Beta blocker toxicity
| Beta blocker toxicity | |
|---|---|
| Other names: Beta blocker poisoning, beta blocker overdose | |
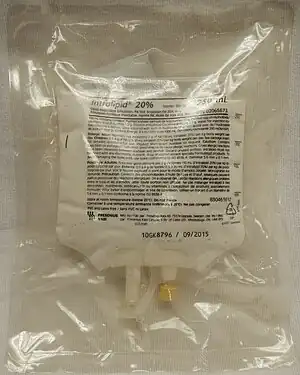 | |
| A 20% lipid emulsion may be used for beta blocker toxicity | |
| Specialty | Emergency medicine |
| Symptoms | Slow heart rate, low blood pressure[1] |
| Complications | Irregular heartbeat, low blood sugar[1] |
| Usual onset | Within 2 hours[2] |
| Causes | Too much beta blockers either by accident or on purpose[2] |
| Differential diagnosis | Calcium channel blocker toxicity, acute coronary syndrome, hyperkalemia[1] |
| Treatment | Activated charcoal, whole bowel irrigation, intravenous fluids, sodium bicarbonate, glucagon, high dose insulin, vasopressors, lipid emulsion, ECMO[1] |
| Prognosis | High risk of death[3] |
| Frequency | Relatively uncommon[1] |
Beta blocker toxicity is the taking of too much of the medications known as beta blockers, either by accident or on purpose.[2] This often causes a slow heart rate and low blood pressure.[1] Some beta blockers can also cause an irregular heartbeat or low blood sugar.[1] Symptoms usually occur in the first two hours but with some forms of the medication may not start until 20 hours.[2] A person may be medically cleared if they have no symptom 6 hours after taking an immediate release preparation.[4]
Beta blockers include metoprolol, bisoprolol, carvedilol, propranolol, and sotalol.[1] ECG changes may include PR prolongation and a wide QRS.[1] Measuring blood levels of beta blockers is not useful.[1] Other conditions that may present similarly include calcium channel blocker toxicity, acute coronary syndrome, and hyperkalemia.[1]
Treatment may include efforts to reduce absorption of the medication including: activated charcoal taken by mouth if given shortly after the ingestion or whole bowel irrigation if an extended release formula was taken.[1] Efforts to bring about vomiting are not recommended.[1] Medications to treat the toxic effects include: intravenous fluids, sodium bicarbonate, glucagon, high dose insulin, vasopressors and lipid emulsion.[1] Extracorporeal membrane oxygenation and electrical pacing may also be options.[1] Some beta blockers may be removable by dialysis.[1]
Beta blocker toxicity is relatively uncommon.[1] Along with calcium channel blockers and digoxin beta blockers have one of the highest rates of death in overdose.[3] These medications first became available in the 1960s and 1970s.[2][4]
Treatment
Vasopressors
The preferred vasopressor is generally epinephrine, though norepinephrine may be used in those who have a normal heart rate.[1] Dopamine is not generally recommended.[1] High doses may be required.[1]
Insulin
Insulin is often recommended at an initial dose of 0.5 to 1 unit per kilogram followed by an ongoing dose of 0.5 to 1 unit per kilogram per hour.[1] This may be increased up to 10 units per kilogram per hour.[1] This should be given together with dextrose, initially 25 grams and than followed by a dose of 0.5 grams per kilogram per hour.[1]
Dialysis
Beta blockers that may be removed by dialysis include sotalol, atenolol, timolol, acebutolol, and nadolol.[4]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 Palatnick, Wesley (September 2020). "Calcium-Channel Blocker, Beta Blocker, and Digoxin Toxicity Management Strategies". www.ebmedicine.net. Archived from the original on 14 May 2014. Retrieved 27 December 2020.
- 1 2 3 4 5 Khalid, MM; Galuska, MA; Hamilton, RJ (January 2020). "Beta-Blocker Toxicity". PMID 28846217.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 Marx, John A. Marx (2014). "Cardiovascular Drugs". Rosen's emergency medicine: concepts and clinical practice (8th ed.). Philadelphia, PA: Elsevier/Saunders. pp. Chapter 152. ISBN 1455706051.
- 1 2 3 Wall, Ron (2017). Rosen's Emergency Medicine: Concepts and Clinical Practice (9 ed.). Elsevier. p. 1881. ISBN 978-0323354790.