Infantile cortical hyperostosis
| Infantile cortical hyperostosis | |
|---|---|
| Other names: Caffey disease | |
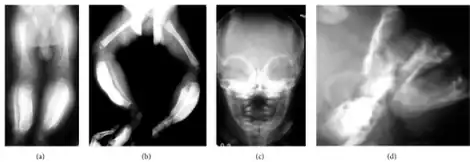 | |
| a,b) Massive cortical thickening/bowing both tibias are shown c,d) massive external cortical of mandible in frontal/lateral projection | |
Infantile cortical hyperostosis is a self-limited inflammatory disorder of infants that causes bone changes, soft tissue swelling and irritability. The disease may be present at birth or occur shortly thereafter. The cause is unknown. Both familial and sporadic forms occur. It is also known as Caffey disease or Caffey's disease.
Signs and symptoms
An affected infant typically has the following triad of signs and symptoms: soft-tissue swelling, bone lesions, and irritability. The swelling occurs suddenly, is deep, firm, and may be tender. Lesions are often asymmetric and may affect several parts of the body. Affected bones have included the mandible, tibia, ulna, clavicle, scapula, ribs, humerus, femur, fibula, skull, ilium, and metatarsals. When the mandible (lower jaw bone) is affected, infants may refuse to eat, leading to failure to thrive.
Genetics
It has been associated with COL1A1.[1]
Pathophysiology
In the early stages of infantile cortical hyperostosis, biopsy shows inflammation of the periosteum and adjacent soft tissues. After this resolves, the periosteum remains thickened, and subperiosteal immature lamellar bone can be seen on biopsy, while the bone marrow spaces contain vascular fibrous tissue. Eventually, the inflammation and subperiosteal changes resolve, and hyperplasia of lamellar cortical bone can be seen.
Radiographs initially show layers of periosteal new bone formation with cortical thickening. Periosteal new bone may cover the diaphysis of the bone, causing an increase in diameter of the bone. Over time, the periosteal new bone density increases, becoming homogenous with the underlying cortex. Eventually, the bone remodels and resumes a normal appearance.
Diagnosis

Most infants with infantile cortical hyperostosis are diagnosed by physical examination. X-rays can confirm the presence of bone changes and soft tissue swelling. Biopsy of the affected areas can confirm the presence of typical histopathological changes. No specific blood tests exist, but tests such as erythrocyte sedimentation rate (ESR) and alkaline phosphatase levels are often elevated. A complete blood count may show anemia (low red blood cell count) and leukocytosis (high white blood cell count). Other tests may be done to help exclude other diagnoses. Ultrasound imaging can help diagnose prenatal cases.
Differential diagnosis
Osteomyelitis (bone infection), which is much more common than infantile cortical hyperostosis, must be excluded, since it requires urgent treatment. Other diagnoses that can mimic this disorder and need to be excluded include physical trauma, child abuse, Vitamin A excess, hyperphosphatemia, prostaglandin E1 and E2 administration, scurvy, infections (including syphilis), Ewing sarcoma, and metastatic neuroblastoma.
Management
The treatment for this condition consists of NSAIDs, ibuprofen and naproxen, additionally sometimes corticosteroids are used[2]
Prognosis
Infantile cortical hyperostosis is a self-limited condition, meaning that the disease resolves on its own without treatment, usually within 6–9 months. Long-term deformities of the involved bones, including bony fusions and limb-length inequalities, are possible but rare.
Epidemiology
The disease has been reported to affect 3 per 1000 infants younger than 6 months in the United States. No predilection by race or sex has been established. Almost all cases occur by the age of 5 months. The familial form is inherited in an autosomal dominant fashion with variable penetrance. The familial form tends to have an earlier onset and is present at birth in 24% of cases, with an average age at onset of 6.8 weeks. The average age at onset for the sporadic form is 9–11 weeks.
Cortical hyperostosis is a potential side effect of long-term use of prostaglandins in neonates.[3]
History
Dr. John Caffey (1895–1978) first described infantile cortical hyperostosis in 1945. He described a group of infants with tender swelling in the soft tissues and cortical thickenings in the skeleton, with onset of these findings during the first 3 months of life. Dr. Caffey was regarded throughout the world as the father of pediatric radiology. His classic textbook, Pediatric X-Ray Diagnosis, which was first published in 1945, has become the recognized bible and authority in its field.[4]
References
- ↑ Kamoun-Goldrat A, Martinovic J, Saada J, et al. (July 2008). "Prenatal cortical hyperostosis with COL1A1 gene mutation". Am. J. Med. Genet. A. 146A (14): 1820–4. doi:10.1002/ajmg.a.32351. PMID 18553566. S2CID 205309510.
- ↑ Kirby, Kristen; Ponnarasu, Subitchan; Alsaleem, Mahdi; Wright, John E. (2022). "Infantile Cortical Hyperostosis". StatPearls. StatPearls Publishing. Archived from the original on 17 January 2022. Retrieved 17 January 2022.
- ↑ Lewis AB, Freed MD, Heymann MA, Roehl SL, Kensey RC (1981). "Side effects of therapy with prostaglandin E1 in infants with critical congenital heart disease". Circulation. 64 (5): 893–898. doi:10.1161/01.cir.64.5.893. PMID 7285304.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Caffey J (November 1946). "Infantile cortical hyperostoses". J. Pediatr. 29 (5): 541–59. doi:10.1016/S0022-3476(46)80122-7. PMID 21002859.
- Herring J (ed.). "Infantile Cortical Hyperostosis". Tachdjian's Pediatric Orthopaedics. Philadelphia PA: WB Saunders. pp. 1561–5.
External links
| Classification | |
|---|---|
| External resources |
|