong; Lan, Linfang; Fan, Yuhua (2017). "Multiple Factors Involved in the Pathogenesis of White Matter Lesions". BioMed Research International. 2017: 9372050. doi:10.1155/2017/9372050. ISSN 2314-6141. PMC 5339523. PMID 28316994.
- Fauci, Anthony S.; Braunwald, Eugene; Weiner, Charles; Kasper, Dennis L.; Hauser, Stephen L.; Longo, Dan L.; Jameson, J. Larry; Loscalzo, Joseph (2008). Harrison's Principles of Internal Medicine (17th ed.). New York: McGraw-Hill. ISBN 978-0-07-149619-3.
- Hu, He-Ying; Ou, Ya-Nan; Shen, Xue-Ning; Qu, Yi; Ma, Ya-Hui; Wang, Zuo-Teng; Dong, Qiang; Tan, Lan; Yu, Jin-Tai (January 2021). "White matter hyperintensities and risks of cognitive impairment and dementia: A systematic review and meta-analysis of 36 prospective studies". Neuroscience and Biobehavioral Reviews. 120: 16–27. doi:10.1016/j.neubiorev.2020.11.007. ISSN 1873-7528. PMID 33188821. S2CID 226301188.
- O'Sullivan M, Morris RG, Huckstep B, Jones DK, Williams SCR, Markus HS (2004). "Diffusion tensor MRI correlates with executive dysfunction in patients with ischaemic leukoaraiosis". J Neurol Neurosurg Psychiatry. 75 (3): 441–47. doi:10.1136/jnnp.2003.014910. PMC 1738975. PMID 14966162.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Maldjian JA, Whitlow CT, Saha BN, Kota G, Vandergriff C, Davenport EM, Divers J, Freedman BI, Bowden DW. "Automated White Matter Total Lesion Volume Segmentation in Diabetes". AJNR Am J Neuroradiol. 2013 Jul 18
Further reading
- Pantoni, L.; Garcia, J. H. (1995). "The Significance of Cerebral White Matter Abnormalities 100 Years After Binswanger's Report : A Review". Stroke. 26 (7): 1293–301. doi:10.1161/01.STR.26.7.1293. PMID 7604429.
- Pantoni, L; Inzitari, D (1998). "New clinical relevance of leukoaraiosis. European Task Force on Age-Related White Matter-Changes" (PDF). Stroke. 29 (2): 543. doi:10.1161/01.str.29.2.543. PMID 9472903.
- Werder, SF (2010). "Cobalamin deficiency, hyperhomocysteinemia, and dementia". Neuropsychiatric Disease and Treatment. 6: 159–95. doi:10.2147/ndt.s6564. PMC 2874340. PMID 20505848.