Hematuria
| Hematuria | |
|---|---|
| Other names: Haematuria, erythrocyturia,[1] blood in the urine | |
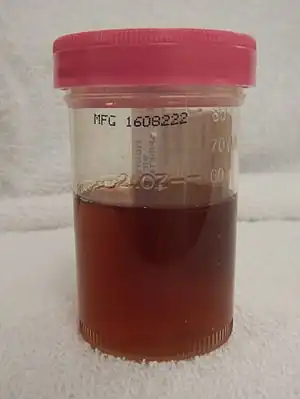 | |
| Visible hematuria | |
| Specialty | Nephrology, urology |
| Types | Microscopic, visible[2] |
| Causes | Glomerular: Nephrotic syndrome, membranoproliferative glomerulonephritis, IgA nephropathy, Alport syndrome[2] Non glomerular: Urinary tract infections, prostatitis, fever, cancer, kidney stones, exercise, and bleeding problems.[2] |
| Diagnostic method | Urinalysis, urine microscopy, medical imaging, cystoscopy, kidney biopsy[2] |
| Differential diagnosis | Vaginal bleeding, gastrointestinal bleeding, certain medication or foods[3] |
| Treatment | Depends on cause[2] |
| Frequency | Common[2] |
Hematuria is defined as the presence of blood, specifically red blood cells, in the urine.[4][2] Pain may or may not be present.[2] Blood clots may also occur in the urine.[2]
Causes are divided into whether or not the glomerulus of the kidney is involved.[2] Those that involve the glomerulus include nephrotic syndrome, membranoproliferative glomerulonephritis, Alport syndrome, and IgA nephropathy.[2] Causes that do not involve the glomerulus include urinary tract infections, prostatitis, fever, cancer, kidney stones, exercise, and bleeding problems.[2] Other conditions that can be mistaken for blood in the urine include vaginal bleeding, gastrointestinal bleeding, and certain medication or foods that turn the urine red.[3]
Diagnosis generally begins with a urinalysis which may be supported by urine microscopy.[2] The presence of protein in the urine or misshapen red blood cells may indicate glomerular involvement.[2] Medical imaging may be useful for picking up kidney stones, cysts, or masses.[2] Cystoscopy may be useful for picking up bladder cancer.[2][5] A kidney biopsy may be useful in those with a glomerular cause.[2]
Treatment depends on the underlying cause.[2] This may vary from observation for those with blood in the urine that comes and goes, with no other symptoms, and otherwise normal investigations.[2] To interventional radiology to embolize significant bleeding.[2] Blood in the urine is a common reason people seek health care.[2]
Causes
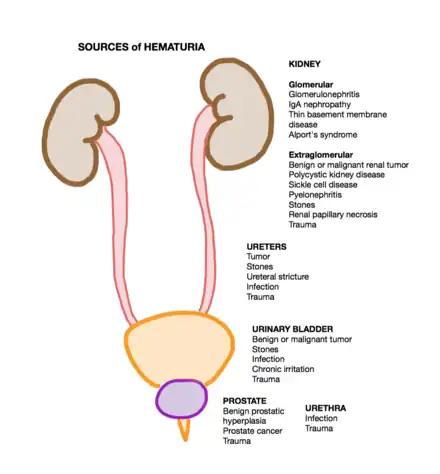
Urinary causes occur anywhere between the kidney glomerulus and the urethral meatus.[6] These can be divided into glomerular and non-glomerular causes.[6] Non-glomerular causes can be further subdivided into upper urinary tract and lower urinary tract causes.[6] The differential diagnosis can be furthered refined by the temporality of hematuria and associated symptoms.
Kidney
A glomerular cause is suggested by dysmorphic red blood cells, protein, and cellular casts in the urine.[6] This requires the consultation of a nephrologist.[6] Common causes include:
- IgA nephropathy
- Thin glomerular basement membrane disease
- Hereditary nephritis (Alport's disease)
- Benign familial hematuria
- Glomerulonephritis
Idiopathic hematuria is hematuria with an unknown cause. It is considered a glomerular syndrome.[7]
Upper urinary tract
- Urinary stones (i.e. kidney stone)[5]
- Pyelonephritis
- Kidney cancer
- Ureteral cancer
Lower urinary tract
- Urinary tract infection (UTI)
- Benign prostatic hyperplasia (BPH)
- Strenuous exercise
- Bladder cancer
- Genitourinary tract injury
Hemoglobinuria
Hemoglobin in the absence of red blood cells can also turn urine red. The inciting event for hemoglobin in the urine is hemolysis in the bloodstream. Hemolysis is a process where red blood cells lyse or burst. This releases hemoglobin into the bloodstream.[8] Hemoglobin then leaves the bloodstream and enters urinary tract at Bowman's capsule.
Children
Common causes of hematuria in children are:[9]
- Congenital abnormalities
- Non-vascular – ureteropelvic junction obstruction, posterior urethral valves, urethral prolapse, urethral diverticula, multicystic dysplastic kidney
- Vascular – arteriovenous malformations, hereditary hemorrhagic telangiectasias, renal vascular thromboses
- Acute nephritis
- Coagulopathy
- Urinary stones
- IgA nephropathy
- Post-streptococcal glomerulonephritis
- Benign familial hematuria
- Sickle cell trait or disease
- Alport syndrome
Diagnosis
After conducting a thorough history and physical examination, further medical testing is warranted. Patients can be stratified into high and low risk.[5] High-risk patients include those with visible hematuria or those with non-visible hematuria and risk factors.[5] A complete evaluation of the urinary tract is indicated for hematuria. This includes imaging of the upper urinary tract and cystoscopy of the lower urinary tract.[5]
Associated symptoms
The differential diagnosis can be furthered refined by the temporality of hematuria and associated symptoms. During urination, blood can appear in the urine at the onset, midstream, or later.[8] It can also have associated symptoms. These include nausea, fever, chills, abdominal pain, flank pain, groin pain, urinary frequency, urinary urgency, and pain or discomfort with urination.[6][8]
When hematuria becomes visible during urination can suggest where in the urinary tract the bleeding originates.[8] If it appears soon after the onset of urination, a distal site is suggested.[8] A longer delay suggests a more proximal lesion.[8] In other words, shorter times suggest distal sites while longer times suggest proximal sites. Hematuria that occurs throughout urination suggests that bleeding is occurring above the level of the bladder.[8]
The presence of hematuria without accompanying symptoms should be considered a tumor of the urinary tract until proven otherwise.[8] Other possible causes include acute glomerulonephritis, staghorn calculus, polycystic kidneys, benign prostatic hyperplasia, solitary renal cyst, sickle cell disease, and hydronephrosis.[8] It can also develop after vigorous exercise.[8][6]
Costovertebral angle tenderness suggests upper urinary tract obstruction.[5] A urinary stone is suggested by the presence of renal colic[8]. The presence of a fever suggests pyelonephritis.[5]
Medical imaging
The preferred modality is a multi-phasic computed topography (CT) urography.[5] This is a three-phase study that includes a non-contrast phase, an arterial phase, and an excretory phase.[6] The study should sufficiently evaluate the kidney and the urothelium lining the upper urinary tracts.[6] If there are contraindications to this study then alternative studies can be used.[5] One alternative is a magnetic resonance (MR) urography with and without intravenous contrast.[6] Another alternative is a retrograde pyelogram paired with either magnetic resonance imaging of the upper urinary tracts (MRI) or a renal ultrasound (US).[5][6] This imaging assessment is capable of excluding upper tract malignancies.[5]
Microscopic
Microscopic hematuria requires medical testing for detection. It is not visible to the naked eye. Rather it requires microscopic examination for detection.[5] It is defined as three or more red blood cells per high-powered field.[6] Another method for detection of microscopic hematuria is the dipstick method. This test works by detecting hemoglobin in a urine sample.[6] False positives can occur with dipstick testing if free hemoglobin or myoglobin are present.[6]
Younger people
For people younger than 35 years old presenting with asymptomatic microscopic hematuria, a cystoscopy may be warranted if risk factors are present.[5]
Initial negative evaluation
Evaluations of hematuria that do not reveal pathology require follow up. A urinary cytology may be helpful.[6] A urinalysis should be repeated once a year. Follow up can be discontinued after two consecutive negative urinalyses.[6] Repeat hematuria on follow-up studies warrants repeat upper urinary tract imaging and a cystoscopy.[6] This should be performed within three to five years of the first evaluation.[6]
Differential diagnosis
- Vaginal bleeding
- Gastrointestinal bleeding
- "Red urine" can result from the medication phenazopyridine[5]
Management
Acute clot retention
Acute clot retention is one of three emergencies that can occur with hematuria.[10] The other two are anemia and shock.[10] Blood clots can prevent urine outflow through either ureter or the bladder.[10] This is known as acute urinary retention.
Blood clots that remain in the bladder are digested by urinary urokinase producing fibrin fragments.[10] These fibrin fragments are natural anticoagulants and promote ongoing bleeding from the urinary tract.[10] Removing all blood clots prevents the formation of this natural anticoagulant.[10] This in turns facilitates the cessation of bleeding from the urinary tract.[10]
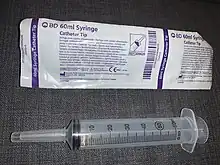
The acute management of obstructing clots is the placement of a large (22-24 French) urethral Foley catheter.[10] Clots are evacuated with a Toomey syringe and saline irrigation.[10] If this does not control the bleeding, management should escalate to continuous bladder irrigation (CBI) via a three-port urethral catheter.[10] If both a large urethral Foley catheter and CBI fail, an urgent cystoscopy in the operating room will be necessary.[10] Lastly, a transfusion and/or a correction of a coexisting coagulopathy may be necessary.[10]
Epidemiology
In the United States of America, microscopic hematuria has a prevalence of somewhere between 2% and 31%.[6] Higher rates exist in individuals older than 60 years of age and those with a current or past history of smoking.[6] Only a fraction of individuals with microhematuria are diagnosed with a urologic cancer.[6] When asymptomatic populations are screened with dipstick or microscopy medical testing about 2% to 3% of those with hematuria have a urologic cancer.[6] Routine screening is not recommended.[6] Individuals with risk factors who undergo repeated testing have higher rates of urologic malignancies.[6] These risks factors include age (>35 years), male gender, previous or current smoking, chemical exposure (e.g., benzenes or aromatic amines), and prior pelvic radiation therapy.[6]
Children
In children the prevalence is 0.5–2%.[11] Risks factor include older age and female gender.[12] About 5% of individuals with microscopic hematuria receive a cancer diagnosis. 40% of individuals with macroscopic hematuria (blood easily visible in the urine) receive a cancer diagnosis.[13]
Society and culture
In general, nephrologists are the experts of glomerular hematuria while urologists manage non-glomerular hematuria.[6]
References
- ↑ Dorland's illustrated medical dictionary. Dorland, W. A. Newman (William Alexander Newman), 1864-1956. (32nd ed.). Philadelphia, PA: Saunders/Elsevier. 2012. p. 645. ISBN 978-1-4160-6257-8. OCLC 706780870.
{{cite book}}: CS1 maint: others (link) - 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Saleem, MO; Hamawy, K (January 2020). "Hematuria". PMID 30480952.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 "Blood in urine". nhs.uk. 8 December 2017. Archived from the original on 18 October 2020. Retrieved 18 October 2020.
- ↑ "Definition of HEMATURIA". www.merriam-webster.com. Archived from the original on 2020-01-29. Retrieved 2019-11-25.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 "Medical Student Curriculum: Hematuria - American Urological Association". www.auanet.org. Archived from the original on 2019-11-28. Retrieved 2019-11-28.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 Coplen, D.E. (January 2013). "Diagnosis, Evaluation and Follow-Up of Asymptomatic Microhematuria (AMH) in Adults: AUA Guideline". Yearbook of Urology. 2013: 1–2. doi:10.1016/j.yuro.2013.07.019. ISSN 0084-4071.
- ↑ Izzo, Joseph L.; Sica, Domenic A.; Black, Henry Richard (2008). Hypertension Primer. Lippincott Williams & Wilkins. p. 382. ISBN 978-0-7817-8205-0. Archived from the original on 2020-08-03. Retrieved 2020-01-31.
- 1 2 3 4 5 6 7 8 9 10 11 McAninch, Jack W.; Lue, Tom (2013). Smith & Tanagho's General Urology. McGraw-Hill Education. pp. Chapter 3: Symptoms of Disorders of the Genitourinary Tract.
- ↑ Pade, Kathryn H.; Liu, Deborah R. (September 2014). "An evidence-based approach to the management of hematuria in children in the emergency department". Pediatric Emergency Medicine Practice. 11 (9): 1–13, quiz 14. ISSN 1549-9650. PMID 25296518.
- 1 2 3 4 5 6 7 8 9 10 11 12 Kaplan, Damara, MD, PhD; Kohn, Taylor. "Urologic Emergencies: Gross Hematuria with Clot Retention". American Urological Association. Archived from the original on 2019-11-28. Retrieved 2019-12-11.
- ↑ Shah, Samir (2014). Step-up to pediatrics. Ronan, Jeanine C.; Alverson, Brian (First ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. pp. 175–176. ISBN 978-1451145809. OCLC 855779297.
- ↑ Cohen, Robert A.; Brown, Robert S. (2003-06-05). "Clinical practice. Microscopic hematuria". The New England Journal of Medicine. 348 (23): 2330–2338. doi:10.1056/NEJMcp012694. ISSN 1533-4406. PMID 12788998.
- ↑ Sharp, Victoria; Barnes, Kerri D.; Erickson, Bradley D. (December 1, 2013). "Assessment of Asymptomatic Microscopic Hematuria in Adults". American Family Physician. 88 (11): 747–54. PMID 24364522. Archived from the original on January 29, 2020. Retrieved September 16, 2019.
External links
| Classification | |
|---|---|
| External resources |
- Ingelfinger, Julie R. (8 July 2021). "Hematuria in Adults". New England Journal of Medicine. 385 (2): 153–163. doi:10.1056/nejmra1604481.