Ciguatera fish poisoning
| Ciguatera fish poisoning | |
|---|---|
| Other names: Ciguatera, ciguatera food poisoning | |
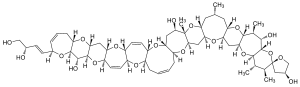 | |
| Chemical structure of ciguatoxin | |
| Symptoms | Diarrhea, vomiting, numbness, itchiness, sensitivity to hot and cold, dizziness, weakness[1][2] |
| Usual onset | 30 min to 2 days[3] |
| Duration | Few weeks to months[3] |
| Causes | Ciguatoxin and maitotoxin within certain reef fish[2] |
| Risk factors | Barracuda, grouper, moray eel, amberjack, sea bass, surgeon fish.[2] |
| Diagnostic method | Based on symptoms and recently eating fish[1] |
| Differential diagnosis | Paralytic shellfish poisoning, neurotoxic shellfish poisoning, scombroid food poisoning, pufferfish poisoning[1] |
| Treatment | Mannitol, gabapentin, amitriptyline[1][2] |
| Prognosis | Risk of death < 0.1%[2] |
| Frequency | ≈50,000 per year[2] |
Ciguatera fish poisoning (CFP), also known simply as ciguatera, is a foodborne illness caused by eating reef fish whose flesh is contaminated with certain toxins.[2] Symptoms may include diarrhea, vomiting, numbness, itchiness, sensitivity to hot and cold, dizziness, and weakness.[1][2] The onset varies with the amount of toxin eaten from half an hour to up to two days.[3] The diarrhea may last for up to four days.[1] Some symptoms may remain for a few weeks to months.[3] Heart difficulties such as slow heart rate and low blood pressure may also occur.[2]
The specific toxins involved are ciguatoxin and maitotoxin.[2] They are originally made by a small marine organism, Gambierdiscus toxicus, that grow on and around coral reefs in tropical and subtropical waters.[2] These are eaten by herbivorous fish which in turn are eaten by larger carnivorous fish.[2] The toxins become more concentrated as they move up the food chain.[3] The fish most often involved include barracuda, grouper, moray eel, amberjack, sea bass, and sturgeon.[2] Diagnosis is based on symptoms together with having recently eaten fish.[1] If a number of those who eat the same fish develop symptoms the diagnosis becomes more likely.[1] If some of the fish they had previously eaten is available this can be tested to confirm the diagnosis.[1]
Preventive efforts include not eating reef fish, not eating high-risk fish, and not eating fish liver, roe, or fish heads.[2] Ciguatoxin has no taste or smell, and cannot be destroyed by conventional cooking.[2] There is no specific treatment for poisoning once it occurs.[2] Mannitol may be considered, but the evidence supporting its use is not strong.[1] Gabapentin or amitriptyline may be used for some symptoms.[2]
Ciguatera fish poisoning affects around 50,000 people globally each year, per the Centers for Disease Control.[2] Other estimates suggest up to 500,000 cases per year.[1] It is the most frequent seafood poisoning.[3] It occurs most commonly in the Pacific Ocean, Indian Ocean, and the Caribbean Sea between the latitudes of 35°N and 35°S.[2] The risk of the condition appears to be increasing due to coral reef deterioration and increasing trade in seafood.[2] The risk of death from poisoning is less than 1 in 1,000.[2] Descriptions of the condition date back to at least 1511.[3] The current name came into use in 1787.[3]
Signs and symptoms
Hallmark symptoms of ciguatera in humans include gastrointestinal, cardiovascular, and neurological effects.[4][5] Gastrointestinal symptoms include nausea, vomiting, and diarrhea, usually followed by neurological symptoms such as headaches, muscle aches, paresthesia, numbness of extremities, mouth and lips, reversal of hot and cold sensation,[6][7] ataxia, vertigo, and hallucinations.[8][5] Severe cases of ciguatera can also result in cold allodynia, which is a burning sensation on contact with cold.[4] Neurological symptoms can persist and ciguatera poisoning is occasionally misdiagnosed as multiple sclerosis.[9] Cardiovascular symptoms include bradycardia, tachycardia, hypotension, hypertension, orthostatic tachycardia, exercise intolerance, and rhythm disorders.[10] Death from the condition can occur, but is very rare.[11]
Dyspareunia and other ciguatera symptoms have developed in otherwise healthy males and females following sexual intercourse with partners suffering ciguatera poisoning, signifying that the toxin may be sexually transmitted.[12] Diarrhea and facial rashes have been reported in breastfed infants of poisoned mothers, suggesting that ciguatera toxins migrate into breast milk.[13]
The symptoms can last from weeks to years, and in extreme cases as long as 20 years, often leading to long-term disability.[14] Most people do recover slowly over time.[15]
Cause
Gambierdiscus toxicus is the primary dinoflagellate responsible for the production of a number of similar polyether toxins, including ciguatoxin, maitotoxin, gambieric acid and scaritoxin, as well as the long-chain alcohol palytoxin.[16][17] Other dinoflagellates that may cause ciguatera include Prorocentrum spp., Ostreopsis spp., Coolia monotis, Thecadinium spp. and Amphidinium carterae.[18]
Diagnosis
Diagnosis is based on a person's symptoms together with having recently eaten fish.[1] If a number of those who eat the same fish have symptoms the diagnosis becomes more likely.[1] If some of the fish they had previously eaten is available this can also be tested to confirm the diagnosis.[1] Other potential causes such as paralytic shellfish poisoning (PSP), neurotoxic shellfish poisoning (NSP), scombrotoxin fish poisoning, and pufferfish poisoning should be excluded.[1]
The reversal of hot and cold sensations is an occasional symptom of CFP that may help differentiate it from intestinal "flu".[19]
Treatment
There is no effective treatment or antidote for ciguatera poisoning. The mainstay of treatment is supportive care. There is some evidence that calcium channel blockers like nifedipine and verapamil are effective in treating some of the symptoms that remain after the initial sickness passes, such as poor circulation and shooting pains through the chest. These symptoms are due to vasoconstriction caused by maitotoxin.[5][20][21][22] Ciguatoxin lowers the threshold for opening voltage-gated sodium channels in synapses of the nervous system. Opening a sodium channel causes depolarization, which could sequentially cause paralysis, heart contraction, and changing the senses of hot and cold. Some medications such as amitriptyline may reduce some symptoms, such as fatigue and paresthesia,[23] although benefit does not occur in every case.[24]
Mannitol
Mannitol was once used for poisoning after one study reported symptom reversal.[5][25] Follow-up studies in animals[26] and case reports in humans[27] also found benefit from mannitol. However, a randomized, double-blind clinical trial found no difference between mannitol and normal saline.[28] Despite this its use may still be considered.[1]
Epidemiology
The current estimated global incidence annually is 20,000 to 50,000 people, though a large number of cases are believed to go unreported.[29]
Due to the limited habitats of ciguatoxin-producing microorganisms, ciguatera is common only in subtropical and tropical waters, particularly the Pacific and Caribbean, and usually is associated with fish caught in tropical reef waters.[4] Exportation of reef fish, as well as tourism, often account for cases that develop in other regions.[29]
Ciguatoxin is found in over 400 species of reef fish. Avoiding consumption of all reef fish is the only sure way to avoid exposure.[30] Imported fish served in restaurants may contain the toxin and produce illness which often goes unexplained by physicians unfamiliar with the symptoms of a tropical toxin.[30][31] Ciguatoxin can also occur in farm-raised salmon.[32] Furthermore, species substitution, labeling a reef fish as a non-reef fish at restaurants and retail, can complicate efforts by consumers to avoid ciguatera.
20th and 21st centuries
- In 1994, Nobel Prize winning novelist Saul Bellow nearly died from Ciguatera after eating red snapper on vacation in St. Martin, fictionalized in his last novel Ravelstein.[33]
- In 2007, ten people in St. Louis, Missouri developed the disease after eating imported fish.[34]
- In February 2008, the U.S. Food and Drug Administration (FDA) traced several outbreaks to the Flower Garden Banks National Marine Sanctuary in the northern Gulf of Mexico, near the Texas–Louisiana shoreline. The FDA advised seafood processors that ciguatera poisoning was reasonably likely to occur from eating several species of fish caught as far as 50 miles (80 km) from the sanctuary.[35]
- From August 2010 to July 2011, there were eight outbreaks of Ciguatera fish poisoning in New York City. Outbreaks were linked to barracuda and grouper purchased at a fish market in Queens, New York.[36]
- In the first quarter of 2012, two restaurants in Lanzarote, Canary Islands are thought to have been the source of ciguatera poisoning, leading to new fishing regulations issued 18 April 2012. The first outbreak was reported in February 2012. Diners suffered with vomiting, diarrhoea and abdominal pain several hours after eating amberjack. The second case was in early April affecting six people who live in Lanzarote and had all eaten amberjack at a local restaurant.[37]
- In March 2014, nine people were hospitalised near Macksville, New South Wales, Australia after a recreational fisherman caught a 55 lb Spanish Mackerel (Scomberomorus commerson) off Scott's Head (NSW) and then shared it among his friends and family.[38]
- In April 2015, fourteen crew members of a potash ship were hospitalized in Saint John, New Brunswick, Canada after consuming tropical fish obtained from international waters.[39] After the incident, Marine Catering Services issued a reminder to seafarers that the UK Food Act makes it illegal for crews to fish for food from their vessels.[40]
- In September 2016, a British holidaymaker died while on honeymoon in Mexico after consuming fish contaminated with the algae that causes ciguatera poisoning.[11] During October 2016, more than 100 people had ciguatera poisoning after eating fish heads supplied by an export firm in Mangalore, India.[41]
History
Ciguatera was first described by one of the surgeon's mates, William Anderson, on the crew of HMS Resolution in 1774.[42]
Researchers suggest that ciguatera outbreaks caused by warm climatic conditions in part propelled the migratory voyages of Polynesians between 1000 and 1400AD.[43][44]
Folk tales
In Northern Australia, where ciguatera is a common problem, two different folk science methods are widely believed to detect whether fish harbor significant ciguatoxin. The first method is that flies are supposed not to land on contaminated fish. The second is that cats will either refuse to eat or vomit/display symptoms after eating contaminated fish. A third, less common testing method involves putting a silver coin under the scales of the suspect fish. If the coin turns black, according to the theory, it is contaminated.
On Grand Cayman and other islands the locals will test barracuda by placing a piece of the fish on the ground and allowing ants to crawl on it. If the ants do not avoid the flesh and will eat it, then the fish is deemed safe.
In Dominican Republic, another common belief is that during months whose names do not include the letter "R" (May through August), it is not recommended to eat certain kinds of fish, because they are more likely to be infected by the ciguatera toxin.
The validity of many of these tests has been scientifically rejected.[45]
Folk remedies
Leaves of Heliotropium foertherianum (Boraginaceae) – also known as octopus bush – are used in many Pacific islands as a traditional medicine to treat ciguatera fish poisoning. Senescent octopus bush leaves contain rosmarinic acid and derivatives, which are known for their antiviral, antibacterial, antioxidant, and anti-inflammatory properties.[46] Rosmarinic acid may remove the ciguatoxins from their sites of action, as well as being an anti-inflammatory.
An account of ciguatera poisoning from a linguistics researcher living on Malakula island, Vanuatu, indicates the local treatment: "We had to go with what local people told us: avoid salt and any seafood. Eat sugary foods. And they gave us a tea made from the roots of ferns growing on tree trunks. I don't know if any of that helped, but after a few weeks, the symptoms faded away".[47]
Various Caribbean folk and ritualistic treatments originated in Cuba and nearby islands. The most common old-time remedy involves bed rest subsequent to a guanabana juice enema. In Puerto Rico, natives drink a tea made from mangrove buttons, purportedly high in B vitamins, to flush the toxic symptoms from the system. There has never been a funded study of these treatments. Other folk treatments range from directly porting and bleeding the gastrointestinal tract to "cleansing" the diseased with a dove during a Santería ritual.
See also
- Algal bloom
- Gambierdiscus toxicus
- Red tide
- Yessotoxin
Footnotes
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Friedman, MA; Fernandez, M; Backer, LC; Dickey, RW; Bernstein, J; Schrank, K; Kibler, S; Stephan, W; Gribble, MO; Bienfang, P; Bowen, RE; Degrasse, S; Flores Quintana, HA; Loeffler, CR; Weisman, R; Blythe, D; Berdalet, E; Ayyar, R; Clarkson-Townsend, D; Swajian, K; Benner, R; Brewer, T; Fleming, LE (14 March 2017). "An Updated Review of Ciguatera Fish Poisoning: Clinical, Epidemiological, Environmental, and Public Health Management". Marine Drugs. 15 (3): 72. doi:10.3390/md15030072. PMC 5367029. PMID 28335428.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 "Food Poisoning from Marine Toxins - Chapter 2 - 2018 Yellow Book". CDC. 2017. Archived from the original on 11 January 2019. Retrieved 1 June 2018.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 3 4 5 6 7 8 "Ciguatera Fish Poisoning (CFP)". Marine biotoxins. Food and Agriculture Organization. 2004. p. Chapter 7. ISBN 978-92-5-105129-0. Archived from the original on 2015-07-04. Retrieved 2015-07-19.
- 1 2 3 Isbister G, Kiernan M (2005). "Neurotoxic marine poisoning". The Lancet Neurology. 4 (4): 219–28. doi:10.1016/S1474-4422(05)70041-7. PMID 15778101.
- 1 2 3 4 Clark RF, Williams SR, Nordt SP, Manoguerra AS (1999). "A review of selected seafood poisonings". Undersea Hyperb Med. 26 (3): 175–84. PMID 10485519. Archived from the original on 2011-08-11. Retrieved 2008-08-12.
- ↑ Patel, Ryan; Brice, Nicola L.; Lewis, Richard J.; Dickenson, Anthony H. (December 2015). "Ionic mechanisms of spinal neuronal cold hypersensitivity in ciguatera". The European Journal of Neuroscience. 42 (11): 3004–3011. doi:10.1111/ejn.13098. ISSN 0953-816X. PMC 4744673. PMID 26454262.
- ↑ Vetter, Irina; Touska, Filip; Hess, Andreas; Hinsbey, Rachel; Sattler, Simon; Lampert, Angelika; Sergejeva, Marina; Sharov, Anastasia; Collins, Lindon S (2012-10-03). "Ciguatoxins activate specific cold pain pathways to elicit burning pain from cooling". The EMBO Journal. 31 (19): 3795–3808. doi:10.1038/emboj.2012.207. ISSN 0261-4189. PMC 3463840. PMID 22850668.
- ↑ Swift A, Swift T (1993). "Ciguatera". J. Toxicol. Clin. Toxicol. 31 (1): 1–29. doi:10.3109/15563659309000371. PMID 8433404.
- ↑ Ting J, Brown A (2001). "Ciguatera poisoning: a global issue with common management problems" (PDF). Eur. J. Emerg. Med. 8 (4): 295–300. doi:10.1097/00063110-200112000-00009. PMID 11785597. Archived (PDF) from the original on 2021-08-28. Retrieved 2019-02-05.
- ↑ Hokama, Y. (1988-01-01). "Ciguatera fish poisoning". Journal of Clinical Laboratory Analysis. 2 (1): 44–50. doi:10.1002/jcla.1860020110. ISSN 1098-2825.
- 1 2 "Newlywed bride dies 10 days after wedding from heart attack believed to have been caused by 'contaminated fish'". The Daily Telegraph. Telegraph Media Group. 13 October 2016. Archived from the original on 17 October 2016. Retrieved 14 October 2016.
- ↑ Lange W, Lipkin K, Yang G (1989). "Can ciguatera be a sexually transmitted disease?". J. Toxicol. Clin. Toxicol. 27 (3): 193–7. doi:10.3109/15563658909038583. PMID 2810444.
- ↑ Blythe D, de Sylva D (1990). "Mother's milk turns toxic following fish feast". JAMA. 264 (16): 2074. doi:10.1001/jama.264.16.2074b. PMID 2214071.
- ↑ Gillespie N, Lewis R, Pearn J, Bourke A, Holmes M, Bourke J, Shields W (1986). "Ciguatera in Australia. Occurrence, clinical features, pathophysiology and management". Med. J. Aust. 145 (11–12): 584–90. PMID 2432386.
- ↑ Pearn J (2001). "Neurology of ciguatera". J. Neurol. Neurosurg. Psychiatry. 70 (1): 4–8. doi:10.1136/jnnp.70.1.4. PMC 1763481. PMID 11118239.
- ↑ Faust, MA and Gulledge RA. Identifying Harmful Marine Dynoflagellates. Archived 2016-03-05 at the Wayback Machine Smithsonian Institution, Contributions from the United States National Herbarium. Volume 42:1-144. 2002.
- ↑ National Office for Harmful Algal Blooms, Ciguatera Fish Poisoning Archived 2018-06-18 at the Wayback Machine. Woods Hole Oceanographic Institution.
- ↑ National Office for Harmful Algal Blooms, Ciguatera Fish Poisoning: Causative organisms: Archived 2019-04-04 at the Wayback Machine. Woods Hole Oceanographic Institution.
- ↑ Lehane, Leigh; Lewis, Richard J (November 2000). "Ciguatera: recent advances but the risk remains". International Journal of Food Microbiology. 61 (2–3): 91–125. doi:10.1016/S0168-1605(00)00382-2. PMID 11078162.
- ↑ Attaway D, Zaborsky O (1993). Marine Biotechnology. p. 8.
- ↑ Fleming L. "Ciguatera Fish Poisoning". Woods Hole Oceanographic Institution. Archived from the original on 2018-06-18. Retrieved 2009-10-30.
- ↑ Schlossberg D (1999). Infections of leisure. p. 13. ISBN 978-3-540-94069-2.
- ↑ Davis R, Villar L (1986). "Symptomatic improvement with amitriptyline in ciguatera fish poisoning". N. Engl. J. Med. 315 (1): 65. doi:10.1056/NEJM198607033150115. PMID 3713788.
- ↑ Hampton M, Hampton A (1989). "Ciguatera fish poisoning". J. Am. Acad. Dermatol. 20 (3): 510–1. doi:10.1016/S0190-9622(89)80094-5. PMID 2918120.
- ↑ Palafox N, Jain L, Pinano A, Gulick T, Williams R, Schatz I (1988). "Successful treatment of ciguatera fish poisoning with intravenous mannitol". JAMA. 259 (18): 2740–2. doi:10.1001/jama.259.18.2740. PMID 3128666.
- ↑ Mattei C, Molgó J, Marquais M, Vernoux J, Benoit E (1999). "Hyperosmolar D-mannitol reverses the increased membrane excitability and the nodal swelling caused by Caribbean ciguatoxin-1 in single frog myelinated axons". Brain Res. 847 (1): 50–8. doi:10.1016/S0006-8993(99)02032-6. PMID 10564735.
- ↑ Williamson J (1990). "Ciguatera and mannitol: a successful treatment". Med. J. Aust. 153 (5): 306–7. PMID 2118229.
- ↑ Schnorf H, Taurarii M, Cundy T (2002). "Ciguatera fish poisoning: a double-blind randomized trial of mannitol therapy". Neurology. 58 (6): 873–80. doi:10.1212/WNL.58.6.873. PMID 11914401.
- 1 2 Marcus, Erin N., Ciguatera fish poisoning, archived from the original on 4 March 2016, retrieved 6 April 2015
- 1 2 Schep LJ, Slaughter RJ, Temple WA, Beasley DM (2010). "Ciguatera poisoning: an increasing occurrence in New Zealand". N. Z. Med. J. 123 (1308): 100–102. PMID 20173810.
- ↑ Geller R, Olson K, Senécal P (1991). "Ciguatera fish poisoning in San Francisco, California, caused by imported barracuda". West. J. Med. 155 (6): 639–642. PMC 1003121. PMID 1812639.
- ↑ DiNubile M, Hokama Y (1995). "The ciguatera poisoning syndrome from farm-raised salmon". Annals of Internal Medicine. 122 (2): 113–114. doi:10.7326/0003-4819-122-2-199501150-00006. PMID 7992985.
- ↑ Leader, Zachary, The Life of Saul Bellow: Love and Strife 1965-2005, p. 528.
- ↑ "Bizarre fish poisoning sparks alarm". NBC News. 2019-05-01. Archived from the original on 2018-02-20. Retrieved 2019-05-07.
- ↑ "FDA Advises Seafood Processors About Ciguatera Fish Poisoning in the Northern Gulf of Mexico Near the Flower Garden Banks National Marine Sanctuary" (Press release). U.S. Food and Drug Administration. 2008-02-05. Archived from the original on 2008-02-08. Retrieved 2008-02-07.
- ↑ Centers for Disease Control and Prevention (CDC) (2013). "Ciguatera fish poisoning - New York City, 2010-2011". MMWR. Morbidity and Mortality Weekly Report. 62 (4): 61–5. PMC 4604878. PMID 23364271. Archived from the original on 2017-07-04. Retrieved 2017-09-09.
- ↑ Cliffe-Jones, Mike Jules (April 17, 2012). "Isolated Cases of Ciguatera Poisoning in Lanzarote". Information Lanzarote. Information Lanzarote. Archived from the original on 5 March 2016. Retrieved 31 October 2015.
- ↑ "Ciguatera poisoning from Spanish Mackerel caught off Scotts Head". ABC News. 2014-03-04. Archived from the original on 2021-08-28. Retrieved 2017-10-16.
- ↑ "Balsa 85 ID'd as ship in Saint John whose crew was hit by food poisoning". CBC New Brunswick. CBC. CBC. 13 April 2015. Archived from the original on 24 September 2015. Retrieved 31 October 2015.
- ↑ "Seafarers told no fishing!". The Sea. No. 236. Mission to Seafarers Limited. Jul–Aug 2015.
- ↑ "Love your fish? Then know about seafood poisoning too". Times of India. 4 October 2016. Archived from the original on 23 October 2016. Retrieved 14 October 2016.
- ↑ Sanders, Lisa (April 5, 2010). "Fish Tale". The New York Times. Archived from the original on 2010-04-13. Retrieved 2010-04-10.
The illness was first described in 1774 by a surgeon's mate on the crew of Captain Cook's South Pacific exploration aboard HMS Resolution. The crewman, John Anderson, documented the symptoms described by several shipmates who had eaten a large fish caught in the tropical waters.
(The New York Times incorrectly gives William Anderson's first name as John.) - ↑ Rongo, Teina; Bush, Mark; Van Woesik, Robert (2009). "Did ciguatera prompt the late Holocene Polynesian voyages of discovery?". Journal of Biogeography. 36 (8): 1423–32. doi:10.1111/j.1365-2699.2009.02139.x.
- ↑ "Did fish poisoning drive Polynesian colonization of the Pacific?". news.mongabay.com. 7 July 2009. Archived from the original on 28 January 2015. Retrieved 1 June 2018.
- ↑ Park, D. L. (1994). "Evaluation of methods for assessing ciguatera toxins in fish". Reviews of Environmental Contamination and Toxicology. 136: 1–20. PMID 8029489.
- ↑ Rossi, Fanny; Jullian, Valérie; Pawlowiez, Ralph; Kumar-Roiné, Shilpa; Haddad, Mohamed; Darius, H. Taiana; Gaertner-Mazouni, Nabila; Chinain, Mireille; Laurent, Dominique (2012). "Protective effect of Heliotropium foertherianum (Boraginaceae) folk remedy and its active compound, rosmarinic acid, against a Pacific ciguatoxin". Journal of Ethnopharmacology. 143 (1): 33–40. doi:10.1016/j.jep.2012.05.045. PMID 22706150.
- ↑ Dimock, Laura (June 2010). "Rescue mission for fading tongue". New Zealand Education Review. Archived from the original on 2014-01-04. Retrieved 2014-01-04.
References
- Ciguatera fish poisoning CDC Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine Archived 2017-12-13 at the Wayback Machine
- Friedman, M. A.; Fernandez, M.; Backer, L. C.; Dickey, R. W.; Bernstein, J.; Schrank, K.; Kibler, S.; Stephan, W.; Gribble, M. O.; Bienfang, P.; Bowen, R. E.; Degrasse, S.; Flores Quintana, H. A.; Loeffler, C. R.; Weisman, R.; Blythe, D.; Berdalet, E.; Ayyar, R.; Clarkson-Townsend, D.; Swajian, K.; Benner, R.; Brewer, T.; Fleming, L. E. (2017). "An Updated Review of Ciguatera Fish Poisoning: Clinical, Epidemiological, Environmental, and Public Health Management". Marine Drugs. 15 (3): 72. doi:10.3390/md15030072. PMC 5367029. PMID 28335428.
