Brodie abscess
| Brodie abscess | |
|---|---|
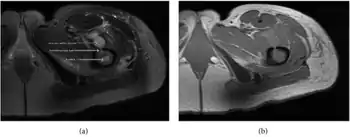 | |
| a,b) MRI showing the Brodie's abscess in the left proximal femur | |
A Brodie abscess is a subacute osteomyelitis, which may persist for years before progressing to a chronic, frank osteomyelitis. Classically, this may present after progression to a draining abscess extending from the tibia out through the skin. Occasionally acute osteomyelitis may be contained to a localized area and walled off by fibrous and granulation tissue.
The most frequent causative organism is Staphylococcus aureus.
Signs and symptoms
Localized pain, often nocturnal, alleviated by aspirin. Often mimics the symptoms of osteoid osteoma, which is typically less than 1 cm in diameter.
Location
Usually occurs at the metaphysis of long bones. Distal tibia, proximal tibia, distal femur, proximal or distal fibula, and distal radius.
Diagnosis
Radiographic features
Oval, elliptical, or serpentine radiolucency usually greater than 1 cm surrounded by a heavily reactive sclerosis, granulation tissue, and a nidus often less than 1 cm. The margins often appear scalloped on radiograph. Brodie's abscess is best visualized using computed tomography (CT) scan. Associated atrophy of soft tissue near the site of infection and shortening of the affected bone. Osteoblastoma may be a classic sign for Brodie's abscess.
 Periostial reaction along the medial cortex indicates an aggressive lesion. Neoplasm such as Ewing sarcoma and osteomyelitis could both have this plain radiographic appearance. Staphylococcus was recovered at surgery.
Periostial reaction along the medial cortex indicates an aggressive lesion. Neoplasm such as Ewing sarcoma and osteomyelitis could both have this plain radiographic appearance. Staphylococcus was recovered at surgery.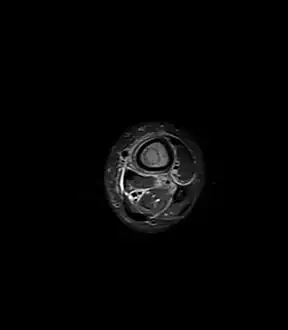 Fat saturated STIR (short tau inversion recovery) image showing hyperintense edema in the calf musculature, marrow edema, and subperiosteal pus. The intramedullary abscess cavity is hyperintense as well.
Fat saturated STIR (short tau inversion recovery) image showing hyperintense edema in the calf musculature, marrow edema, and subperiosteal pus. The intramedullary abscess cavity is hyperintense as well. Coronal fat suppressed STIR image showing, bone marrow and subcutaneous edema as well as subperiosteal edema. The thin hypointense rim surrounding the intramedullary collection represents the reactive interface between the abscess and the body's attempt to wall it off.
Coronal fat suppressed STIR image showing, bone marrow and subcutaneous edema as well as subperiosteal edema. The thin hypointense rim surrounding the intramedullary collection represents the reactive interface between the abscess and the body's attempt to wall it off. Axial T1-weighted MRI pre-contrast enhancement showing that the intramedullary collection is T1-hyperintense suggesting proteinaceous viscous fluid consistent with infection.
Axial T1-weighted MRI pre-contrast enhancement showing that the intramedullary collection is T1-hyperintense suggesting proteinaceous viscous fluid consistent with infection.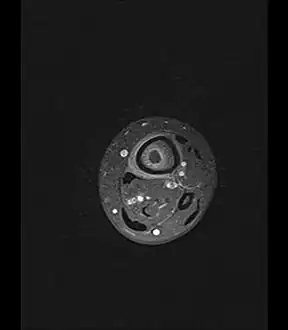 Axial T1-weighted fat-saturated MRI image following IV gadolinium contrast demonstrating the intramedullary lytic area seen on radiography to be ring enhancing consistent with a purulent fluid collection. Extensive circumferential periosteal enhancement is noted. There is also substantial bone marrow enhancement.
Axial T1-weighted fat-saturated MRI image following IV gadolinium contrast demonstrating the intramedullary lytic area seen on radiography to be ring enhancing consistent with a purulent fluid collection. Extensive circumferential periosteal enhancement is noted. There is also substantial bone marrow enhancement.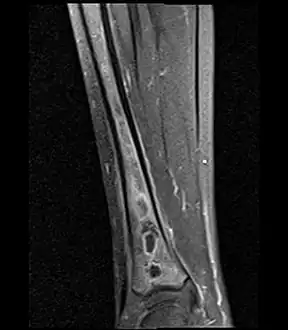 Sagittal T1-weighted fat-suppressed post gadolinium image showing the extent of the multiloculated intramedullary abscess.
Sagittal T1-weighted fat-suppressed post gadolinium image showing the extent of the multiloculated intramedullary abscess.
Treatment
In the majority of cases, surgery has to be performed. If the cavity is small then surgical evacuation and curettage is performed under antibiotic cover. If the cavity is large then the abscess space may need packing with cancellous bone chips after evacuation.
History
Brodie abscess is named after Sir Benjamin Collins Brodie, 1st Baronet. In the 1830s, he initially described a chronic inflammatory condition affecting the tibia without obvious acute etiology.[1] It was later discovered that this was caused by infection.
References
External links
| Classification | |
|---|---|
| External resources |