Cocoliztli epidemics
The cocoliztli epidemic, or the great pestilence,[1] is a term given to millions of deaths in the territory of New Spain in present-day Mexico in the 16th century attributed to one or more illnesses collectively called cocoliztli, a mysterious illness characterized by high fevers and bleeding. It ravaged the Mexican highlands in epidemic proportions. The disease became known as Cocoliztli by the native Aztecs, and had devastating effects on the area’s demography, particularly for the indigenous people.
Based on the death toll, this outbreak is often referred to as the worst disease epidemic in the history of Mexico.[2] Subsequent outbreaks continued to baffle both Spanish and native doctors, with little consensus among modern researchers on the pathogenesis. However, recent bacterial genomic studies have suggested that Salmonella, specifically a serotype of Salmonella enterica known as Paratyphi C, was at least partially responsible for this initial outbreak.[3] It might have also been an indigenous viral hemorrhagic fever, perhaps exacerbated by the worst droughts to affect that region in 500 years, as well as living conditions for indigenous peoples of Mexico in the wake of the Spanish conquest (c. 1519).[4]
Etymology
The word cocoliztli originated from the Nahuatl word for "pest",[4] or disease, illness, and plague.
History
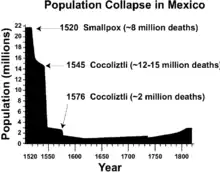
There have been 12 epidemics that have been identified as potentially being of cocoliztli, with the largest ones being those in 1520, 1545, 1576, 1736, and 1813.[6] Soto et al. have hypothesized that a large scale outbreak of hemorrhagic fever could also have contributed to the earlier collapse of the Classic Mayan civilization (AD 750–950), though most experts believe other factors including climate change likely played a much larger role.[7][8]
Cocoliztli epidemics usually occurred within two years of a major drought, while another disease called "matlazahuatl" appeared within two years of rainy periods. The epidemic in 1576 occurred after a drought stretching from Venezuela to Canada.[9][6] The correlation between drought and the disease has been thought to be that population numbers of the vesper mouse, a carrier of viral hemorrhagic fever, increased during the rains that followed the drought, as conditions improved.[5]
There exists some ambiguity regarding if cocoliztli preferentially targeted native people, as opposed to European colonists. The majority of firsthand accounts regarding the outbreak come from Aztec informants, who were primarily concerned with the diseases’ novelty and pronounced symptoms. Spanish colonizers may have used indigenous fears to further justify and enforce Christianity, as expressed by the following statement from Gonzalo de Ortiz (an encomendero): "envió Dios tal enfermedad sobre ellos que de quarto partes de indios que avia se llevó las tres" (God sent down such sickness upon the Indians that three out of every four of them perished).[10] It is unclear if Ortiz was exaggerating, or if the Spanish colonizers were truly less affected by this "act of God". Accounts by Toribio de Benavente Motolinia, an early Spanish missionary, seem to contradict Ortiz’s sentiment by suggesting that 60–90% of New Spain's total population decreased, regardless of ethnicity.[2] Bernardino de Sahagún, another Spanish clergyman and author of the Florentine Codex, attested to contracting the disease himself towards the end of the outbreak.[2] During a second cocoliztli outbreak in 1576, Sahagún identified both African slaves and Spanish colonists as being susceptible to the disease.
Sources and vectors
The social and physical environment of Colonial Mexico was likely key in allowing the Outbreak of 1545–1548 to reach the heights that it did. Already weakened by war and earlier disease outbreaks, the Aztecs were forced into easily governable reducciones (congregations) that focused on agricultural production and conversion to Christianity.[11] The reducciones would have not only brought people in much closer contact to one another, but with animals, as well. Whether it is rats, chickens, pigs, or cattle, animals imported from the Old World were potentially disease vectors for illnesses of New and Old World origins.
At the same time, droughts plagued Central America, with tree-ring data showing that the outbreak occurred in the midst of a megadrought.[4] The lack of water would have altered sanitary conditions and encouraged poor hygiene habits. Megadroughts were reported before both the 1545 and 1576 outbreaks. Additionally, periodic rains during a supposed megadrought, such as those hypothesized for shortly before 1545, would have increased the presence of New World rats and mice.[12] These animals are believed to have also been able to transport the arenaviruses capable of causing hemorrhagic fevers.[13] The effects of drought, combined with the now crowded settlements, is a highly plausible explanation for disease transmission, especially if the pathogens are spread by either human fecal matter or animals.
The Aztecs and other indigenous groups affected by the outbreak were potentially put at a disadvantage given their lack of exposure to zoonotic diseases. Given that many of the Old World pathogens being considered as responsible for the cocoliztli outbreak, it is significant that all but one of the most common species of domestic mammalian livestock (llamas/alpacas being the exception) come from the Old World.[14]
Extent
Scholars suspect it began in the southern and central Mexico Highlands, near modern-day Puebla City.[2] Shortly after its initial onset, however, it may have spread as far north as Sinaloa,[15] and as south as Chiapas and Guatemala, where it was called gucumatz.[10] It may have even crossed the South American border, and into Ecuador[16] and Peru,[17] although it is hard to be certain that the same disease was described. The outbreak seemed to be limited to higher elevation, as it was nearly absent from coastal regions at sea level, e.g. the plains along the Gulf of Mexico and Pacific coast.[4]
Symptoms
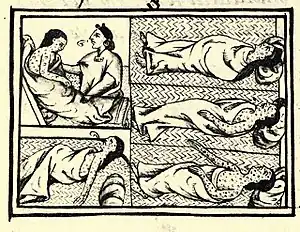
Although symptomatic descriptions of cocoliztli are similar to those of Old World diseases (e.g. measles, yellow fever, typhus), many researchers believe that it should be recognized as a separate disease.[3][12][18] According to Francisco Hernández de Toledo, a physician who witnessed the outbreak in 1576, symptoms included high fever, severe headache, vertigo, black tongue, dark urine, dysentery, severe abdominal and chest pain, head and neck nodules, neurologic disorders, jaundice, and profuse bleeding from the nose, eyes, and mouth; death frequently occurred within 3 to 4 days.[4] Some also describe the afflicted during this period as having spotted skin[19] and gastrointestinal hemorrhaging, leading to bloody diarrhea, as well as bleeding from the eyes, mouth, and vagina.[18] The onset was often rapid, and without any precursors that would suggest one was sick. The disease was characterized by an extremely high level of virulence, with death often occurring within a week of one becoming symptomatic.[20] Due to the virulence and effectiveness of the disease, recognizing its existence in the archaeological record has been difficult. Cocoliztli, and other diseases that work rapidly, usually do not leave impacts (lesions) on the decedent’s bones, despite causing significant damage to the gastrointestinal, respiratory, and other bodily systems.[21]
Causes
Numerous 16th century accounts detail the outbreak’s devastation, but the symptoms do not match any known pathogen. Shortly after 1548, the Spanish started calling the disease tabardillo (typhus), which had only been recognized in Spain since the late 15th century.[12] However, the symptoms of cocoliztli were still not identical to the typhus, or spotted fever, observed in the Old World at that time. Perhaps, this is why Francisco Hernández de Toledo, a Spanish physician, insisted on using the Nahuatl word when describing the disease to correspondents in the Old World.[12] Centuries later, in 1970, a historian named Germain Somolinos d'Ardois took a systematic look at all the proposed explanations at the time, including haemorrhagic influenza, leptospirosis, malaria, typhus, typhoid and yellow fever.[18] According to Somolinos d'Ardois, none of these quite matched the 16th century accounts of cocoliztli, leading him to conclude the disease was a result of "viral process of hemorrhagic influence." In other words, Somolinos d'Ardois believed cocoliztli was not the result of any known Old World pathogen, but possibly, a virus of either European or New World origins.
It has been speculated that it might have been an indigenous viral hemorrhagic fever as there are accounts of similar diseases having struck Mexico in Precolumbian times. The Codex Chimalpopoca states that an outbreak of bloody diarrhea occurred in Colhuacan in 1320.[22] If the disease was indigenous, it was perhaps exacerbated by the worst droughts to affect that region in 500 years and living conditions for indigenous peoples of Mexico in the wake of Spanish conquest (c. 1519).[4] Some historians have suggested it was typhus, measles, or smallpox, though the symptoms did not match.[23]
Marr and Kiracofe (2000) attempted to build off this work by reexamining Hernandez’s account of cocoliztli and comparing them with various clinical descriptions of other diseases.[12] They suggested that scholars consider "New World arenaviruses" and the role these pathogens may have played in colonial disease outbreaks. Rebelling against the universal acceptance of Post-Contact epidemics being "Old-World importations," Marr and Kiracofe theorized that arenaviruses, which mainly affect rodents,[13] were largely kept away from Pre-Columbian people. Consequently, rat and mice infestations brought upon by the arrival of the Spanish may, combined with climatic and landscape change, have brought these arenaviruses into much closer contact with people. Subsequent studies seemed to have accepted the viral haemorrhagic fever diagnosis, and became more interested in assessing how the disease became so widespread.[20]
In 2018, Johannes Krause, an evolutionary geneticist at the Max Planck Institute for the Science of Human History, and colleagues discovered new evidence for an Old World culprit. DNA samples from the teeth of 29 sixteenth-century skeletons in the Oaxaca region of Mexico were identified as belonging to a rare strain of the bacterium Salmonella enterica (subsp. enterica) which causes paratyphoid fever, suggesting that paratyphoid was the underlying fever behind the disease.[24][25]
The team extracted ancient DNA from the teeth of 29 individuals buried at Teposcolula-Yucundaa in Oaxaca, Mexico. The Contact-era site has the only cemetery to be conclusively linked to victims of the Cocoliztli Outbreak of 1545–1548. Using the MEGAN alignment tool (MALT), a program that attempts to match fragments of extracted DNA with a database of bacterial genomes, the researchers were able to recognize nonlocal microbial infections.
Within 10 individuals, they identified Salmonella enterica subsp. enterica serovar Paratyphi C, which causes enteric fevers in humans.[26] This strain of Salmonella is unique to humans, and was not found in any soil samples or pre-Contact individuals that were used as controls. Enteric fevers, also known as typhoid or paratyphoid, are similar to typhus, and were only distinguished from one another in the 19th century.[27] Today, S. Paratyphi C continues to cause enteric fevers, and if untreated, has a mortality rate up to 15%.[28] Infections are largely limited to developing nations in Africa and Asia, although enteric fevers, in general, are still a health threat world wide.[29] Infections with S. Paratyphi C are rare, as the majority of cases reported (about 27 million in 2000) were the result of the serovars S. Typhi and S. Paratyphi A.[3]
These findings are boosted by the recent discovery of S. Paratyphi C within a 13th century Norwegian cemetery.[30] A young female, who likely died from an enteric fever, is proof that the pathogen was present in Europe over 300 years before the epidemics in Mexico. Thus, it is possible that healthy carriers transported the bacteria to the New World, where it thrived. Those who unknowingly possessed the bacteria were likely aided from generations of contact with it, as it is believed that S. Paratyphi C may have first transferred over to humans from swine in the Old World during, or, shortly after the Neolithic period.[30]
Some, including evolutionary geneticist, María Ávila-Arcos, have questioned this evidence, since S. enterica symptoms are poorly matched with the disease.[31][32][28] Both Ávila-Arcos, and even Krause’s team and authors of earlier historical analyses,[33] point out that RNA viruses, among other non-bacterial pathogens, had not been investigated. Others have highlighted the fact that certain symptoms described, including gastrointestinal hemorrhaging, are not present in current observations of S. Paratyphi C infections.[34] Ultimately, a more definitive proposal for the cause of any of the cocoliztli epidemics of 1545–1548 and 1576-81 awaits further developments in ancient RNA analysis and the causes of different outbreaks may prove to differ.[35][36]
Effects
Death toll
Beyond the estimations done by Motolinia and others for New Spain, most of the death toll figures cited for the outbreak of 1545–1548 are concerned with Aztec populations. Around 800,000 died in the Valley of Mexico, which led to the widespread abandonment of many indigenous sites in the area during, or, shortly after this four-year period.[19] Estimates for the entire number of human lives lost during this epidemic have ranged from 5 to 15 million people,[37] making it one of the most deadly disease outbreaks of all time.[4]
Other
The effects of the outbreak extended beyond just a loss in terms of population. The lack of indigenous labor led to a sizeable food shortage, which affected both the natives and Spanish.[38] The death of many Aztecs due to the plague led to a void in land ownership, with Spanish colonists of all backgrounds looking to exploit these now vacant lands.[38] Coincidentally, the Spanish Emperor, Charles V, had been seeking a way to disempower the encomendero class, and establish a more efficient and "ethical" settlement system.[39]
Starting around the end of the outbreak in 1549, the encomederos, crippled by the loss in profits resulting and unable to meet the demands of New Spain, were forced to comply with the new tasaciones (regulations).[38] The new ordinances, known as Leyes Nuevas aimed to limit the amount of tribute encomenderos could personally extract, while also prohibiting them from exercising absolute control over the labor force.[40] Simultaneously, non-encomenderos began claiming lands lost by the encomenderos, as well as, the labor provided by the indigenous. This developed in to the implementation of the repartimiento system, which sought to institute a higher level of oversight within the Spanish colonies and maximize the overall tribute extracted for public and crown use.[38] Rules regarding tribute itself were also changed in response to the epidemic of 1545, as fears over future food shortages ran rampant among the Spanish. By 1577, after years of debate and a second major outbreak of cocoliztli, maize and money were designated as the only two forms of acceptable tribute.[19][38]
Later outbreaks
A second large outbreak of cocoliztli occurred in 1576, lasting until about 1580. Although less destructive (around 2 million deaths) than its predecessor, this outbreak appears in much greater detail in colonial accounts.[18] Many of the descriptions of cocoliztli symptoms, beyond the bleeding, fevers, and jaundice, were recorded during this epidemic. In total, there are 13 cocoliztli epidemics cited in Spanish accounts between 1545 and 1642, with a later outbreak in 1736 taking a similar form, but referred to by a different name (tlazahuatl).[20]
See also
- Virgin soil epidemic
- Columbian Exchange
- Ecological imperialism
- Millenarianism in colonial societies
References
- ↑ Skaarup 2015, p. 205.
- 1 2 3 4 Prem, Hanns (1991). "Disease Outbreaks in Central Mexico During the Sixteenth Century". In Cook, Noble David; Lovell, W. George (eds.). "Secret Judgments of God": Old World Disease in Colonial Spanish America. Norman: University of Oklahoma Press. pp. 20–48. ISBN 0806123729.
- 1 2 3 Vågene, Åshild; et al. (2018). "Salmonella enterica genomes from victims of a major sixteenth-century epidemic in Mexico". Nature Ecology & Evolution. 2 (3): 520–528. doi:10.1038/s41559-017-0446-6. PMID 29335577. S2CID 3358440.
- 1 2 3 4 5 6 7 Acuna-Soto, R.; Stahle, D. W.; Cleaveland, M. K.; Therrell, M. D (April 2002). "Megadrought and megadeath in 16th century Mexico". Emerging Infectious Diseases. 8 (4): 360–362. doi:10.3201/eid0804.010175. PMC 2730237. PMID 11971767.
- 1 2 ""Huey cocoliztli" en el México del siglo XVI: ¿una enfermedad emergente del pasado?". www.madrimasd.org. Retrieved 8 December 2015.
- 1 2 "Fiebres hemorrágicas causa de muerte en las culturas originarias". www.ciudadania-express.com. Retrieved 6 December 2015.
- ↑ Turner, B. L.; Sabloff, J. A. (21 August 2012). "Classic Period collapse of the Central Maya Lowlands: Insights about human-environment relationships for sustainability". Proceedings of the National Academy of Sciences. 109 (35): 13908–13914. Bibcode:2012PNAS..10913908T. doi:10.1073/pnas.1210106109. PMC 3435155. PMID 22912403.
- ↑ Haug, G. H. (14 March 2003). "Climate and the Collapse of Maya Civilization". Science. 299 (5613): 1731–1735. Bibcode:2003Sci...299.1731H. doi:10.1126/science.1080444. PMID 12637744. S2CID 128596188.
- ↑ "Cocoliztli y Matlazahuatl". www.zocalo.com.mx. Retrieved 6 November 2015.
- 1 2 Lovell, W. George (1991). "Disease and Depopulation in Early Colonial Guatemala". In Cook, Noble David; Lovell, W. George (eds.). "Secret Judgments of God": Old World Disease in Colonial Spanish America. Norman: University of Oklahoma Press. pp. 49–83. ISBN 0806123729.
- ↑ Rice, Prudence (2012). "Torata Alta: An Inka Administrative Center and Spanish Colonial Reducción in Moquegua, Peru". Latin American Antiquity. 23 (1): 3–28. doi:10.7183/1045-6635.23.1.3. S2CID 163519431.
- 1 2 3 4 5 Marr, John; Kiracofe, J.B. (2000). "Was Huey Cocoliztli a Haemorrhagic fever?". Medical History. 44 (3): 341–262. doi:10.1017/S0025727300066746. PMC 1044288. PMID 10954969. S2CID 8951159.
- 1 2 Bowen, Michael; Peters, Clarence; Nichol, Stuart (1997). "Phylogenetic Analysis of theArenaviridae: Patterns of Virus Evolution and Evidence for Cospeciation between Arenaviruses and Their Rodent Hosts". Molecular Phylogenetics and Evolution. 8 (3): 301–316. doi:10.1006/mpev.1997.0436. PMID 9417890.
- ↑ Wolfe, Nathan; Dunavan, Claire; Diamond, Jared (2007). "Origins of Major Human Infectious Diseases". Nature. 447 (7142): 279–83. Bibcode:2007Natur.447..279W. doi:10.1038/nature05775. PMC 7095142. PMID 17507975.
- ↑ Reff, Daniel (1991). Disease, Depopulation, and Culture Change in Northwestern New Spain, 1518-1764. Salt Lake City: University of Utah Press. ISBN 0874803551.
- ↑ Newson, Linda (1991). "Old World Epidemics in Ecuador". In Cook, Noble David; Lovell, W. George (eds.). "Secret Judgments of God": Old World Disease in Colonial Spanish America. Norman: University of Oklahoma Press. pp. 84–112. ISBN 0806123729.
- ↑ Evans, Brian (1991). "Death in Aymaya of Upper Peru, 1580–1623". In Cook, Noble David; Lovell, W. George (eds.). "Secret Judgments of God": Old World Disease in Colonial Spanish America. Norman: University of Oklahoma Press. ISBN 0806123729.
- 1 2 3 4 Somolinos d'Ardois, Germaine (1970). "La epidemia de Cocoliztli de 1545 senalada en un codice". Tribuna Medica. 15 (4): 85.
- 1 2 3 Warinner, Christina; et al. (2012). "Disease, demography, and diet in early colonial New Spain: investigation of a sixteenth-century Mixtec cemetery at Teposcolula Yucundaa". Latin American Antiquity. 23 (4): 467–489. doi:10.7183/1045-6635.23.4.467. hdl:11858/00-001M-0000-002B-7496-6. S2CID 163523841.
- 1 2 3 Acuña-Soto, Roldalfo; Calderón Romero, Leticia; Maguire, James (2000). "Large epidemics of hemorrhagic fevers in Mexico 1545–1815". The American Journal of Tropical Medicine and Hygiene. 62 (6): 733–739. doi:10.4269/ajtmh.2000.62.733. PMID 11304065.
- ↑ Siek, Thomas (2013). "The Osteological Paradox and Issues of Interpretation in Paleopathology". Vis-à- Vis: Explorations in Anthropology. 12 (1): 92–101.
- ↑ John Bierhorst, History and Mythology of the Aztecs: The Codex Chimalpopoca pg 66.
- ↑ "La epidemia de cocoliztli de 1576" (PDF). Instituto Nacional de Antropología e Historia. Retrieved 30 November 2015.
- ↑ "500 years later, scientists discover what probably killed the Aztecs". The Guardian. AFP. 18 January 2018. Retrieved 16 January 2018.
- ↑ Hersher, Rebecca (16 January 2017). "Salmonella May Have Caused Massive Aztec Epidemic, Study Finds". National Public Radio. Retrieved 2018-01-17.
- ↑ Judd, Michael; Mintz, Eric (2014). "Chapter 3: Typhoid & Paratyphoid Fever". In Newton, Anna (ed.). CDC Health Information for International Travel: The Yellow Book. Oxford: Oxford Press. ISBN 9780199948499.
- ↑ Smith, Dale (1980). "Gerhard's distinction between typhoid and typhus and its reception in America, 1833-1860". Bulletin of the History of Medicine. 54 (3): 368–385. JSTOR 44441270. PMID 6998525.
- 1 2 Callaway, Ewen (2017). "Collapse of Aztec society linked to catastrophic salmonella outbreak". Nature. 542 (7642): 404. doi:10.1038/nature.2017.21485. PMID 28230141.
- ↑ "2014 National Typhoid and Paratyphoid Fever Surveillance Annual Summary" (PDF). CDC. Retrieved 20 April 2018.
- 1 2 Zhou, Zhemin; et al. (2017). "Millennia of genomic stability within the invasive Para C Lineage of Salmonella enterica". bioRxiv. doi:10.1101/105759.
- ↑ "What Wiped Out the Aztecs? Scientists Find New Clues". National Geographic News. 16 January 2018. Retrieved 6 June 2019.
- ↑ Chen, Angus (16 January 2018). "One of history's worst epidemics may have been caused by a common microbe". Science. Retrieved 6 June 2019.
- ↑ Community, Nature Research Ecology & Evolution (2018-01-15). "Enteric fever in sixteenth-century Mexico". Nature Research Ecology & Evolution Community. Retrieved 2020-04-11.
- ↑ Puente, Jose Luis; Calva, Edmundo (2017). "The One Health Concept—the Aztec empire and beyond". Pathogens and Disease. 75 (6). doi:10.1093/femspd/ftx062. PMID 28605517.
- ↑ Lindqvist, Charlotte; Rajora, Om P., eds. (2019). Paleogenomics: Genome-Scale Analysis of Ancient DNA. Population Genomics. Springer International Publishing. ISBN 978-3-030-04752-8.
- ↑ Community, Nature Research Ecology & Evolution (2018-01-15). "Enteric fever in sixteenth-century Mexico". Nature Research Ecology & Evolution Community. Retrieved 2020-04-11.
- ↑ Acuna-Soto, Rodolfo; et al. (2004). "When half of the population died: the epidemic of hemorrhagic fevers of 1576 in Mexico". FEMS Microbiology Letters. 240 (1): 1–5. doi:10.1016/j.femsle.2004.09.011. PMC 7110390. PMID 15500972.
- 1 2 3 4 5 Gibson 1964.
- ↑ Espinsoa, Aurelio (2006). "The Spanish Reformation: Institutional Reform, Taxation, And The Secularization Of Ecclesiastical Properties Under Charles V". The Sixteenth Century Journal. 37 (1): 3–24.
- ↑ Prem, Hanns (1992). "Spanish colonization and Indian property in central Mexico, 1521–1620". Annals of the Association of American Geographers. 82 (3): 444–459. doi:10.1111/j.1467-8306.1992.tb01969.x.
Bibliography
- Skaarup, Bjørn Okholm (2015). Anatomy and Anatomists in Early Modern Spain (1st ed.). Routledge. p. 205. ISBN 978-1472448262.
- Gibson, Charles (1964). The Aztecs Under Spanish Rule: A history of the Indians of the Valley of Mexico 1519–1810. Stanford: Stanford University Press.
External links
- "Megadeath in Mexico". discovermagazine.com. Retrieved 2015-11-28.
- "'Ebola' bug wiped out the Aztecs". The Guardian. Retrieved 2015-11-28.
- "Expert: Native disease killed Aztecs, not outsiders". chron.com. Retrieved 2015-12-05.
La Epidemica De Cocoliztli
La epidemia de cocoliztli, o la gran pestilencia, es un término dado a millones de muertes en el territorio de la Nueva España en el actual México en el siglo XVI atribuidas a una o más enfermedades denominadas colectivamente cocoliztli, una enfermedad misteriosa caracterizada por fiebres altas y sangrado. Devastó el altiplano mexicano en proporciones epidémicas. La enfermedad se conoció como Cocoliztli por los nativos aztecas y tuvo efectos devastadores en la demografía del área, particularmente para los indígenas.
Con base en el número de muertos, este brote a menudo se conoce como la peor epidemia de enfermedad en la historia de México. Los brotes posteriores continuaron desconcertando tanto a los médicos españoles como a los nativos, con poco consenso entre los investigadores modernos sobre la patogenia. Sin embargo, estudios genómicos bacterianos recientes han sugerido que Salmonella, específicamente un serotipo de Salmonella enterica conocido como Paratyphi C, fue al menos parcialmente responsable de este brote inicial. También podría haber sido una fiebre hemorrágica viral indígena, quizás exacerbada por las peores sequías que afectaron a esa región en 500 años, así como las condiciones de vida de los pueblos indígenas de México a raíz de la conquista española (c. 1519).