Lisfranc injury
| Lisfranc injury | |
|---|---|
| Other names: Lisfranc fracture, Lisfranc dislocation, Lisfranc fracture dislocation, tarsometatarsal injury, midfoot injury | |
 | |
| An X-ray of a Lisfranc injury showing widening between the 1st and 2nd metatarsal base. | |
| Specialty | Orthopedics |
| Symptoms | Swelling, pain, and bruising of the midfoot[1][2] |
| Complications | Arthritis, chronic pain[1] |
| Types | Homolateral, divergent, isolated[3] |
| Causes | Injury[2] |
| Diagnostic method | X-ray or CT scan[4] |
| Treatment | Open reduction and internal fixation[4] |
| Prognosis | Healing may take months[2] |
| Frequency | Relatively uncommon[1] |
Lisfranc injury, also known as Lisfranc fracture, is an injury of the foot involving the joints between the metatarsal bones and tarsus bones.[1][2] Symptoms may include swelling, pain, and bruising of the midfoot.[2][1] Symptoms are worsened by attempts to walk.[2] Without treatment complications may include arthritis and chronic pain.[1]
The cause may include twisting the foot, such as when playing sports, or more severe injuries such as a fall from heights.[2] Generally it occurs in people without specific risk factors, though those with diabetes are more commonly affected.[1] Diagnosis is by X-ray when weight bearing or CT scan.[4] The diagnosis should be suspected if midfoot pain lasts more than 5 days.[1]
Initial treatment may involved reduction, splinting, and keeping the foot elevated.[1] If the injury is unstable or displaced, surgery in the form of an open reduction and internal fixation is generally recommended.[4][1] Healing may take months.[2]
Lisfranc injuries are relatively uncommon, representing about 0.2% of fractures.[1] Middle aged males are most commonly affected.[1] It is named after Jacques Lisfranc de St. Martin, a French surgeon who noticed the injury among cavalry in 1815, following the War of the Sixth Coalition.[5][2]
Signs and symptoms

Symptoms may include swelling, pain, and bruising of the foot.[2] Symptoms are worsened by attempts to walk.[2]
Causes
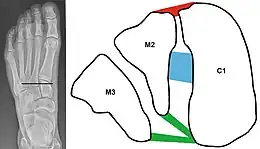
C1 = Medial cuneiform
M2 = 2nd metatarsal base
M3 = 3rd metatarsal base
Red = dorsal Lisfranc ligament
Blue = interosseous Lisfranc ligament
Green = plantar Lisfranc ligament.
The midfoot consists of five bones that form the arches of the foot (the cuboid, navicular, and three cuneiform bones) and their articulations with the bases of the five metatarsal bones, and these articulations are damaged in a Lisfranc injury. Such injuries typically involve the ligaments between the medial cuneiform bone and the bases of the second and third metatarsal bones, and each of these ligaments is called Lisfranc ligament.[6]
Lisfranc injuries are caused when excessive kinetic energy is applied either directly or indirectly to the midfoot and are often seen in traffic collisions or industrial accidents.[7]
Direct Lisfranc injuries are usually caused by a crush injury, such as a heavy object falling onto the midfoot, or the foot being run over by a car or truck, or someone landing on the foot after a fall from a significant height.[8] Indirect Lisfranc injuries are caused by a sudden rotational force on a plantar flexed (downward pointing) forefoot.[7] Examples of this type of trauma include a rider falling from a horse but the foot remaining trapped in the stirrup, or a person falling forward after stepping into a storm drain.[8]
In athletic trauma, Lisfranc injuries occur commonly in activities such as windsurfing, kitesurfing, wakeboarding, or snowboarding (where appliance bindings pass directly over the metatarsals).[9] American football players occasionally acquire this injury, and it most often occurs when the athlete's foot is plantar flexed and another player lands on the heel. This can also be seen in pivoting athletic positions such as a baseball catcher or a ballerina spinning.
Diagnosis
In a high energy injury to the midfoot, such as a fall from a height or a motor vehicle accident, the diagnosis of a Lisfranc injury should, in theory at least, pose less of a challenge. There will be deformity of the midfoot and X-ray abnormalities should be obvious. Further, the nature of the injury will create heightened clinical suspicion and there may even be disruption of the overlying skin and compromise of the blood supply. Typical X-ray findings would include a gap between the base of the first and second toes.[10] The diagnosis becomes more challenging in the case of low energy incidents, such as might occur with a twisting injury on the racquetball court, or when an American Football lineman is forced back upon a foot that is already in a fully plantar flexed position. Then, there may only be complaint of inability to bear weight and some mild swelling of the forefoot or midfoot. Bruising of the arch has been described as diagnostic in these circumstances but may well be absent.[11] Typically, conventional radiography of the foot is utilized with standard non-weight bearing views, supplemented by weight bearing views which may demonstrate widening of the interval between the first and second toes, if the initial views fail to show abnormality. Unfortunately, radiographs in such circumstances have a sensitivity of 50% when non-weight bearing and 85% when weight bearing, meaning that they will appear normal in 15% of cases where a Lisfranc injury actually exists.[12] In the case of apparently normal x-rays, if clinical suspicion remains, advanced imaging such as magnetic resonance imaging (MRI) or computed tomography (CT scan) is a logical next step.[13]
 Lisfranc fracture (marked by the oval). This case also has fractures of the distal second (marked by the arrow), third, and fourth metatarsal bones.
Lisfranc fracture (marked by the oval). This case also has fractures of the distal second (marked by the arrow), third, and fourth metatarsal bones. Lisfranc dislocation of the left foot due to lisfranc ligament rupture as seen on bilateral weight bearing radiographs.[1]
Lisfranc dislocation of the left foot due to lisfranc ligament rupture as seen on bilateral weight bearing radiographs.[1]
Classification
There are three classifications for the fracture:[14]
- Homolateral: All five metatarsals are displaced in the same direction. Lateral displacement may also suggest cuboidal fracture.
- Isolated: one or two metatarsals are displaced from the others.
- Divergent: metatarsals are displaced in a sagittal or coronal plane and may also involve the intercuneiform area and include a navicular fracture.
Treatment
Options include operative or non-operative treatment. One study claims that in athletes, and if the dislocation is less than 2 mm, the fracture can be managed with casting for six weeks.[15] The person's injured limb cannot bear weight during this period. In the majority of cases early anatomical reduction and stable fixation is indicated.[16] A 2005 study suggests that closed reduction and Kirschner wire (K-wire) stabilisation or open reduction and stabilisation - generally using screws to avoid the complication of K-wires and maintain a stable reduction - are the treatments of choice.[16]
According to a 1997 study, for severe Lisfranc injuries, open reduction with internal fixation (ORIF) and temporary screw or Kirschner wire fixation is the treatment of choice.[17] The foot cannot be allowed to bear weight for a minimum of six weeks. Partial weight-bearing may then begin, with full weight bearing after an additional several weeks, depending on the specific injury. K-wires are typically removed after six weeks, before weight bearing, while screws are often removed after 12 weeks.[17]
When a Lisfranc injury is characterized by significant displacement of the tarsometatarsal joint(s), nonoperative treatment often leads to severe loss of function and long-term disability secondary to chronic pain and sometimes to a planovalgus deformity. In cases with severe pain, loss of function, or progressive deformity that has failed to respond to nonoperative treatment, mid-tarsal and tarsometatarsal arthrodesis (operative fusion of the bones) may be indicated.[18]
History
During the Napoleonic Wars, Jacques Lisfranc de St. Martin encountered a soldier who suffered from vascular compromise and secondary gangrene of the foot after a fall from a horse.[5] Subsequently, Lisfranc performed an amputation at the level of the tarsometatarsal joints,[5] and that area of the foot has since been eponymously referred to as the "Lisfranc joint".[19] Although Lisfranc did not describe a specific mechanism of injury or classification scheme, a Lisfranc injury has come to mean a dislocation or fracture-dislocation injury at the tarsometatarsal joints.[20]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Buchanan, BK; Donnally III, CJ (January 2021). "Lisfranc Dislocation". PMID 28846306.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 3 4 5 6 7 8 9 10 11 "Lisfranc (Midfoot) Injury - OrthoInfo - AAOS". www.orthoinfo.org. Archived from the original on 19 March 2021. Retrieved 9 March 2021.
- ↑ Gaillard, Frank. "Lisfranc injury". Radiopaedia. Radiopaedia.org. Archived from the original on 21 October 2020. Retrieved 9 March 2021.
- 1 2 3 4 "Fracture-Dislocation of the Midfoot (Lisfranc Injury) - Injuries; Poisoning". Merck Manuals Professional Edition. Archived from the original on 16 May 2021. Retrieved 9 March 2021.
- 1 2 3 Lisfranc, J (1815). Nouvelle méthode opératoire pour l'amputation partielle du pied dans son articulation tarso-métatarsienne: méthode précédée des nombreuses modifications qu'a subies celle de Chopart (in français). Paris: L’imprimerie de Feuguery. pp. 1–52. Archived from the original on 2021-08-28. Retrieved 2020-11-01.
- 1 2 Rettedal, David D; Graves, Nathan C; Marshall, Joshua J; Frush, Katherine; Vardaxis, Vassilios (2013). "Reliability of ultrasound imaging in the assessment of the dorsal Lisfranc ligament". Journal of Foot and Ankle Research. 6 (1): 7. doi:10.1186/1757-1146-6-7. ISSN 1757-1146. PMC 3626864. PMID 23453037.
- 1 2 Smith BR, Begeman PC, Leland R, Meehan R, Levine RS, Yang KH, King AI (2005). "A Mechanism of Injury to the Forefoot in Car Crashes". Traffic Injury Prevention. 6 (2): 156–69. doi:10.1080/15389580590931635. ISSN 1538-9588. PMID 16019401. S2CID 35856985.
- 1 2 Chan, SCF; Chow, SP (2001). "Current concept review on Lisfranc injuries" (PDF). Hong Kong Journal of Orthopaedic Surgery. 5 (1): 75–80. Archived from the original (PDF) on 2016-03-04. Retrieved 2012-06-05.
- ↑ Lievers WB, Frimenko RE, McCullough KA, Crandall JR, Kent RW (2015). "Etiology and biomechanics of midfoot (Lisfranc) injuries in athletes". Critical Reviews in Biomedical Engineering. 43 (2–3): 213–238. doi:10.1615/CritRevBiomedEng.v43.i2-3.60. PMID 27278743.
- ↑ Davies MS, Saxby TS (September 1999). "Intercuneiform instability and the "gap" sign". Foot Ankle Int. 20 (9): 606–9. doi:10.1177/107110079902000912. PMID 10509690. S2CID 33610199.
- ↑ Ross G, Cronin R, Hauzenblas J, Juliano P (1986). "Plantar ecchymosis sign: a clinical aid to diagnosis of occult Lisfranc tarsometatarsal injuries". J Orthop Trauma. 10 (2): 119–122. doi:10.1097/00005131-199602000-00008. PMID 8932671.
- ↑ Rankine JJ, Nicholas CM, Wells G, Barron DA (April 2012). "The diagnostic accuracy of radiographs in Lisfranc injury and the potential value of a craniocaudal projection". AJR Am J Roentgenol. 198 (4): W365–9. doi:10.2214/AJR.11.7222. PMID 22451574.
- ↑ Hatem SF (November 2008). "Imaging of Lisfranc Injury and Midfoot Sprain". Radiologic Clinics of North America. 46 (6): 1045–1060. doi:10.1016/j.rcl.2008.09.003. PMID 19038612.
- ↑ Wheeless CR (2011). "Lisfranc's Fracture / TarsoMetatarsal Injuries". Wheeless' Textbook of Orthopaedics online. Durham, North Carolina: Duke Orthopaedics. Archived from the original on 2012-07-02. Retrieved 2012-06-05.
- ↑ Lattermann C, Goldstein JL, Wukich DK, Lee S, Bach BR Jr (July 2007). "Practical management of Lisfranc injury in athletes". Clin J Sport Med. 17 (4): 311–51. doi:10.1097/JSM.0b013e31811ed0ba. PMID 17620787. S2CID 41073329.
- 1 2 Makwana, Nilesh (2005). "Tarsometatarsal injuries—Lisfranc injuries" (PDF). Current Orthopaedics. 19: 108–118. doi:10.1016/j.cuor.2004.12.008.
{{cite journal}}: CS1 maint: url-status (link) - 1 2 Mulier, T; Reynders, P; Sioen, W; Van Den Bergh, J; De Reymaeker, G; Reynaert, P; Broos, P (1997). "The Treatment of Lisfranc Injuries" (PDF). Acta Orthopaedica Belgica. 63 (2): 82–90. ISSN 0001-6462. PMID 9265792. Archived from the original (PDF) on 2013-11-05.
- ↑ Mann, RA; Prieskorn, D; Sobel, M (1996). "Mid-tarsal and tarsometatarsal arthrodesis for primary degenerative osteoarthrosis or osteoarthrosis after trauma". Journal of Bone and Joint Surgery. American Volume. 78 (9): 1376–85. doi:10.2106/00004623-199609000-00013. PMID 8816654. S2CID 20769992. Archived from the original on 2012-12-13. Retrieved 2012-06-06.
- ↑ Lisfranc's joint at Who Named It?
- ↑ DiDomenico, LA; Cross, D (2012). "Tarsometatarsal/Lisfranc Joint" (PDF). Clinics in Podiatric Medicine and Surgery. 29 (2): 221–42. doi:10.1016/j.cpm.2012.01.003. PMID 22424486. Archived from the original (PDF) on 2016-03-04. Retrieved 2012-06-05.
External links
| External resources |
|---|