1924 Los Angeles pneumonic plague outbreak
| 1924 Los Angeles pneumonic plague outbreak | |
|---|---|
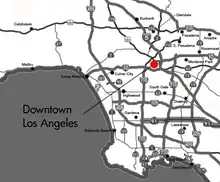 Downtown area of Los Angeles, California | |
| Disease | Pneumonic plague |
| Source | Rats[1] |
| Location | Los Angeles, California, United States |
| Index case | Jesús Lajun[2] |
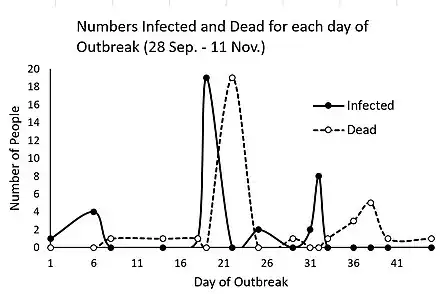
| Date | September 28, 1924[1] to November 13, 1924[3] |
| Suspected cases‡ | 37 (clinically diagnosed)[3] |
Deaths | 30[4] |
| ‡Suspected cases have not been confirmed by laboratory tests as being due to this strain, although some other strains may have been ruled out. | |
The 1924 Los Angeles pneumonic plague outbreak was an outbreak of the pneumonic plague in Los Angeles, California that began on September 28, 1924 and was declared fully contained on November 13, 1924.[3] It represented the first time that the plague had emerged in Southern California; plague outbreaks previously surfaced in San Francisco and Oakland. The outbreak killed 30 people and infected several more.[4] Public health officials credited the lessons learned from the San Francisco outbreak with saving lives, and swiftly implemented preventative measures, including hospitalization of the sick and all their contacts, a neighborhood quarantine, and a large-scale rat eradication program.[4][5][6][7] The epicenter of the plague was in the Macy Street District, primarily home to Mexican immigrants.[4] Racism against Mexican Americans tainted the reaction to the plague, an issue not made public until the outbreak concluded.[8][9] This outbreak was the last instance of aerosol transmission of the plague[10] and the last major plague outbreak in the United States.[11]
Background
During the 1920s, thousands of Mexicans crossed the border to work on large plantations that thrived on "cheap, compliant labor." The large plantation owners supported open immigration, because Mexicans were thought of as "docile and backward." However, immigrants faced a backlash from labor unions which supported increased border security and often expressed racists tendencies towards Hispanic immigrants due to the belief that cheap labor on plantations would favor immigrants instead of American workers. In addition, Hispanics also had to face the stereotype of spreading crime and disease, and some worried that they refused to assimilate into white America. As a consequence, Hispanics were often "physically isolated from the white" communities of Los Angeles.[8] At the time, roughly 19% of Los Angeles residents were foreign born, 22,000 of which were Mexican.[4]
At the time, Los Angeles, being the largest city on the West Coast and the fifth-largest in the country, was growing on an economy primarily reliant on its flourishing tourism industry, a "land boom," and a new harbor.[4] An ideal climate allowed its population to explode in the early 20th century: it grew by 80.66% between 1910 and 1920 and by 114.69% between 1920 and 1930.[12]
Mexicans in Los Angeles mostly settled in Eastern Los Angeles and unincorporated territory of Los Angeles County, primarily in two neighborhoods – known by white residents as ghettos – Belvedere and the Macy Street District. In the Macy Street District, named for its southern boundary of Macy Street (now Cesar Chavez Avenue), roughly 3,000 residents were surrounded by the Los Angeles River, polluted by dead carcasses and brick, coal, gas and meatpacking plants. The rat population also thrived on the prevalence of horse and mule yards. Residents were crammed into one-fifth of a square mile, living in cramped residences with high rent despite low-quality living conditions. Residents often had to travel through someone's else's apartment to get to their own room. Despite often illegal living conditions, no investigations into the Macy District's living conditions was ever held, and the only four paved roads into the District were never inspected by the Department of Streets and Sanitation.[8][13]
Timeline
September 1924
On September 28, 1924, in the Macy Street District (present day Los Angeles Chinatown)[15] of Los Angeles, California, a 51-year-old man named Jesús Lajun fell ill with a fever and a painful lump in his groin. Prior to the onset of symptoms, Lajun had discovered a decaying rat under his house and picked it up, throwing it in the trash. The physician also misdiagnosed Lajun's pneumonic plague as a venereal disease (sexually transmitted infection), due to his enlarged lymph node. Even after the Los Angeles City Health Officers' confirmation of the disease as the pneumonic plague, the disease was referred as strange malady, pneumonia, virulent pneumonia, or malignant pneumonia until November 6. Investigators initially believed that Lajun contracted the bubonic plague. Left untreated, the bubonic plague can move to the lungs and cause a secondary pneumonic infection, with a mortality rate of 40–60%.[16] As Lajun's condition worsened, he developed extreme symptoms such as bloody sputum, causing doctors to believe it converted into pneumonic form. Because he was the first with identifiable symptoms of the plague, Lajun was designated the index patient.[3]
October 1924
In the same week, on October 3, 1924, Jesús Lajun's fifteen-year-old daughter Francisca also fell ill, complaining of fever and shortness of breath. Both also suffered from sore throats and back pain. Doctor Porter, a physician of the Los Angeles City Health Office, was called to the house and misdiagnosed Francisca with lobar pneumonia, a form of pneumonia weakening the lobe of a lung due to inflammatory exudate between alveoli.[17][18][19] Porter also misdiagnosed Lajun's plague as a venereal disease, or sexually transmitted infection, due to his enlarged lymph node. Following the Lajuns' diagnosis, they were treated by Lucina Samarano, a pregnant nurse.[20] Samarano lived at 742 Clara Street, which would become the eventual epicenter of the outbreak.[21]
However, neither of the Lajuns recovered; 15-year old Francisca died in an ambulance on its way to Los Angeles County General Hospital after her symptoms worsened. An autopsy of Lajun performed by physician Doctor Webb misdiagnosed her cause of death as double pneumonia. Jesús Lajun died on October 11, with his cause of death misdiagnosed as bronchopneumonia.[22]
Lucina Samarano developed similar respiratory symptoms and died days later on October 15. No autopsy was conducted on Samarano and she was yet again misdiagnosed with acute myocarditis, or inflammation of the heart muscle. [23][24] Samarano's fetus was stillborn and her body was returned to Guadalupe Samarano, her husband, infecting him.
Between October 15 and 19, Father M. Brualla, a Catholic priest who had administered last rites to the victims and held the requiem mass for Samarano, developed the same respiratory symptoms and died days later, as did several attendants of Samarano's funeral. Many of the Samaranos' friends and family were unknowingly infected by Guadalupe Samarano,[25] and within a week, the plague killed his entire family of eight.[1][26]
On October 22, Guadalupe and Jessie Flores, neighbors of the Samaranos, also fell ill with symptoms of the pneumonic plague and are subsequently hospitalized at the General Hospital. On October 24, doctors misdiagnosed the Flores with severe pneumonia as there was no known connection at the time between the Flores and Samaranos.[23]
On October 26, Guadalupe Flores died and received an autopsy by Doctor Lawrence Parsons, who also misdiagnoses his cause of death as double pneumonia. Therefore, no bacterial test was conducted to correctly identify the pathogen as Yersinia pestis, the causative agent of the pneumonic plague.[27] Flores' body was returned to his family on October 27, exposing their family to the pneumonic plague.[28] Afterwards, the hospital's morgue staff quarantined for five days.[29]
On October 28, physician George Stevens reported an unknown, highly contagious disease to the hospital and recommended the construction of a quarantine ward after he and Doctor Elmer Anderson both treated patients in unusually critical condition.[30] That same day, brothers Mike and Jose Jiminez also fell ill and vacated 742 Clara Street, the residence of the Samaranos, exposing the rest of the district to the plague.[28][30]
On October 29, several people who were in close contact with the Samaranos contracted the plague, including Mary Costello, Guadalupe Samarano's nurse; Fred Ortega, who lived at 742 Clara Street; Samarano's mother, Maria; and his brother, Victor. Maria and Victor Samarano were hospitalized under Doctor Bogen's supervision after exhibiting suspected symptoms of avian influenza. Jesus and Maria Valenzuela, cousins of the Samaranos, also fell ill with symptoms of the plague, though they were not traced back to the Samaranos. The Samaranos' children, Alfredo, Gilberto, Raul, and Roberto, along with six others, were hospitalized and diagnosed with meningitis, despite their skin turning black, a pathognomonic symptom of the plague.[28][31][32][33] A physician also requested an ambulance from the hospital for two patients in critical condition and were highly contagious.[4]
On October 30, the Los Angeles County Hospital pathologist Doctor George Maner finally identified the pneumonic plague as the disease causing the outbreak and notified the Los Angeles City Health Department and state officials. Maner identified it from a blood serum sample from a patient who died after attending Lucena Samarano's funeral. City health official quarantined an eight-block area encompassing Clara Street, where the funeral had taken place, as well as a six-block area in Belvedere after Jesús Lajun was identified as the index case, but did not announce the causative disease of the outbreak.[34] Thirteen more cases of an unknown disease were admitted, all of whom developed cyanosis and hemoptysis, or bloody sputum,[4] the former of which is indicative of low oxygen saturation of tissues near the skin surface.[35] Three of the patients died the same day, and in response the pneumonic plague was first suggested as the cause of the outbreak. The following morning, the diagnosis of pneumonic plague was confirmed by pathologists after an autopsy reported gram-negative bipolar staining bacilli resembling the plague.
Alexandre Yersin, the co-discoverer of Yersinia pestis, and the hospital's assistant superintendent sent a telegram ordering antiserum and vaccine on October 31, notifying the California Board of Health United States Public Health Service of the outbreak.[29] However, the antiserum requested was produced solely by the H.K. Mulford Company laboratories in Philadelphia, a 3,141-mile journey which would require automobile transport to Mineola, New York then a flight by mail plane to Los Angeles with a stopover in San Francisco. With cooperation from the United States Post Office Department and its respective air mail officials, it was prepared within an hour, according to the company.[4] In spite of the rapid deployment of the antiserum, it was successfully used on only two patients, Raul Samarano and Mary Costello, and remained largely unused for the rest of the outbreak.[3] Cumming subsequently commenced an investigation into the outbreak.[36]
The same day, County Health Commissioner J. L. Pomeroy imposed a quarantine, with 75 police officers and 200 armed World War I veterans deployed to assist quarantine guards in enforcing the quarantine,[37][38] who often looted from local residents and businesses.[39]
November 1924
On November 1, Benjamin Brown, a United States Public Health Service surgeon in Los Angeles, warned the United States Surgeon General Hugh S. Cumming[40] of the outbreak and Yersin's request for an antiserum. Brown's transmission was encoded, referring to "pneumonic plague" as "ekkil," "suspected cases" as "suspects," "deaths" as "begos," and "situation bad" as "ethos":[4]
Eighteen cases ekkil. Three suspects. Ten begos. Ethos. Recommend federal aid
Cumming then alerted Senior Surgeon James Perry, who was then stationed in San Francisco, to confidentially investigate the outbreak, attempting to avoid gratuitous involvement in state and municipal affairs.
10 more fatalities were recorded,[41] and Pomeroy extended the quarantine to encompass the entire Macy Street District,[37] purportedly to ensure that "Mexicans who we feared would scatter" couldn't evade the original quarantine.[42] The border's boundaries were closed to regular vehicle traffic and guards were positioned at every home with suspected cases.[42] Agricultural and railroad workers were exempted from the quarantine.[43] A temporary laboratory was constructed by the Los Angeles City Health Department in the quarantined area to quickly identify new cases. By this time, the cause of the outbreak had been definitively established as the pneumonic plague.[4]
Fatalities spiked yet again on November 2. Among them was Father Bruella, who oversaw the last rites of many of the plague victims in his ward and died from the plague at 9 a.m.[41] By this time, over 400 armed guards were deployed to implement the quarantine.[44][45] Despite its rapid spread, the outbreak remained largely unknown to the public – information that was released was often falsified or distorted, such as the Los Angeles Times, which attributed the quarantine to pneumonia, as opposed to newspapers on the East Coast which generally covered the outbreak without hesitation.[41]
By November 3, 24 people died over the course of two weeks,[lower-alpha 1] all but one of whom were Mexicans.[44] All Mexicans who died were required to undergo an autopsy even if it is not suspected that they died of the plague. Los Angeles authorities racially quarantined Mexican homes outside of the Macy Street District as well as majority African American, Chinese, and Japanese neighborhoods. The Macy Street District port mandated the inspection and fumigation of incoming ships while outgoing ships hung a yellow flag, indicating the ship originated in a quarantined zone.[46]
On November 4, 5 more died, bringing the total death toll to 29 (reported as 25 in local newspapers).[39]
On November 5, the plague antiserum requested by the Los Angeles County Hospital finally arrived, though it was only used on three patients. By this time, everyone else who lived at 742 Clara Street died. Despite a piling death toll, the hospital continued falsifying or contorting information regarding the outbreak.[39] A six-block quarantine was also imposed in Belvedere Gardens in response to two suspected plague deaths.[43]
By November 6, the death toll rose to 33 deaths (reported as 30 in local newspapers). That same day, El Heraldo de México became the first local newspaper to transparently report on the outbreak, revealing that the plague spread by rat fleas, not pneumonia, was its cause.[47] The newspaper also refuted city officials' claims that the plague outbreak began on October 30.[3] Consequently, the Port of Los Angeles began the eradication of all rats to avoid a quarantine and economic downturn.[43] The Los Angeles government advised those in the Macy Street District not to congregate by or heed to the newspaper.
On November 8, Los Angeles government and hospitals began the rollout of a vaccine. However, it would require the quarantined to leave the restricted area, meaning the vaccine was largely isolated to the sick. The plague vaccine at the time was also largely ineffective against the pneumonic plague, and in those who were vaccinated, the plague often progressed too far for the vaccine to be effective.[3][48]
On November 10, the Los Angeles County General Hospital superintendent, Doctor N. N. Wood, officially reported 9 clinically diagnosed plague cases after weeks of silence on the plague, which was adjusted to 37 on November 11.[3]
On November 13, the quarantine was lifted after 6 days of no new cases.[3]
On November 14, a man named Martin Hernandez, who did not live anywhere near the Macy Street District, died of the plague; his case was not reported to any authorities.[3]
On November 15, the plague was officially declared over by local health officials in spite of lingering active cases of the plague,[3] allowing the introduction of a citywide rat extermination program.[49]
Epidemiology and pathology
Transmission
The pneumonic plague is the only form of the plague capable of person-to-person transmission, which occurs during droplet-respiration, or breathing, as opposed to other forms of the plague.[50][51] The 1924 Los Angeles pneumonic plague outbreak was the last instance of aerosol transmission of the plague in the United States.[10] A person is infected when they breathe in particles of Yersinia pestis, a bacterium transmitted by rat fleas, in the air. Alternatively, if the bubonic plague (another form of the plague) goes untreated, the bacteria can spread to the lungs through the bloodstream and cause a secondary case of the pneumonic plague.[52] Between 1900 and 2009, there were 1,001 reported cases of pneumonic plague, of which 81% occurred before 1943, when effective antibiotics, such as doxycycline, ciprofloxacin, and levofloxacin[52][51] became widely available.[53] In that time period, 92% of cases were fatal.[8]
The pneumonic plague's potency of person-to-person transmission is disputed[54] – it is agreed that Yersinia pestis can spread the pneumonic plague through aerosol transmission of infected droplets, and the bacterium can survive in the air for up to one hour in optimum conditions. Somebody exposed to someone infected with the pneumonic plague can fall ill within 1 to 6 days.[52] However, Jacob L. Kool objects to the supposed high risk of person-to-person transmission in an article titled ""Risk of Person‐to‐Person Transmission of Pneumonic Plague" in Clinical Infectious Diseases, stating that people are only at risk of exposure to the plague when the disease has progressed to its end stage and the infected begin coughing bloody sputum.[50] Even then, direct and close contact within six feet is required for the plague to spread, according to the Centers for Disease Control and Prevention's National Center for Emerging and Zoonotic Infectious Diseases.[51] Transmission can be prevented by tight-fitting surgical masks and social distancing.[52] Only 11% of patients that contracted the disease actually spread it to another person.[8]
After the 1924 outbreak in Los Angeles, there have been no secondary transmissions (transmission of the disease from a secondary case).[8] Bodily fluids and tissue of an infected animal can still transmit the plague to humans through direct contact if handled improperly, but this is exceedingly rare: today, the World Health Organization reports only 1,000 to 3,000 cases of the plague annually.[52] Zoonosis is often the direct result of an epizootic, a flare-up of a disease in animals analogous to a human epidemic. Though the plague is most common in rural and semi-arid regions of the western United States, epizootics are frequent among rodents in big cities and urban areas with large, diverse specimen populations, as exemplified in this outbreak, the last urban plague epizootic.[10]
Signs and symptoms
The pneumonic plague primarily affects the lungs, and common symptoms include fatigue, fever, and pneumonia, the latter of which in turn can cause chest pain, coughing, hemoptysis (bloody sputum), and shortness of breath. The plague may also cause abdominal pain, nausea, and vomiting. If antibiotic treatments, which were not available until 1943,[53] are not administered within 24 hours of the onset of symptoms, the plague will often progress into respiratory failure, shock, and death.[52]
Diagnosis
The pneumonic plague is diagnosed after evaluation by a healthcare worker and a laboratory test of the patient's blood, lymph node aspirate, or sputum confirms infection.[52]
Treatment
The plague can be treated with a therapeutic antiserum, a treatment first initiated in 1896 by Alexandre Yersin, a bacteriologist, physician, and co-discoverer of Yersinia pestis as the causative bacterium of the plague. The efficacy of antiserum is disputed but it is generally accepted to be successful in mitigating negative effects of the plague: the mortality rates for antiserum-treated patients was 35%, as opposed to 82% for untreated patients.[55]
In the 1924 Los Angeles outbreak, the serum was only successfully used on two patients, Mary Costello and Raul Samarano, remaining largely unused.[3] At the time, it was only produced by H.K. Mulford Company laboratories in Philadelphia, Pennsylvania, but was quickly flown the 3,141-mile route via car to Mineola, New York then flown on air mail to Los Angeles via San Francisco.[4]
Response
Initial medical response and concealment
The government of Los Angeles consistently ensured that the pneumonic plague outbreak never became public. On October 29, Yersinia pestis, the bacterium causing the plague, was found in the lungs of a plague victim, a finding not released to the public until after the outbreak. As cases piled up, a telegram sent on October 31 recommended federal aid for the city of Los Angeles, replacing the terms "pneumonic plague," "death," and "situation" with code "ekkil," "begos," and "ethos," respectively.[4] Government officials knew the outbreak was attributed to the pneumonic plague well before October 30, when it was first labeled in official government documents. Secretary of the State Board of Health Doctor Walter Dickie conducted a test on a guinea pig with a lymph node sample taken from Jesus Lajun before he died. The guinea pig died from the pneumonic plague, yet it took 17 days for an announcement confirming the outbreak was the fault of the plague.[37]
In spite of significant delays in medical announcements, significant preventative measures were still enacted: a quarantine of the eight blocks surrounding Jesús Lajun's residence was quickly imposed, affecting roughly 2,500 residents, most of whom were Mexican immigrants. Medical personnel traveled to each house inspecting residents for signs and symptoms of the plague.[4]
Two years following the outbreak's conclusion, Dickie reported to Governor of California Friend W. Richardson commending the response to the outbreak as "the most outstanding accomplishment" of the year, which was questioned as "historical drift" by Arthur J. Viseltear in a 1974 article published in Yale Journal of Biology and Medicine.[4]
Media coverage
Los Angeles media coverage of the plague was considered vague compared to that of media outside of the city, often attributing the outbreak to pneumonia, as seen in a subheading in the Los Angeles Examiner reading "Officials Believe Virulent Pneumonia Outbreak Controlled" and a headline in the Los Angeles Times reading "Seven are Dead from Pneumonia," both of which published on November 3.[4][56] The plague was not referred to by name until November 6, by which time the plague was practically over. Many Los Angeles newspapers also incorrectly depicted Belvedere Gardens and the Macy Street District, both heavily populated by Mexican immigrants, as separate from the City of Los Angeles.[43] Any news reports that did refer to the outbreak by name often portrayed Mexican Americans and their respective neighborhoods as 'menaces.'[57]
By comparison, The New York Times and The Washington Post both referred to the plague by name, even comparing it to the Black Death of the 14th century. Several newspapers outside of Los Angeles covered the deployment of the plague antiserum in early November in detail, including the Chicago Tribune; The Evening World; Herald & Review; The Indianapolis Times; Moon-Journal of Battle Creek, Michigan; New York World; The Philadelphia Bulletin; The Philadelphia Inquirer; The Philadelphia North American; Public Ledger; San Francisco Daily News; and the San Francisco Evening Bulletin.[4]
Racism
The city's handling of the outbreak reinforced the widespread stereotype that Mexicans were poor and of a degraded class. Due to cramped and often illegal living conditions, rats were prevalent in majority Hispanic neighborhoods, cultivating the belief that the plague was an ethnic trait, as exemplified in a University of California, Los Angeles professor who claimed that Mexicans have a tendency to "huddle together" and therefore spread disease.[58]
Institutional racism and poverty also advanced the spread of the plague, as overcrowding, poor ventilation, poor sanitization, and high rodent populations often exacerbate the spread and harshness of the plague.[33][54][59][60] In 1924, Mexican immigrants made up the largest ethnic group living in often dense and unsafe work camps, which flourished under widespread sentiment against Mexican immigrants and workers. Employment discrimination was also frequent as Mexicans were viewed as cheap and expendable, and many perceived Mexican Americans being relegated to working in factories and agricultural fields enclosing Los Angeles.[61] On November 9, 200 Mexican workers at the Biltmore Hotel, most of whom did not live in the Macy Street District, were rehired after previously and controversially being fired.[3] Several Mexican residents believed that quarantine guards and the over 200 armed veterans enforcing the quarantine were holding them against their will.[57] Mexican men often had to convert from Catholicism to Protestantism to be respected, while Mexican women were societally obligated to be trained in proper housekeeping.[62] These racist sentiments were possibly the fault of the misdiagnosis of Jesus Lajun's cause of death as a sexually transmitted infection[3] and bronchopneumonia.[22]
After the plague, health officials recognized the need for programs encouraging safe hygiene practices among the Mexican population. Health officials blamed the plague outbreak on Mexicans' supposed ignorance of proper hygiene, despite actually being the fault of notoriously inferior living conditions and poverty in the Macy Street District. Some health officials even blamed the outbreak itself entirely on Mexican Americans, which Feldinger argues reinforced the pro-segregation views widely held at the time.[63] The response also failed to provide vital access to clean water and sanitary disposal.[43]
Rat extermination
After the 1900–1904 San Francisco bubonic plague outbreak, squirrels carrying fleas with the Yersinia pestis bacteria were found all throughout California. At the time, it was widely believed that rodents or small animals were directly responsible for spreading the plague, rather than fleas .[9] In response, the City of Los Angeles hired people to systematically eradicate or tag rodents, primarily targeting squirrels.[4]
Following the Los Angeles outbreak, the City of Los Angeles began a citywide rat and ground squirrel extermination program. On November 15, Doctor Walter Dickie announced an ordinance requiring Los Angeles residents to maintain a clean household. Violations could result in the destruction of said private property, a consequence that devastated Mexicans. A committee dedicated to the eradication of rats received $250,000 in funding between November 1924 and July 1925 and $500,000 between July 1925 and July 1926. The city established a rat bounty and infected rats were found Downtown, in Beverly Hills, and at the harbor. The city lifted houses 18 inches above the ground and ripped off their siding to allow stray cats and dogs to eat infected rats. Buildings were also sprayed with hydrogen cyanide, rodenticide, and sulfur. Health officials also burned lumber, clothing, and garbage.[49][64]
Today, only 5 to 15 cases of the plague are reported annually in the western United States, and naturally occurring pneumonic plague is practically nonexistent.[10][52]
See also
- Airborne transmission
- Bubonic plague
- Septicemic plague
- Super-spreader
- Outbreak
- Epidemic
- Zoonosis
- Black rat
Notes
- ↑ Reported as 21 deaths in newspapers at the time due to the misdiagnoses of the Lajuns and Lucina Samarano.
References
- 1 2 3 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 9–10. ISBN 978-1-56343-885-1.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 51. ISBN 978-1-56343-885-1.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 124–130. ISBN 978-1-56343-885-1.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Viseltear, AJ (February 28, 1974). "The pneumonic plague epidemic of 1924 in Los Angeles". The Yale Journal of Biology and Medicine. 47 (1): 40–54. PMC 2595158. PMID 4596466.
- ↑ Jacob L. Kool. Risk of Person to Person Transmission of Pneumonic Plague. Clin. Infect. Dis. (2005) 40 (8): 1166-1172.
- ↑ "CDC - Maps & Statistics - Plague". CDC.gov. 2013-04-23. Retrieved 2013-07-30.
- ↑ Martin Helen Eastman, The History of Los Angeles County Hospital, 1878–1968; and the Los Angeles County University of Southern California Medical Center 1969–1978. (Los Angeles: University of Southern California Press, 1979) 5–7.
- 1 2 3 4 5 6 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 17–19. ISBN 978-1-56343-885-1.
- 1 2 Anderson, Elizabeth T. (1974). "Plague in the Continental United States, 1900-76". Public Health Reports. 93 (3): 297–301. PMC 1431896. PMID 349602.
- 1 2 3 4 "Ecology and Transmission | Plague". Centers for Disease Control and Prevention National Center for Emerging and Zoonotic Infectious Diseases. July 31, 2019. Retrieved January 1, 2021.
{{cite web}}: CS1 maint: url-status (link) - ↑ Weise, Elizabeth (July 26, 2013). "Why you don't need to worry about getting the plague". USA Today. Retrieved January 2, 2021.
{{cite web}}: CS1 maint: url-status (link) - ↑ "US Census Bureau Publications - Census of Population and Housing". United States Census Bureau. United States Census Bureau Administration and Customer Services Division. Retrieved January 7, 2021.
{{cite web}}: CS1 maint: others (link) CS1 maint: url-status (link) - ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 20–21. ISBN 978-1-56343-885-1.
- ↑ Feldinger, Frank. (2008). A slight epidemic : the government cover-up of black plague in Los Angeles : what happened and why it matters (1st ed.). Los Angeles, CA: Silver Lake Pub. ISBN 978-1-56343-885-1. OCLC 191727582.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague: What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 135. ISBN 978-1-56343-885-1.
- ↑ Dufel, Susan E. (April 18, 2017). "CBRNE - Plague: Background, Pathophysiology, Epidemiology" – via Medscape.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease. St. Louis, Mo: Elsevier Saunders. p. 749. ISBN 0-7216-0187-1.
- ↑ "What is Lobar Pneumonia?". AAPC Knowledge Center. February 11, 2020. Retrieved December 31, 2020.
{{cite web}}: CS1 maint: url-status (link) - ↑ "Pneumonia - Symptoms and causes". Mayo Clinic. Retrieved December 31, 2020.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 11–12. ISBN 978-1-56343-885-1.
- ↑ "742 Clara Street. Focus of outbreak". Online Archive of California. University of California Berkeley, Bancroft Library. 1988. Retrieved 31 December 2020.
{{cite web}}: CS1 maint: others (link) CS1 maint: url-status (link) - 1 2 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 13. ISBN 978-1-56343-885-1.
- 1 2 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 25–26. ISBN 978-1-56343-885-1.
- ↑ "Myocarditis - Symptoms and causes". Mayo Clinic. Retrieved December 31, 2020.
{{cite web}}: CS1 maint: url-status (link) - ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 25–26. ISBN 978-1-56343-885-1.
- ↑ Cecilia Rasmussen "Los Angeles Then and Now," March 5, 2006, The Los Angeles Times.
- ↑ "Plague". Centers for Disease Control and Prevention. July 23, 2020. Retrieved December 31, 2020.
{{cite web}}: CS1 maint: url-status (link) - 1 2 3 Deverell, William (2004). Whitewashed Adobe: The Rise of Los Angeles and the Remaking of Its Mexican Past. United States of America: University of California Press. pp. 155–158. ISBN 9780520932531.
- 1 2 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 28–30. ISBN 978-1-56343-885-1.
- 1 2 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 45–46. ISBN 978-1-56343-885-1.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 46–48. ISBN 978-1-56343-885-1.
- ↑ "Symptoms of plague | CDC". Centers for Disease Control and Prevention. November 27, 2018. Retrieved December 31, 2020.
- 1 2 "Plague - Symptoms and causes". Mayo Clinic. Retrieved December 31, 2020.
{{cite web}}: CS1 maint: url-status (link) - ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 51. ISBN 978-1-56343-885-1.
- ↑ Adeyinka, Adebayo; Kondamundi, Noah P. (September 22, 2020). "Cyanosis". National Center for Biotechnology Information Bookshelf. National Center for Biotechnology Information at the National Library of Medicine. PMID 29489181. NBK482247. Retrieved January 7, 2021.
{{cite journal}}: CS1 maint: url-status (link) - ↑ Feldinger, Fred (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 52–53. ISBN 978-1-56343-885-1.
- 1 2 3 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 56–57. ISBN 978-1-56343-885-1.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 82. ISBN 978-1-56343-885-1.
- 1 2 3 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 115–117. ISBN 978-1-56343-885-1.
- ↑ "Previous Surgeons General". Department of Health and Human Services. Office of the Surgeon General. December 14, 2017. Retrieved December 31, 2020.
{{cite web}}: CS1 maint: others (link) CS1 maint: url-status (link) - 1 2 3 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 84–85. ISBN 978-1-56343-885-1.
- 1 2 Deverell, William (2004). Whitewashed Adobe: The Rise of Los Angeles and the Remaking of Its Mexican Past. United States of America: University of California Press. pp. 161–163. ISBN 9780520932531.
- 1 2 3 4 5 Molina, Natalia (2006). Fit to be a Citizens?: Public Health and Race in Los Angeles, 1879-1939. American Crossroads Ser. Vol. 20 (1 ed.). United States of America: University of California Press. pp. 76–80. ISBN 9780520939202.
- 1 2 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 86–87. ISBN 978-1-56343-885-1.
- ↑ Deverell, William (2004). Whitewashed Adobe: The Rise of Los Angeles and the Remaking of Its Mexican Past. United States of America-: University of California Press. pp. 164–167. ISBN 9780520932531.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 92. ISBN 978-1-56343-885-1.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 120. ISBN 978-1-56343-885-1.
- ↑ Bubeck, Sarah S.; Dube, Peter H. (July 25, 2007). "Yersinia pestis CO92ΔyopH Is a Potent Live, Attenuated Plague Vaccine". Clinical and Vaccine Immunology. American Society for Microbiology. 14 (9): 1235–1238. doi:10.1128/CVI.00137-07. ISSN 1556-6811. PMC 2043315. PMID 17652523.
- 1 2 Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 132–133. ISBN 978-1-56343-885-1.
- 1 2 Kool, Jacob L.; A. Weinstein, Robert (15 April 2005). "Risk of Person‐to‐Person Transmission of Pneumonic Plague". Clinical Infectious Diseases. 40 (8): 1166–1172. doi:10.1086/428617. PMID 15791518 – via Oxford Academic.
- 1 2 3 "Human Plague: Transmission from Person to Person" (PDF). Centers for Disease Control and Prevention. National Center for Emerging and Zoonotic Infectious Diseases, Division of Vector-borne Diseases. Retrieved January 1, 2021.
{{cite web}}: CS1 maint: others (link) CS1 maint: url-status (link) - 1 2 3 4 5 6 7 8 "Frequently Asked Questions (FAQ) About Plague". Centers for Disease Control and Prevention Emergency Preparedness and Response. April 4, 2018. Retrieved January 1, 2021.
{{cite web}}: CS1 maint: url-status (link) - 1 2 Hinckley, A. F.; Biggerstaff, B. J.; Griffith, K. S.; Mead, P. S. (7 July 2011). "Transmission Dynamics of primary pneumonic plague in the USA". Epidemiology and Infection (published March 2012). 140 (3): 554–560. doi:10.1017/S0950268811001245. PMID 21733272 – via Cambridge University Press.
- 1 2 Greninger, Alex (2004). The Definition and Measurement of Dangerous Research; Pneumonic Plague. Center for International & Security Studies. pp. 31–50.
- ↑ Butler, T. (March 2014). "Plague history: Yersin's discovery of the causative bacterium in 1894 enabled, in the subsequent century, scientific progress in understanding the disease and the development of treatments and vaccines". Clinical Microbiology and Infection. 20 (3): 202–209. doi:10.1111/1469-0691.12540. ISSN 1198-743X. PMID 24438235 – via Elsevier ScienceDirect.
- ↑ Feldinger, Frank (2008). A Slight Epidemic: The Government Cover-up of the Black Plague in Los Angeles. United States of America: Silver Lake Publishing. pp. 19. ISBN 978-1-56343-885-1.
- 1 2 Rasmussen, Cecilia (March 5, 2006). "In 1924 Los Angeles, a Scourge from the Middle Ages". Los Angeles Times. Retrieved November 13, 2020.
{{cite web}}: CS1 maint: url-status (link) - ↑ Deverell, William (2004). Whitewashed Adobe: The Rise of Los Angeles and the Remaking of its Mexican Past. United States of America: University of California Press. pp. 179–180. ISBN 9780520932531.
- ↑ Murrell, Daniel (January 3, 2018). "The Plague: Types, Causes & Symptoms". Healthline. Retrieved January 3, 2021.
{{cite web}}: CS1 maint: url-status (link) - ↑ Rabaan, Ali A.; Al-Ahmed, Shamsah H.; Alsuliman, Shahab A.; Aldrazi, Fatimah A.; Alfouzan, Wadha A.; Haque, Shafiul (March 2019). "The rise of pneumonic plague in Madagascar: current plague outbreak breaks usual seasonal mould". Journal of Medical Microbiology. United States National Library of Medicine at the National Institutes of Health (published January 11, 2019). 68 (3): 292–302. doi:10.1099/jmm.0.000915. ISSN 1473-5644. PMID 30632956 – via PubMed.
- ↑ "THE 1920S TO THE GREAT DEPRESSION: Mexican Farm Workers' Strike in Corcoran, California". Omeka.
- ↑ Monroy, Douglas (1983). "Like Swallows at the Old Mission: Mexicans and the Racial Politics of Growth in Los Angeles in the Interwar Period". The Western Historical Quarterly. 14 (4): 435–458. doi:10.2307/968200. JSTOR 968200.
- ↑ Feldinger, Frank (2007). A Slight Epidemic: The Government Cover-Up of the Black Plague in Los Angeles What Happened and Why it Matters. United States of America: Silver Lake Publishing. pp. 30–31. ISBN 978-1-56343-885-1.
- ↑ Deverell, William (2004). Whitewashed Adobe The Rise of Los Angeles and the Remaking of Its Mexican Past. United States of America: University of California Press. pp. 164–169. ISBN 9780520932531.
External links
- Facts about Pneumonic Plague. Centers for Disease Control and Prevention.