Third plague pandemic
| Third plague pandemic | |
|---|---|
 Plague patient being injected by a doctor in 1897, British Raj India. | |
 Bubo of the axi in bubonic plague | |
| Disease | Bubonic plague |
| Bacteria strain | Yersinia pestis species (Genus:Yersinia) [1] |
| Source | Ground rodent(Rattus flavipectus)[2] (Rattus rattus)[3] |
| Location | India, China, worldwide[1] |
| First reported | Yunnan, China[4] |
| Date | 1855–1960 (105 years)[5] |
| Hospitalized cases | statistics were not kept during this period |
Deaths | 15 million total[6][7] (10 million in India, 2 million in China, 3 million elsewhere) |
Territories | Europe, Asia[1] |
The third plague pandemic (or third bubonic plague pandemic[8])was a major bubonic plague pandemic that began in Yunnan, China, in 1855.[4] This episode of bubonic plague spread to all inhabited continents, and ultimately led to more than 12 million deaths in India and China[9] (and perhaps over 15 million worldwide[6]), and at least 10 million Indians were killed in British Raj India alone, making it one of the deadliest pandemics in history.[10][6][11] According to the World Health Organization, the pandemic was considered active until 1960 when worldwide casualties dropped to 200 per year. Plague deaths have continued at a lower level for every year since.[12]
The name refers to the third of at least three known major plague pandemics.[13] The first began with the Plague of Justinian, which ravaged the Byzantine Empire and surrounding areas in 541 and 542; the pandemic persisted in successive waves until the middle of the 8th century. The second began with the Black Death, which killed at least one third of Europe's population in a series of expanding waves of infection from 1346 to 1353; this pandemic recurred regularly until the 19th century.[14]
Casualty patterns indicate that waves of this late-19th-century/early-20th-century pandemic may have come from different sources. One was primarily bubonic and was carried around the world through ocean-going trade, through transporting infected persons, rats, and cargoes harboring fleas. The other strain was primarily pneumonic in character with a strong person-to-person contagion, this strain was largely confined to Asia.[15][16]
Epidemiology
The bubonic plague was endemic in populations of infected ground rodents in Central Asia and was a known cause of death among the migrant and established human populations in that region for centuries. An influx of new people because of politics and global trade led to the spread of the disease throughout the world from Asia to the rest of Europe, and other regions.[3][17]
A natural reservoir or nidus for plague is in western Yunnan and is still an ongoing health risk. The third pandemic of plague originated in the area after a rapid influx of Han Chinese to exploit the demand for minerals, primarily copper, in the second half of the 19th century.[2] By 1850, the population had exploded to over 7 million people. Increasing transportation throughout the region brought people in contact with plague-infected fleas, the primary vector between the yellow-breasted rat (Rattus flavipectus) and humans. People brought the fleas and rats back into growing urban areas, where small outbreaks sometimes reached epidemic proportions. The plague spread further and began to appear in the Pearl River delta, including Canton and Hong Kong. Although William McNeil and others believe the plague to have been brought from the interior to the coastal regions by troops returning from battles against the Muslim rebels, Benedict suggested evidence to favor the growing and lucrative opium trade, which began after about 1840.[2]
In the city of Canton, beginning in March 1894, the disease killed 80,000 people in a few weeks. Daily water-traffic with the nearby city of Hong Kong rapidly spread the plague. Within two months, after 100,000 deaths, the death rates dropped below epidemic rates, but the disease continued to be endemic in Hong Kong until 1929.[18]
Distribution
The network of global shipping ensured the widespread distribution of the disease over the next few decades.[19][20][21][22] Recorded outbreaks included the following:
- Beihai, Qing China 1882.[2]
- Guangzhou, Qing China 1894.[2]
- British Hong Kong 1894.[2]
- Japanese Taiwan, Empire of Japan 1896 [19]
- Bombay Presidency, India, 1896–1898.[23]
- Calcutta, India, 1898.[24]
- French Madagascar, 1898.[25]
- Kobe, 1898.[26]
- Khedivate of Egypt, 1899.[27]
- Paraguay, 1899.[28]
- Porto, Portugal, 1899.[29]
- Republic of Hawaii, 1899–1900.[30][31]
- Glasgow, United Kingdom, 1900.[32]
- San Francisco, United States, 1900.[33][34][35]
- Manila, 1900.[36]
- Australia, 1900–1905.[37]
- Fujian, China 1901.[38]: 165
- Johannesburg, South Africa, 1904.[39]
- British Burma, 1905.[40]
- French Tunisia, 1907.[38]: 311
- Venezuela, and Ecuador, 1908.[41]
- Bolivia and Brazil, 1908.[38]: 311
- Freston, Suffolk, United Kingdom, 1910 (disputed)[42][43][44]
- Northeast China 1910-1911[45]
- Puerto Rico, 1912.[46]
Each of the areas, as well as areas of Europe, continued to experience plague outbreaks and casualties until the 1960s, although extremely few of these occurred after 1950.The last significant outbreak of plague associated with the pandemic occurred in Peru and Argentina in 1945.[5][38]: 561
1894 Hong Kong plague

The 1894 Hong Kong plague was a major outbreak of the third global pandemic from the late 19th century to the early 20th century.[16]
The hardest hit was the mountainous area in Sheung Wan, the most densely-populated area in Hong Kong, characterised by Chinese-style buildings. From May to October 1894, the plague killed more than 6,000 people, leading to the exodus of one third of the population.Through maritime traffic, the epidemic spread to the rest of the country after 1894 and eventually spread to British Raj India where about ten million Indians were killed.[18][47][48]
There were several reasons for the rapid outbreak and spread of the plague. Firstly, in the early days, Sheung Wan was a Chinese settlement. Houses — in the mountains — had no drainage channels, toilets, or running water. The houses were small and the floors were not paved. Secondly, during the Ching Ming Festival in 1894, many Chinese living in Hong Kong returned to the countryside to tend to family graves, which coincided with the outbreak of the epidemic in Canton and the introduction of bacteria into Hong Kong. Thirdly, in the first four months of 1894, rainfall decreased and soil dried up, accelerating the spread of the plague.[49]
The main preventive measures were setting up plague hospitals and deploying medical staff to treat and isolate plague patients; conducting house-to-house search operations, discovering and transferring plague patients, and cleaning and disinfecting infected houses and areas; and setting up designated cemeteries and assigning a person responsible for transporting and burying the plague dead.[50]
Etiology
Yersinia pestis is a gram-negative, non-motile, coccobacillus bacterium without spores that is related to both Yersinia pseudotuberculosis and Yersinia enterocolitica. It is a facultative anaerobic organism.[51]
It causes the disease plague, which caused the first plague pandemic and the Black Death, the deadliest pandemic in recorded history[52]. Plague takes three main forms: pneumonic, septicemic, and bubonic.[53] Yersinia pestis is a parasite of its host, the rat flea, which is also a parasite of rats[54]
Disease research
_-_fotografias_de_Ant%C3%B3nio_Pl%C3%A1cido_da_Costa_(Museu_de_Hist%C3%B3ria_da_Medicina_Maximiano_Lemos%252C_FMUP).png.webp)
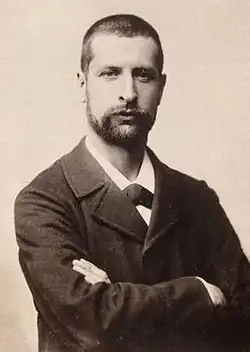
Researchers working in Asia during the "Third Pandemic" identified plague vectors and the plague bacillus. In 1894, in Hong Kong, Swiss-born French bacteriologist Alexandre Yersin isolated the responsible bacterium (Yersinia pestis, named for Yersin) and determined the common mode of transmission.His discoveries led in time to modern treatment methods, including insecticides, the use of antibiotics and eventually plague vaccines. [16] [55] [56]
In 1898, French researcher Paul-Louis Simond demonstrated the role of fleas as a vector[57]
The disease is caused by a bacterium usually transmitted by the bite of fleas from an infected host, often a black rat. The bacteria are transferred from the blood of infected rats to flea (Xenopsylla cheopis). The bacillus multiplies in the stomach of the flea, blocking it. When the flea next bites a mammal, the consumed blood is regurgitated along with the bacillus into the bloodstream of the bitten animal. Any serious outbreak of plague in humans is preceded by an outbreak in the rodent population. During the outbreak, infected fleas that have lost their normal rodent hosts seek other sources of blood.[58]
The British colonial government in India pressed medical researcher Waldemar Haffkine to develop a plague vaccine. After three months of persistent work with a limited staff, a form for human trials was ready. On January 10, 1897, Haffkine tested it on himself. After the initial test was reported to the authorities, volunteers at the Byculla jail were used in a control test. All inoculated prisoners survived the epidemics, while seven inmates of the control group died. By the turn of the century, the number of inoculees in India alone reached four million. Haffkine was appointed the Director of the Plague Laboratory, now called the Haffkine Institute, in Bombay.[59]
New international health organizations
.svg.png.webp)
In the early 1900s, despite the increasing knowledge of germ theory and the rapid growth of scientific communities around the prevention of major disease, there was little the international communities could do other than create standard protocols for how to deal with an outbreak of the plague.[8] In 1897 and 1903, two conventions were held known as International Sanitary Conferences; the first in Venice and the second in Paris, to help deal with threat of the new outbreaks of the bubonic plague. From these conventions was formed an international disease convention supervised by the Office International D'hygiene Publique (OIHP) in Paris which would be one of the major predecessors of the League of Nations health organization.[8] From these conventions came the standard Protocols used in dealing with the bubonic plague throughout the early 1900s.[8] These protocols were often old fashioned and were generally summarized as the 3 "I's": Isolation, Incineration, and Inoculation. Isolation is a standard protocol of many modern disease outbreaks, but the usage of incineration was a protocol of disease control used most uniquely for dealing with the bubonic plague.[8] Burning was used often to deal with the Plague as it was believed to the be most effective way to eliminate strains of the disease from places inhabited by the infected.[8] But it was also a problematic technique as it led to the creation of many out-of-control fires that devastated communities, the most notable being the great fire in Honolulu which devastated the Chinatown community there.[8] Inoculation was the usage of newly invented plague vaccines, with some in India being recorded to have an efficacy of over 50%.[60]
Social implications
In many instances, the third plague pandemic either revealed or exacerbated major social conflicts and racial inequalities.[8] Many of the ports infected during the plague were at the time British-held colonies. This meant that in these colonies the British Empire was responsible for most of the actions used to prevent the disease.[61]
Because of this the British often ended up enforcing western hygiene and medical practices and radical quarantine measures in countries and provinces such as India, and other countries. Many of these imposed western sanitary measures were new to these areas and caused natives fear and apprehension of the British government.[62][63]
In India harsh quarantines were initially implemented by the British governments, leading to Indian resentment of quarantine measures.[61] In South Africa when the plague broke out in Cape Colony, the British government caused a large group of native South Africans to move out of a supposed slum into areas on the outskirts of the city, which many historians argue was a racially motivated move by white South Africans to segregate African-born South Africans in other parts of the city.[64] In Hong Kong the British enforced many locally unfamiliar medical practices, such as floating plague victims out on boats onto the water and cooling plague victims with ice, which scared many Chinese residents of Hong Kong and led to their migrating back to mainland China, which was even more badly affected by the plague.[65]
Another instance of social harm caused by the response to the plague is the great fire of Honolulu in 1900, which caused the Chinatown in Honolulu to be destroyed, rendering over 7,000 Chinese and Japanese residents homeless.[8] In America when the plague reached San Francisco, the medical board of the city implemented a strict quarantine of the entire Chinatown district after discovering only one case of the plague; this has led many to question whether this measure was motivated by racial bias among medical professionals, who may have believed Chinatown to be unsanitary and hence already infected by the plague.[66]
See also
- Timeline of plague
- British Raj India pandemics
References
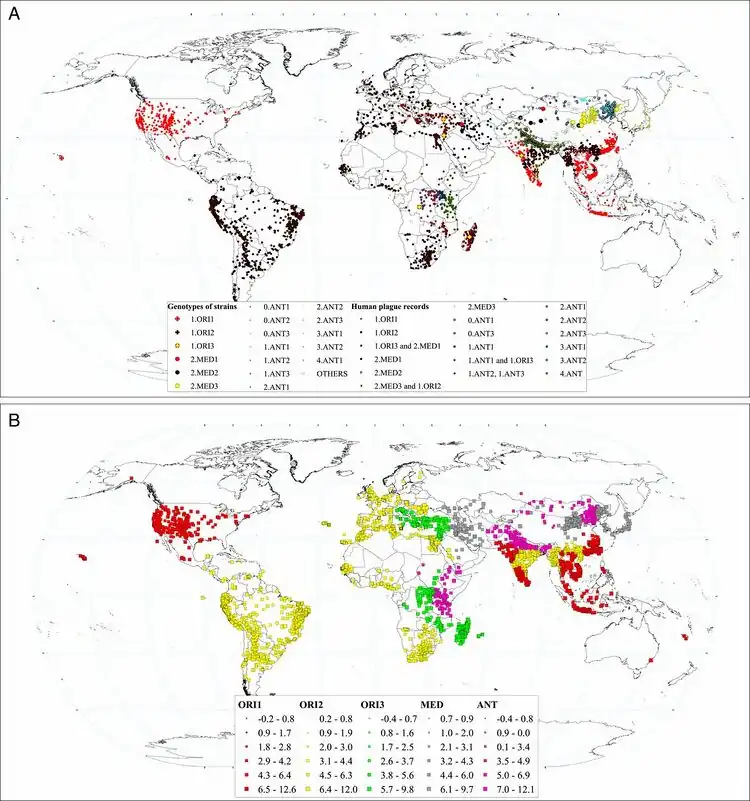
- 1 2 3 Xu, Lei; Stige, Leif C.; Leirs, Herwig; Neerinckx, Simon; Gage, Kenneth L.; Yang, Ruifu; Liu, Qiyong; Bramanti, Barbara; Dean, Katharine R.; Tang, Hui; Sun, Zhe; Stenseth, Nils Chr.; Zhang, Zhibin (11 June 2019). "Historical and genomic data reveal the influencing factors on global transmission velocity of plague during the Third Pandemic". Proceedings of the National Academy of Sciences. 116 (24): 11833–11838. doi:10.1073/pnas.1901366116. ISSN 0027-8424. Archived from the original on 5 August 2023. Retrieved 2 August 2023.
- 1 2 3 4 5 6 Benedict, Carol (1996). Bubonic plague in eighteenth-century China. Stanford, CA: Stanford Univ. Press. pp. 47, 70. ISBN 978-0804726610.
- 1 2 Bramanti, B; Dean, KR; Walløe, L; Chr Stenseth, N (24 April 2019). "The Third Plague Pandemic in Europe". Proceedings. Biological sciences. 286 (1901): 20182429. doi:10.1098/rspb.2018.2429. PMID 30991930. Archived from the original on 25 March 2020. Retrieved 2 August 2023.
- 1 2 Cohn, Samuel K. (2003). The Black Death Transformed: Disease and Culture in Early Renaissance Europe. A Hodder Arnold. p. 336. ISBN 0-340-70646-5.
- 1 2 Glatter, KA; Finkelman, P (February 2021). "History of the Plague: An Ancient Pandemic for the Age of COVID-19". The American journal of medicine. 134 (2): 176–181. doi:10.1016/j.amjmed.2020.08.019. PMID 32979306. Archived from the original on 18 June 2022. Retrieved 2 August 2023.
- 1 2 3 Frith, John. "The History of Plague – Part 1. The Three Great Pandemics". Journal of Military and Veterans' Health. 20 (2). Archived from the original on 2019-10-02. Retrieved 2023-07-06.
The third pandemic waxed and waned throughout the world for the next five decades and did not end until 1959, in that time plague had caused over 15 million deaths, the majority of which were in India.
- ↑ Srivastava, K; Chaudhry, S; Sowmya, AV; Prakash, J (January 2020). "Mental health aspects of pandemics with special reference to COVID-19". Industrial psychiatry journal. 29 (1): 1–8. doi:10.4103/ipj.ipj_64_20. PMID 33776268. Archived from the original on 18 August 2023. Retrieved 15 August 2023.
- 1 2 3 4 5 6 7 8 9 Echenberg, Myron (2002). "Pestis Redux: The Initial Years of the Third Bubonic Plague Pandemic, 1894-1901". Journal of World History. 13 (2): 429–449. doi:10.1353/jwh.2002.0033. ISSN 1045-6007. JSTOR 20078978. PMID 20712094. S2CID 45975258. Archived from the original on 2021-05-22. Retrieved 2023-07-06.
- ↑ "Plague deaths: Quarantine lifted after couple die of bubonic plague". BBC News. 2019-05-07. Archived from the original on 2021-10-24. Retrieved 2021-08-28.
In the 19th Century there was a plague outbreak in China and India, which killed more than 12 million.
- ↑ Stenseth, Nils Chr (2008-08-08). "Plague Through History". Science. 321 (5890): 773–774. doi:10.1126/science.1161496. ISSN 0036-8075. S2CID 161336516. Archived from the original on 2023-04-13. Retrieved 2023-07-06.
- ↑ Sanburn, Josh (2010-10-26). "Top 10 Terrible Epidemics: The Third Plague Pandemic". Time. ISSN 0040-781X. Archived from the original on 2021-02-14. Retrieved 2021-01-01.
- ↑ Høiby, Niels (July 2021). "Pandemics: past, present, future: That is like choosing between cholera and plague". APMIS. 129 (7): 352–371. doi:10.1111/apm.13098. ISSN 1600-0463. PMC 7753327. PMID 33244837.
- ↑ Stenseth, Nils Chr; Atshabar, Bakyt B; Begon, Mike; Belmain, Steven R; Bertherat, Eric; Carniel, Elisabeth; Gage, Kenneth L; Leirs, Herwig; Rahalison, Lila (January 2008). "Plague: Past, Present, and Future". PLOS Medicine. 5 (1): e3. doi:10.1371/journal.pmed.0050003. ISSN 1549-1277. PMC 2194748. PMID 18198939.
- ↑ Huremović, Damir (16 May 2019). "Brief History of Pandemics (Pandemics Throughout History)". Psychiatry of Pandemics: 7–35. doi:10.1007/978-3-030-15346-5_2. ISBN 978-3-030-15345-8. PMC 7123574.
- ↑ Kausrud, Kyrre Linné; Begon, Mike; Ari, Tamara Ben; Viljugrein, Hildegunn; Esper, Jan; Büntgen, Ulf; Leirs, Herwig; Junge, Claudia; Yang, Bao; Yang, Meixue; Xu, Lei; Stenseth, Nils Chr (27 August 2010). "Modeling the epidemiological history of plague in Central Asia: Palaeoclimatic forcing on a disease system over the past millennium". BMC Biology. 8 (1): 112. doi:10.1186/1741-7007-8-112. ISSN 1741-7007. Archived from the original on 2023-08-11. Retrieved 9 August 2023.
- 1 2 3 Bramanti, Barbara; Dean, Katharine R.; Walløe, Lars; Chr. Stenseth, Nils (24 April 2019). "The Third Plague Pandemic in Europe". Proceedings of the Royal Society B: Biological Sciences. The Royal Society. 286 (1901): 20182429. doi:10.1098/rspb.2018.2429. PMC 6501942. PMID 30991930.
- ↑ DO, Pamela G. Rockwell (3 November 2017). Vaccine Science and Immunization Guideline: A Practical Guide for Primary Care. Springer. p. 6. ISBN 978-3-319-60471-8. Archived from the original on 14 August 2023. Retrieved 14 August 2023.
- 1 2 Pryor, E.G. (1975). "The Great Plague of Hong Kong" (PDF). Journal of the Hong Kong Branch of the Royal Asiatic Society. 15: 61–70. PMID 11614750. Archived (PDF) from the original on 2020-10-24. Retrieved 2023-07-06.
- 1 2 Tsai, Hungyin (10 August 2022). "The History of Vaccine Uptake in Taiwan". American Scientist. Archived from the original on 22 October 2022. Retrieved 3 August 2023.
- ↑ Low, Bruce (1899). "Report upon the Progress and Diffusion of Bubonic Plague from 1879 to 1898". Reports of the Medical Officer of the Privy Council and Local Government Board, Annual Report, 1898–99. London: Darling & Son, Ltd. on behalf of His Majesty's Stationery Office: 199–258. Retrieved 17 October 2010.
- ↑ Low, Bruce (1902). "Summary of the Progress and Diffusion of the Plague in 1900". Reports of the Medical Officer of the Privy Council and Local Government Board, Annual Report, 1900–01. London: Darling & Son, Ltd. on behalf of His Majesty's Stationery Office: 264–282. Retrieved 17 October 2010.
- ↑ Eager, J.M. (1908). "The Present Pandemic of Plague". Public Health Bulletin. Washington: Government Printing Office: 436–443. Retrieved 17 October 2010.
- ↑ "The Bombay plague | National Army Museum". www.nam.ac.uk. Archived from the original on 2023-03-23. Retrieved 2023-08-04.
- ↑ Patterson, R. F. (1898). "INDIA. Existence of plague at Calcutta suspected". Public Health Reports (1896-1970). 13 (22): 571–571. ISSN 0094-6214. Retrieved 4 August 2023.
- ↑ Chanteau, Suzanne; Ratsifasoamanana, Lala; Rasoamanana, Bruno; Rahalison, Lila; Randriambelosoa, Jean; Roux, Jean; Rabeson, Dieudonné. "Plague, a Reemerging Disease in Madagascar - Volume 4, Number 1—March 1998 - Emerging Infectious Diseases journal - CDC". doi:10.3201/eid0401.980114. Archived from the original on 2 April 2023. Retrieved 4 August 2023.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "Report on the epidemic of plague in Kobe and Osaka from November, 1899, to January, 1900". Public Health Reports (1896-1970). 16 (14): 671–677. 1901. ISSN 0094-6214. Retrieved 4 August 2023.
- ↑ "Egypt: Report from Alexandria. History of Plague in Egypt, 1899-1908. Transmission of Plague by Rats. Sanitary Measures Enforced in Cities". Public Health Reports (1896-1970). 24 (2): 39–40. 1909. ISSN 0094-6214. Retrieved 4 August 2023.
- ↑ Hollis, W. Stanley (1899). "AFRICA. Disease at Magude thought to be plague". Public Health Reports (1896-1970). 14 (45): 1994–1994. ISSN 0094-6214. Retrieved 5 August 2023.
- ↑ (:Unkn) Unknown (2018). "Plague Hospital in Porto - 1899". Apollo - University of Cambridge Repository. doi:10.17863/CAM.32180. Archived from the original on 6 February 2021. Retrieved 1 March 2020.
- ↑ "Honolulu's Battle with Bubonic Plague". Hawaiian Almanac and Annual. Honolulu: Thos. G. Thrum, Hawaiian Gazette Co.: 97–105 1900. Archived from the original on 5 August 2023. Retrieved 17 October 2010.
- ↑ Kevin R. Bailey (June 2007). "Plague in paradise : a study of plague on Hawaiian sugarcane plantations" (PDF). Department of History and the Honors College of the University of Oregon. p. 3. Archived (PDF) from the original on 2011-07-18. Retrieved 2023-07-06.
- ↑ MacDonald, Kenneth (2 January 2019). "Rats 'wrongly blamed' for 1900 Glasgow plague outbreak". BBC News. Archived from the original on 2 January 2019. Retrieved 2 January 2019.
- ↑ "On The Plague In San Francisco". Journal of the American Medical Association. Chicago: The American Medical Association. 36 (15): 1042. April 13, 1901. doi:10.1001/jama.1901.52470150038003. Archived from the original on 5 August 2023. Retrieved 17 October 2010.
- ↑ "The Plague, "American Medicine," And The "Philadelphia Medical Journal."". Occidental Medical Times. San Francisco. 15: 171–179. 1901. Archived from the original on 5 August 2023. Retrieved 17 October 2010.
- ↑ "Bubonic Plague At San Francisco, Cal". Annual Report of the Supervising Surgeon General of the Marine Hospital Service of the United States for the Fiscal Year 1901. Washington: Government Printing Office: 491–. 1901. Retrieved 17 October 2010.
- ↑ Curry, Joseph J. (21 March 1901). "Bubonic Plague: Report on the Plague in Manila, P. I., from Jan. 1, 1900 to June 30, 1900". The Boston Medical and Surgical Journal. 144 (12): 277–279. doi:10.1056/NEJM190103211441203. ISSN 0096-6762. Archived from the original on 5 August 2023. Retrieved 5 August 2023.
- ↑ "The University of Sydney School of Medicine". University of Sydney. Archived from the original on 30 May 2023. Retrieved 5 August 2023.
- 1 2 3 4 Kohn, George C. (2007). Encyclopedia of Plague and Pestilence: From Ancient Times to the Present. Infobase Publishing. ISBN 978-1-4381-2923-5. Archived from the original on 2023-08-08. Retrieved 2023-08-06.
- ↑ Evans, Charles M.; Egan, Joseph R.; Hall, Ian (January 2018). "Pneumonic Plague in Johannesburg, South Africa, 1904". Emerging Infectious Diseases. 24 (1). doi:10.3201/eid2401.161817.
- ↑ Keck, Stephen L. (6 October 2015). British Burma in the New Century, 1895–1918. Springer. ISBN 978-1-137-36433-3. Archived from the original on 8 August 2023. Retrieved 7 August 2023.Google books does not offer page number
- ↑ Bezerra, Matheus Filgueira; de Almeida, Alzira Maria Paiva (2022). "Important Infectious Diseases in Latin America and the Caribbean: Plague". Infectious Tropical Diseases and One Health in Latin America. Springer International Publishing. pp. 45–70. ISBN 978-3-030-99712-0. Archived from the original on 8 August 2023. Retrieved 7 August 2023.
- ↑ Zwanenberg, D Van (Jan 1970). "The last epidemic of plague in England? Suffolk 1906-1918". Medical History. 14 (1): 63–74. doi:10.1017/s0025727300015143. PMC 1034015. PMID 4904731.
- ↑ Benedictow, Ole Jørgen (2004). The Black Death, 1346-1353: the complete history. Boydell & Brewer. p. 20. ISBN 0-85115-943-5.
- ↑ Shrewsbury, J. F. D. (2005). A History of Bubonic Plague in the British Isles. Cambridge University Press. pp. 509–510. ISBN 0-521-02247-9.
- ↑ Q, Zhang; F, Zhang; B, Yang (2018). "Pneumonic plague epidemic in Northeast China in 1910-1911: Dr. Wu Lien-Teh's epidemic preventive system for plague control". Frontiers of medicine. 12 (1). doi:10.1007/s11684-018-0613-4. ISSN 2095-0225. Archived from the original on 25 May 2022. Retrieved 6 August 2023.
- ↑ Zulawski, Ann (September 2018). "Environment, Urbanization, and Public Health: The Bubonic Plague Epidemic of 1912 in San Juan, Puerto Rico". Latin American Research Review. 53 (3): 500–516. doi:10.25222/larr.424. ISSN 0023-8791. Archived from the original on 12 October 2022. Retrieved 6 August 2023.
- ↑ Sihn, Kyu-Hwan (April 2017). "Reorganizing Hospital Space: The 1894 Plague Epidemic in Hong Kong and the Germ Theory". Ui Sahak. 26 (1): 59–94. doi:10.13081/kjmh.2017.26.59. ISSN 1225-505X. Archived from the original on 11 August 2023. Retrieved 9 August 2023.
- ↑ Catanach, I. J. (1 March 2017). "Plague and the tensions of empire: India, 1896–1918". Imperial medicine and indigenous societies. Manchester University Press: 149–171. Archived from the original on 14 August 2023. Retrieved 13 August 2023.
- ↑ "1894上環大鼠疫". elearning.qcobass.edu.hk. Archived from the original on 2004-03-24. Retrieved 2019-03-06.
- ↑ 楊, 祥銀 (2010). "公共衛生與1894年香港鼠疫研究". 華中師範大學學報. 49: 68–75.
- ↑ Ryan, KJ; Ray, CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 484–88. ISBN 978-0-8385-8529-0.
- ↑ Cohn SK, Jr (2008). "Epidemiology of the Black Death and successive waves of plague". Medical history. Supplement (27): 74–100. PMID 18575083. Archived from the original on 21 April 2021. Retrieved 10 August 2023.
- ↑ "Plague | CDC Yellow Book 2024". wwwnc.cdc.gov. Archived from the original on 11 August 2023. Retrieved 10 August 2023.
- ↑ Clements, Bruce W. (1 January 2009). "Chapter 2 - Bioterrorism". Disasters and Public Health. Butterworth-Heinemann. pp. 27–63. ISBN 978-1-85617-612-5. Retrieved 10 August 2023.
- ↑ "Alexandre Yersin, the man who discovered the bacterium responsible for the plague". Institut Pasteur. 24 October 2017. Archived from the original on 3 June 2023. Retrieved 12 August 2023.
- ↑ Hawgood, Barbara J. (August 2008). "Alexandre Yersin (1863-1943): discoverer of the plague bacillus, explorer and agronomist". Journal of Medical Biography. 16 (3): 167–172. doi:10.1258/jmb.2007.007017. ISSN 0967-7720. Archived from the original on 18 May 2022. Retrieved 12 August 2023.
- ↑ Simond, M.; Godley, M. L.; Mouriquand, P. D. (February 1998). "Paul-Louis Simond and his discovery of plague transmission by rat fleas: a centenary". Journal of the Royal Society of Medicine. 91 (2): 101–104. doi:10.1177/014107689809100219. ISSN 0141-0768. Archived from the original on 31 January 2021. Retrieved 11 August 2023.
- ↑ Hanhart, Joel. Waldemar Mordekhaï Haffkine (1860–1930). Biographie intellectuelle. Honore Champion.
- ↑ Hanhart, Joel (2016). Waldemar Mordekhaï Haffkine (1860–1930). Biographie intellectuelle. Paris: Honore Champion.
- ↑ Hawgood, Barbara J (2007-02-01). "Waldemar Mordecai Haffkine, CIE (1860–1930): prophylactic vaccination against cholera and bubonic plague in British India". Journal of Medical Biography. 15 (1): 9–19. doi:10.1258/j.jmb.2007.05-59. ISSN 0967-7720. PMID 17356724. S2CID 42075270. Archived from the original on 2023-08-05. Retrieved 2023-07-06.
- 1 2 Chatterjee, Srilata (2005). "Plague and Politics in Bengal 1896 to 1898". Proceedings of the Indian History Congress. 66: 1194–1201. ISSN 2249-1937. JSTOR 44145931. Archived from the original on 2021-05-22. Retrieved 2023-07-06.
- ↑ Yip, Ka-che (June 2012). "Segregation, Isolation, and Quarantine: Protecting Hong Kong from Diseases in the Pre-war Period". The Journal of Comparative Asian Development. 11 (1): 93–116. doi:10.1080/15339114.2012.668110. ISSN 1533-9114.
- ↑ Cohn, Samuel (2021). "Plague in India: Contagion, Quarantine, and the Transmission of Scientific Knowledge". Plague Image and Imagination from Medieval to Modern Times. Springer International Publishing. pp. 191–203. ISBN 978-3-030-72304-0. Archived from the original on 13 August 2021. Retrieved 15 August 2023.
- ↑ Swanson, Maynard W. (July 1977). "The Sanitation Syndrome: Bubonic Plague and Urban Native Policy in the Cape Colony, 1900–1909". The Journal of African History. 18 (3): 387–410. doi:10.1017/S0021853700027328. ISSN 1469-5138. PMID 11632219. S2CID 43662707. Archived from the original on 2021-05-25. Retrieved 2023-07-06.
- ↑ Benedict, Carol (1988). "Bubonic Plague in Nineteenth-Century China". Modern China. 14 (2): 107–155. doi:10.1177/009770048801400201. ISSN 0097-7004. JSTOR 189268. PMID 11620272. S2CID 33772946. Archived from the original on 2022-01-09. Retrieved 2023-07-06.
- ↑ Vavlas, Belinda A. (2010). Anti-Chinese Discrimination in Twentieth Century America: Perceptions of Chinese Americans During the Third Bubonic Plague Pandemic in San Francisco, 1900-1908 (Thesis). Youngstown State University. Archived from the original on 2021-05-21. Retrieved 2023-07-06.
Further reading
- Advisory Committee for Plague Investigations in India (1911), Report On Plague Investigations In India, 1906–1910
- Hazrat Mirza Ghulam Ahmad, The Promised Messiah. Noah’s Ark: An Invitation to Faith.
- Gandhi, M. K. The Plague Panic in South Africa
- Gregg, Charles. Plague: An Ancients Disease in the Twentieth Century. Albuquerque, University of New Mexico Press, 1985.
- Kelly, John. The Great Mortality: An Intimate History of the Black Death, the Most Devastating Plague of All Time. New York: HarperCollins Publishers, 2005. ISBN 0-06-000692-7.
- McNeill, William H. Plagues and People. New York: Anchor Books, 1976. ISBN 0-385-12122-9.
- Orent, Wendy. Plague: The Mysterious Past and Terrifying Future of the World's Most Dangerous Disease. New York: Free Press, 2004. ISBN 0-7432-3685-8.
- Frith, John. "The History of Plague – Part 1. The Three Great Pandemics". JMVH. 20 (2). Archived from the original on 2 October 2019. Retrieved 2 September 2022.
- Glatter, Kathryn A.; Finkelman, Paul (1 February 2021). "History of the Plague: An Ancient Pandemic for the Age of COVID-19". The American Journal of Medicine. 134 (2): 176–181. doi:10.1016/j.amjmed.2020.08.019. PMC 7513766. PMID 32979306.
- Bramanti, Barbara; Dean, Katharine R.; Walløe, Lars; Chr. Stenseth, Nils (24 April 2019). "The Third Plague Pandemic in Europe". Proceedings of the Royal Society B: Biological Sciences. 286 (1901): 20182429. doi:10.1098/rspb.2018.2429. PMC 6501942. PMID 30991930.
External links
- Visual Representations of the Third Plague Pandemic Archived 2021-09-28 at the Wayback Machine