Testicular pain
| Testicle pain | |
|---|---|
| Other names: Scrotal pain, orchialgia, genital pain | |
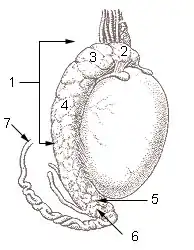 | |
| 1 - 6: Epididymis 7: Vas deferens | |
| Specialty | Urology |
| Types | Acute, chronic[1][2] |
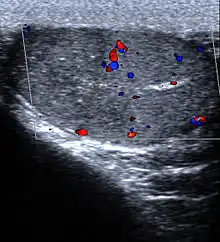
| Diagnostic method | Ultrasound, urine tests, blood tests[1][2] |
| Differential diagnosis | Acute: Epididymitis, testicular torsion, orchitis, varicocele, inguinal hernia, kidney stones, iliac artery aneurysm, testicular cancer, Fournier gangrene[1] Chronic: Varicocele, spermatocele, Henoch–Schönlein purpura, post-vasectomy pain syndrome, chronic pelvic pain syndrome[2] |
Testicular pain, also known as scrotal pain, is when one or both testicles or scrotum hurts.[3] Testicular pain may be of sudden onset or of long duration.[1][2] Often swelling is also present.[4] Long term pain is associated with depression, chronic prostatitis, infertility, and drug misuse.[2]
Causes of sudden onset include injury, epididymitis, testicular torsion, orchitis, varicocele, inguinal hernia, kidney stones, iliac artery aneurysm, testicular cancer, and Fournier gangrene.[1] Causes of chronic pain may include spermatocele, varicocele, post-vasectomy pain syndrome, vasculitis, interstitial cystitis, osteitis pubis, post hernia surgery nerve entrapment, side effect of amiodarone, and chronic pelvic pain syndrome.[2] Diagnosis may be supported by ultrasound, urine tests, and blood tests.[1][2] A CT scan of the abdomen may be useful in certain cases.[2]
Pain management is typically given with definitive treatment depending on the underlying cause.[2] Complaints related to the genital and urinary tract make up between 0.5% and 2.5% of emergency visits.[1] Long term pain effects about 100,000 people in the United States.[2]
Definition
Testicular pain is when part or all of either one or both testicles hurt. Pain of the scrotum is often included. It may be either acute (onset within a couple of days), subacute or chronic (duration of greater than 3 months).[1][2]
Chronic
Chronic scrotal pain (pain for greater than 3 months) may occur due to a number of underlying conditions.[5] It occurs in 15-19% of men post vasectomy, due to infections such as epididymitis, prostatitis, and orchitis, as well as varicocele, hydrocele, spermatocele, polyarteritis nodosa, testicular torsion, previous surgery and trauma.[5] In 25% of cases the cause is never determined.[5] The pain can persist for a long and indefinite period of time following the vasectomy, in which case it is termed post-vasectomy pain syndrome (PVPS).
Cause
The causes of testicular pain is broad and involves conditions from benign to life-threatening. The most common causes of pain in children presenting to the emergency room are testicular torsion (16%), torsion of a testicular appendage (46%), and epididymitis (35%).[6] In adults, the most common cause is epididymitis.
Testicular torsion
Testicular torsion usually presents with an acute onset of diffuse testicular pain and tenderness of less than 6 hrs of duration. There is often an absent or decreased cremasteric reflex, the testicle is elevated, and often is horizontal.[7] It occurs annually in about 1 in 4000 males before 25 years of age,[5] is most frequent among adolescents (65% of cases presenting between 12 – 18 years of age),[8] and is rare after 35 years of age.[9] Because it can lead to necrosis within a few hours, it is considered a surgical emergency.[9] Another version of this condition is a chronic illness called intermittent testicular torsion (ITT) which is characterized by recurrent rapid acute onset of pain in one testis which will temporarily assume a horizontal or elevated position in the scrotum similar to that of a full torsion followed by eventual spontaneous detortion and rapid solution of pain. Nausea or vomiting may also occur.[10]
Epididymitis and orchitis
Epididymitis occurs when there is inflammation of the epididymis (a curved structure at the back of the testicle).[9] This condition usually presents with gradual onset of varying degrees of pain, and the scrotum may be red, warm and swollen. It is often accompanied by symptoms of a urinary tract infection, fever, and in over half of cases it presents in combination with orchitis.[9] In those between the ages of 14 to 35 it is usually caused by either gonorrhea or chlamydia. In people either older or younger E. coli is the most common bacterial infection.[9] Treatment involves the use of antibiotics.[9]
Fournier's gangrene
Fournier's gangrene (an aggressive and rapidly spreading infection of the perineum) usually presents with fever and intense pain. It is a rare condition but fatal if not identified and aggressively treated with a combination of surgical debridement and broad spectrum antibiotics.[11]
Others
Many other less common conditions can lead to testicular pain. These include inguinal hernias, injury, hydroceles, disc herniations[12], and varicoceles among others. Testicular cancer is usually painless.[13] Another potential cause is epididymal hypertension (also known as "blue balls").[14][15]
Diagnostic approach
Physical findings
The cremaster reflex (elevation of the testicle in response to stroking the upper inner thigh) is typically present in epididymitis but absent in testicular torsion as the testis is already elevated.[9] Prehn's sign (the relief of pain with elevation) though a classic physical exam finding has not been found to be reliable in distinguishing torsion from other causes of testicular pain such as epididymitis.[16]
Laboratory tests
Useful tests that may help in the determination of the cause include a urinalysis (usually normal in testicular torsion). Pyuria and bacteriuria (white blood cells and bacteria in the urine) in patients with acute scrotum suggests an infectious cause such as epididymitis or orchitis and specific testing for gonorrhea and chlamydia should be done.[9] All people with chronic pain should be tested for gonorrhea and chlamydia.[5]
Imaging
Ultrasound is useful if the cause is not certain based on the above measures.[17] If the diagnosis of torsion is certain, imaging should not delay definitive management such as physical maneuvers and surgery.[9]
References
- 1 2 3 4 5 6 7 8 Boniface, Michael (16 Dec 2018). "Acute Scrotum Pain". StatPearls. PMID 29262236. Archived from the original on 13 April 2020. Retrieved 22 June 2019.
- 1 2 3 4 5 6 7 8 9 10 11 Leslie, Stephen (2 May 2019). "Chronic Testicular Pain (Orchialgia)". StatPearls. PMID 29494088. Archived from the original on 18 March 2020. Retrieved 22 June 2019.
- ↑ Jenkins, Jon L.; Braen, G. Richard (2005). Manual of Emergency Medicine. Lippincott Williams & Wilkins. p. 313. ISBN 978-0-7817-5035-6. Archived from the original on 29 August 2021. Retrieved 19 October 2020.
- ↑ Collins, R. Douglas (2003). Algorithmic Diagnosis of Symptoms and Signs: A Cost-effective Approach. Lippincott Williams & Wilkins. p. 464. ISBN 978-0-7817-3805-7. Archived from the original on 29 August 2021. Retrieved 19 October 2020.
- 1 2 3 4 5 Wampler SM, Llanes M (September 2010). "Common scrotal and testicular problems". Prim. Care. 37 (3): 613–26, x. doi:10.1016/j.pop.2010.04.009. PMID 20705202.
- ↑ Lewis AG, Bukowski TP, Jarvis PD, Wacksman J, Sheldon CA (February 1995). "Evaluation of acute scrotum in the emergency department". J. Pediatr. Surg. 30 (2): 277–81, discussion 281–2. doi:10.1016/0022-3468(95)90574-X. PMID 7738751.
- ↑ Karmazyn B, Steinberg R, Kornreich L (March 2005). "Clinical and sonographic criteria of acute scrotum in children: a retrospective study of 172 boys". Pediatr Radiol. 35 (3): 302–10. doi:10.1007/s00247-004-1347-9. PMID 15503003.
- ↑ Edelsberg JS, Surh YS (August 1988). "The acute scrotum". Emerg. Med. Clin. North Am. 6 (3): 521–46. PMID 3292226.
- 1 2 3 4 5 6 7 8 9 Trojian TH, Lishnak TS, Heiman D (April 2009). "Epididymitis and orchitis: an overview". Am Fam Physician. 79 (7): 583–7. PMID 19378875.
- ↑ Uribe, Juan F. (2008). Potts, Jeannette M. (ed.). Genitourinary pain and inflammation: diagnosis and management. Totowa, New Jersey: Humana. p. 150. ISBN 978-1-58829-816-4.
- ↑ Burch DM, Barreiro TJ, Vanek VW (November 2007). "Fournier's gangrene: be alert for this medical emergency" (PDF). JAAPA. 20 (11): 44–7. doi:10.1097/01720610-200711000-00020. PMID 18035764. Archived from the original (PDF) on 2009-10-07.
- ↑ Chu, Eric (7 August 2020). "Taming of the Testicular Pain Complicating Lumbar Disc Herniation With Spinal Manipulation". American Journal of Men's Health. doi:10.1177/1557988320949358. PMID 32772625. Archived from the original on 29 August 2021. Retrieved 2 September 2020.
- ↑ "Testicle pain: MedlinePlus Medical Encyclopedia". National Institute of Health. Archived from the original on 2016-07-05.
- ↑ Chalett JM, Nerenberg LT (October 2000). ""Blue balls": A diagnostic consideration in testiculoscrotal pain in young adults: A case report and discussion". Pediatrics. 106 (4): 843. doi:10.1542/peds.106.4.843. PMID 11015532.
- ↑ Wiener, SL; Walker, HK; Hall, WD; Hurst, JW (1990). "Testicular Pain". PMID 21250139.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Lavallee ME, Cash J (April 2005). "Testicular torsion: evaluation and management". Curr Sports Med Rep. 4 (2): 102–4. doi:10.1097/01.CSMR.0000306081.13064.a2. PMID 15763047.
- ↑ Galejs LE (February 1999). "Diagnosis and treatment of the acute scrotum". American Family Physician. 59 (4): 817–24. PMID 10068706. Archived from the original on 2011-06-06. Retrieved 2010-01-17.
External links
| External resources |
|---|