Radiculopathy
| Radiculopathy | |
|---|---|
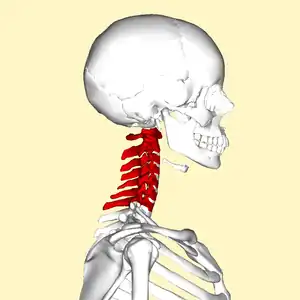 | |
| C5-C6, followed by C6-C7, is the most common location for radiculopathy in the neck. | |
| Specialty | Neurosurgery |
Radiculopathy, also commonly referred to as pinched nerve, refers to a set of conditions in which one or more nerves are affected and do not work properly (a neuropathy). Radiculopathy can result in pain (radicular pain), weakness, altered sensation (paresthesia) or difficulty controlling specific muscles.[1] Pinched nerves arise when surrounding bone or tissue, such as cartilage, muscles or tendons, put pressure on the nerve and disrupt its function.[2]
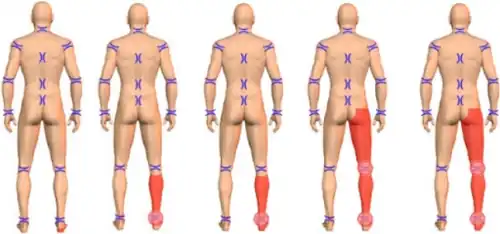
In a radiculopathy, the problem occurs at or near the root of the nerve, shortly after its exit from the spinal cord. However, the pain or other symptoms often radiate to the part of the body served by that nerve. For example, a nerve root impingement in the neck can produce pain and weakness in the forearm. Likewise, an impingement in the lower back or lumbar-sacral spine can be manifested with symptoms in the foot.
The radicular pain that results from a radiculopathy should not be confused with referred pain, which is different both in mechanism and clinical features. Polyradiculopathy refers to the condition where more than one spinal nerve root is affected.
Signs and symptoms
The clinical presentation is consistent with the following:[3][4]
- Pain
- Numbness
- Paresthesia
- Weakness (pattern consistent with distribution of particular nerve root)
Causes
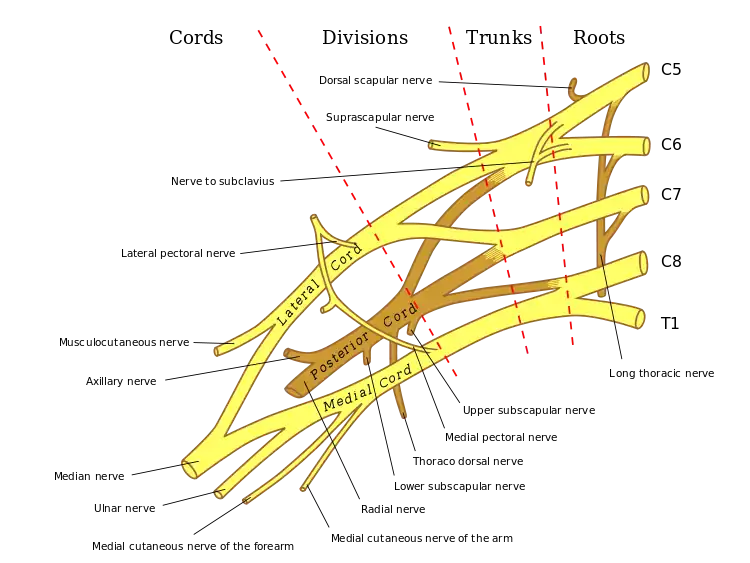
Radiculopathy most often is caused by mechanical compression of a nerve root usually at the exit foramen or lateral recess. It may be secondary to intervertebral disk herniation (most commonly at C7 and then the C6 level), degenerative disc disease, osteoarthritis, facet joint degeneration/hypertrophy, ligamentous hypertrophy, spondylolisthesis, or a combination of these factors.[5][6] Other possible causes of radiculopathy include neoplastic disease, infections such as shingles, HIV, or Lyme disease, spinal epidural abscess, spinal epidural hematoma, proximal diabetic neuropathy, Tarlov cysts, or, more rarely, sarcoidosis, arachnoiditis, tethered spinal cord syndrome, or transverse myelitis.[5]
Repeated, longer term exposure (5 years or more) to certain work-related activities may put people at risk of developing lumbosacral radiculopathy.[7] These behaviours may include physically demanding work, bending over or twisting at the trunk, lifting and carrying, or a combination of these activities.[7]
Less common causes of radiculopathy include injury caused by tumor (which can compress nerve roots locally) and diabetes (which can effectively cause ischemia or lack of blood flow to nerves).
Diagnosis
Clinical presentation
Radiculopathy is a diagnosis commonly made by physicians in primary care specialties, orthopedics, physiatry, and neurology. Physical examination may reveal motor and sensory deficits in the distribution of a nerve root. In the case of cervical radiculopathy, Spurling's test may elicit or reproduce symptoms radiating down the arm. Similarly, in the case of lumbosacral radiculopathy, a straight leg raise maneuver or a femoral nerve stretch test may demonstrate radiculopathic symptoms down the leg.[5] Deep tendon reflexes (also known as a Stretch reflex) may be diminished or absent in areas innervated by a particular nerve root.
Diagnosis typically involves electromyography and lumbar puncture.[5] Shingles is more common among the elderly and immunocompromised; usually (but not always) pain is followed by appearance of a rash with small blisters along a single dermatome.[5] It can be confirmed by quick laboratory tests.[8] Acute Lyme radiculopathy follows a history of outdoor activities during warmer months in likely tick habitats in the previous 1–12 weeks.[9] In the U.S., Lyme is most common in New England and Mid-Atlantic states and parts of Wisconsin and Minnesota, but it is expanding to other areas.[10][11] The first manifestation is usually an expanding rash possibly accompanied by flu-like symptoms. Lyme radiculopathy is usually worse at night and accompanied by extreme sleep disturbance, lymphocytic meningitis with variable headache and no fever, and sometimes by facial palsy or Lyme carditis.[12] Lyme can also cause a milder, chronic radiculopathy an average of 8 months after the acute illness.[5] Lyme can be confirmed by blood antibody tests and possibly lumbar puncture.[9][5] If present, the above conditions should be treated immediately.[5]
Although most cases of radiculopathy are compressive and resolve with conservative treatment within 4–6 weeks, guidelines for managing radiculopathy recommend first excluding possible causes that, although rare, require immediate attention, among them the following. Cauda equina syndrome should be investigated in case of saddle anesthesia, loss of bladder or bowel control, or leg weakness.[5] Cancer should be suspected if there is previous history of cancer, unexplained weight loss, or low-back pain that does not decrease by lying down or is unremitting.[5] Spinal epidural abscess is more common among those with diabetes mellitus or immunocompromised, who use intravenous drugs, or had spinal surgery, injection or catheter; it typically causes fever, leukocytosis and increased erythrocyte sedimentation rate.[5] If any of the previous is suspected, urgent magnetic resonance imaging is recommended for confirmation.[5] Proximal diabetic neuropathy typically affects middle aged and older people with well-controlled type-2 diabetes mellitus; onset is sudden causing pain usually in multiple dermatomes quickly followed by weakness.
Investigations
 Oblique projectional radiograph of a man presenting with pain by the nape and left shoulder, showing a stenosis of the left intervertebral foramen of cervical spinal nerve 4, corresponding with the affected dermatome.
Oblique projectional radiograph of a man presenting with pain by the nape and left shoulder, showing a stenosis of the left intervertebral foramen of cervical spinal nerve 4, corresponding with the affected dermatome.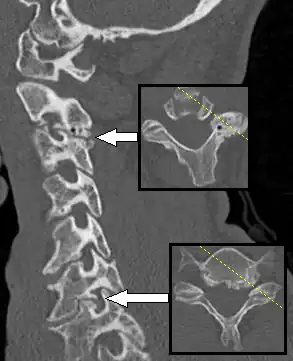 CT scan of a man presenting with radiculopathy of the left cervical spinal nerve 7, corresponding to spondylosis with osteophytes between the vertebral bodies C6 and C7 on the left side, causing foraminal stenosis at this level (lower arrow, showing axial plane). There is also spondylosis of the facet joint between C2 and C3, with some foraminal stenosis at this level (upper arrow), which appears to be asymptomatic.
CT scan of a man presenting with radiculopathy of the left cervical spinal nerve 7, corresponding to spondylosis with osteophytes between the vertebral bodies C6 and C7 on the left side, causing foraminal stenosis at this level (lower arrow, showing axial plane). There is also spondylosis of the facet joint between C2 and C3, with some foraminal stenosis at this level (upper arrow), which appears to be asymptomatic.
If symptoms do not improve after 4–6 weeks of conservative treatment, or the person is more than 50 years old, further tests are recommended.[5] The American College of Radiology recommends that projectional radiography is the most appropriate initial study in all patients with chronic neck pain.[13] Two additional diagnostic tests that may be of use are magnetic resonance imaging and electrodiagnostic testing. Magnetic resonance imaging (MRI) of the portion of the spine where radiculopathy is suspected may reveal evidence of degenerative change, arthritic disease, or another explanatory lesion responsible for the patient's symptoms. Electrodiagnostic testing, consisting of NCS (nerve conduction study) and EMG (electromyography), is also a powerful diagnostic tool that may show nerve root injury in suspected areas. On nerve conduction studies, the pattern of diminished Compound muscle action potential and normal sensory nerve action potential may be seen given that the lesion is proximal to the posterior root ganglion. Needle EMG is the more sensitive portion of the test, and may reveal active denervation in the distribution of the involved nerve root, and neurogenic-appearing voluntary motor units in more chronic radiculopathies. Given the key role of electrodiagnostic testing in the diagnosis of acute and chronic radiculopathies, the American Association of Neuromuscular & Electrodiagnostic Medicine has issued evidence-based practice guidelines, for the diagnosis of both cervical and lumbosacral radiculopathies.[14][15] The American Association of Neuromuscular & Electrodiagnostic Medicine has also participated in the Choosing Wisely Campaign and several of their recommendations relate to what tests are unnecessary for neck and back pain.[16]
Treatment
Ideally, effective treatment aims to resolve the underlying cause and restores the nerve root to normal function. Conservative treatment may include bed rest, physical therapy, or simply continuing to do usual activities; for pain, nonsteroidal anti-inflammatory drugs, nonopioid or, in some cases, narcotic analgesics may be prescribed.[5] A systematic review found moderate quality evidence that spinal manipulation is effective for the treatment of acute lumbar radiculopathy[17] and cervical radiculopathy.[18] Only low level evidence was found to support spinal manipulation for the treatment of chronic lumbar radiculopathies, and no evidence was found to exist for treatment of thoracic radiculopathy.[17] Evidence also supports consideration of epidural steroid injection with local anesthetic in improving both pain and function in cases of lumbosacral radiculopathy.[19]
Rehabilitation
With a recent injury (e.g. one that occurred one week ago), a formal physical therapy referral is not yet indicated. Often mild to moderate injuries will resolve or greatly improve within the first few weeks. Additionally, patients with acute injuries are often too sore to participate effectively in physical therapy so soon after the insult. Waiting two to three weeks is generally recommended before starting formal physical therapy. In acute injury resulting in lumbosacral radiculopathy, conservative treatment such as acetaminophen and NSAIDs should be the first line of therapy.[1]
Therapeutic exercises are frequently used in combination with many of the previously mentioned modalities and with great results. A variety of exercise regimens are available in patient treatment. An exercise regimen should be modified according to the abilities and weaknesses of the patient.[20] Stabilization of the cervicothoracic region is helpful in limiting pain and preventing re-injury. Cervical and lumbar support braces typically are not indicated for radiculopathy, and may lead to weakness of support musculature.[21] The first part of the stabilization procedure is achieving a pain free full range of motion which can be accomplished through stretching exercises. Subsequently, a strengthening exercise program should be designed to restore the deconditioned cervical, shoulder girdle, and upper trunk musculature.[22] As reliance on the neck brace diminishes, an isometric exercise regimen should be introduced. This is a preferred method of exercise during the sub-acute phase because it resists atrophy and is least likely to exacerbate the condition. Single plane resistance exercises against cervical flexion, extension, bending, and rotation are used.
Surgery
While conservative approaches for rehabilitation are ideal, some patients will not improve and surgery is still an option.[23] Patients with large cervical disk bulges may be recommended for surgery; however, most often, conservative management will help the herniation regress naturally.[24] Procedures such as foraminotomy, laminotomy, or discectomy may be considered by neurosurgeons and orthopedic surgeons. Regarding surgical interventions for cervical radiculopathy, the anterior cervical discectomy and fusion procedure is more commonly performed than the posterior cervical foraminotomy procedure.[25] However, both procedures are likely equally effective and without significant differences in their complication rates.[25]
Epidemiology
Cervical radiculopathy has an annual incidence rate of 107.3 per 100,000 for men and 63.5 per 100,000 for women, whereas lumbar radiculopathy has a prevalence of approximately 3-5% of the population.[26][27] According to the AHRQ's 2010 National Statistics for cervical radiculopathy, the most affected age group is between 45 and 64 years with 51.03% of incidents. Females are affected more frequently than males and account for 53.69% of cases. Private insurance was the payer in 41.69% of the incidents followed by Medicare with 38.81%. In 71.61% of cases the patients' income was considered not low for their zipcode. Additionally over 50% of patients lived in large metropolitans (inner city or suburb). The South is the most severely affected region in the US with 39.27% of cases. According to a study performed in Minnesota, the most common manifestation of this set of conditions is the C7 monoradiculopathy, followed by C6.[28]
See also
References
- 1 2 "Cervical Radiculopathy (Pinched Nerve)". OrthoInfo by American Academy of Orthopaedic Surgeons. June 2015. Archived from the original on 3 November 2017. Retrieved 22 September 2017.
- ↑ "Pinched Nerve Symptoms & Treatment | Advanced Neurosurgery". Advanced Neurosurgery Associates. Archived from the original on 2021-01-20. Retrieved 2020-12-14.
- ↑ Childress MA, Becker BA (May 2016). "Nonoperative Management of Cervical Radiculopathy". American Family Physician. 93 (9): 746–54. PMID 27175952. Archived from the original on 2022-03-24. Retrieved 2022-09-17.
- ↑ Tawa N, Rhoda A, Diener I (February 2017). "Accuracy of clinical neurological examination in diagnosing lumbo-sacral radiculopathy: a systematic literature review". BMC Musculoskeletal Disorders. 18 (1): 93. doi:10.1186/s12891-016-1383-2. PMC 5324296. PMID 28231784.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Tarulli AW, Raynor EM (May 2007). "Lumbosacral radiculopathy" (PDF). Neurologic Clinics. 25 (2): 387–405. doi:10.1016/j.ncl.2007.01.008. PMID 17445735. S2CID 15518713. Archived from the original (PDF) on 2019-02-20.
- ↑ Iyer S, Kim HJ (September 2016). "Cervical radiculopathy". Current Reviews in Musculoskeletal Medicine. 9 (3): 272–80. doi:10.1007/s12178-016-9349-4. PMC 4958381. PMID 27250042.
- 1 2 Kuijer PP, Verbeek JH, Seidler A, Ellegast R, Hulshof CT, Frings-Dresen MH, Van der Molen HF (September 2018). "Work-relatedness of lumbosacral radiculopathy syndrome: Review and dose-response meta-analysis". Neurology. 91 (12): 558–564. doi:10.1212/01.wnl.0000544322.26939.09. PMC 6161552. PMID 30120136. Archived from the original on 2022-03-20. Retrieved 2022-09-17.
- ↑ Dworkin RH, Johnson RW, Breuer J, Gnann JW, Levin MJ, Backonja M, et al. (January 2007). "Recommendations for the management of herpes zoster". Clinical Infectious Diseases. 44 Suppl 1: S1-26. doi:10.1086/510206. PMID 17143845. S2CID 10894629. Archived from the original on 2021-08-28. Retrieved 2022-09-17.
- 1 2 Shapiro ED (May 2014). "Clinical practice. Lyme disease" (PDF). The New England Journal of Medicine. 370 (18): 1724–31. doi:10.1056/NEJMcp1314325. PMC 4487875. PMID 24785207. Archived from the original (PDF) on 19 October 2016.
- ↑ "Lyme Disease Data and surveillance". Lyme Disease. Centers for Disease Control and Prevention. 2019-02-05. Archived from the original on 2019-04-13. Retrieved April 12, 2019.
- ↑ "Lyme Disease risk areas map". Risk of Lyme disease to Canadians. Government of Canada. 2015-01-27. Archived from the original on 2019-05-10. Retrieved May 8, 2019.
- ↑ Ogrinc K, Lusa L, Lotrič-Furlan S, Bogovič P, Stupica D, Cerar T, et al. (August 2016). "Course and Outcome of Early European Lyme Neuroborreliosis (Bannwarth Syndrome): Clinical and Laboratory Findings". Clinical Infectious Diseases. 63 (3): 346–53. doi:10.1093/cid/ciw299. PMID 27161773.
- ↑ Malanga GA. "Cervical Radiculopathy Workup". Archived from the original on 2018-06-12. Retrieved 2017-06-29. Updated: Dec 14, 2016
- ↑ So YT (1999). "Guidelines in electrodiagnostic medicine. Practice parameter for needle electromyographic evaluation of patients with suspected cervical radiculopathy" (PDF). Muscle & Nerve. Supplement. 8: S209-21. PMID 16921635. Archived (PDF) from the original on 2016-08-20. Retrieved 2022-09-17.
- ↑ Cho SC, Ferrante MA, Levin KH, Harmon RL, So YT (August 2010). "Utility of electrodiagnostic testing in evaluating patients with lumbosacral radiculopathy: An evidence-based review". Muscle & Nerve. 42 (2): 276–82. doi:10.1002/mus.21759. PMID 20658602. S2CID 14391502. Archived from the original on 2022-12-19. Retrieved 2022-09-17.
- ↑ "American Association of Neuromuscular & Electrodiagnostic Medicine". Choosing Wisely. 2015-02-10. Archived from the original on 2018-04-06. Retrieved 2018-04-05.
- 1 2 Leininger B, Bronfort G, Evans R, Reiter T (February 2011). "Spinal manipulation or mobilization for radiculopathy: a systematic review". Physical Medicine and Rehabilitation Clinics of North America. 22 (1): 105–25. doi:10.1016/j.pmr.2010.11.002. PMID 21292148.
- ↑ Zhu L, Wei X, Wang S (February 2016). "Does cervical spine manipulation reduce pain in people with degenerative cervical radiculopathy? A systematic review of the evidence, and a meta-analysis". Clinical Rehabilitation. 30 (2): 145–55. doi:10.1177/0269215515570382. PMID 25681406. S2CID 23757555.
- ↑ Manchikanti L, Knezevic NN, Boswell MV, Kaye AD, Hirsch JA (March 2016). "Epidural Injections for Lumbar Radiculopathy and Spinal Stenosis: A Comparative Systematic Review and Meta-Analysis". Pain Physician. 19 (3): E365-410. doi:10.36076/ppj/2016.19.E365. PMID 27008296.
- ↑ Cleland JA, Whitman JM, Fritz JM, Palmer JA (December 2005). "Manual physical therapy, cervical traction, and strengthening exercises in patients with cervical radiculopathy: a case series". The Journal of Orthopaedic and Sports Physical Therapy. 35 (12): 802–11. doi:10.2519/jospt.2005.35.12.802. PMID 16848101.
- ↑ Muzin S, Isaac Z, Walker J, Abd OE, Baima J (June 2008). "When should a cervical collar be used to treat neck pain?". Current Reviews in Musculoskeletal Medicine. 1 (2): 114–9. doi:10.1007/s12178-007-9017-9. PMC 2684205. PMID 19468883.
- ↑ Saal JA, Saal JS (April 1989). "Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. An outcome study". Spine. 14 (4): 431–7. doi:10.1097/00007632-198904000-00018. PMID 2718047. S2CID 12334905.
- ↑ Gebreyohanes, A; Erotocritou, M; Choi, D (16 June 2022). "Appraising The Evidence for Conservative versus Surgical Management of Motor Deficits in Degenerative Cervical Radiculopathy". Global Spine Journal: 21925682221109562. doi:10.1177/21925682221109562. PMID 35708971. S2CID 249709589.
- ↑ Heckmann JG, Lang CJ, Zöbelein I, Laumer R, Druschky A, Neundörfer B (October 1999). "Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients". Journal of Spinal Disorders. 12 (5): 396–401. doi:10.1097/00002517-199910000-00008. PMID 10549703.
- 1 2 Liu WJ, Hu L, Chou PH, Wang JW, Kan WS (November 2016). "Comparison of Anterior Cervical Discectomy and Fusion versus Posterior Cervical Foraminotomy in the Treatment of Cervical Radiculopathy: A Systematic Review". Orthopaedic Surgery. 8 (4): 425–431. doi:10.1111/os.12285. PMC 6584082. PMID 28032703.
- ↑ Berry JA, Elia C, Saini HS, Miulli DE (October 2019). "A Review of Lumbar Radiculopathy, Diagnosis, and Treatment". Cureus. 11 (10): e5934. doi:10.7759/cureus.5934. PMC 6858271. PMID 31788391. Archived from the original on 2022-07-03. Retrieved 2022-09-17.
- ↑ Woods BI, Hilibrand AS (June 2015). "Cervical radiculopathy: epidemiology, etiology, diagnosis, and treatment". Journal of Spinal Disorders & Techniques. 28 (5): E251-9. doi:10.1097/BSD.0000000000000284. PMID 25985461. S2CID 1017140. Archived from the original on 2022-12-19. Retrieved 2022-09-17.
- ↑ Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT (April 1994). "Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990". Brain. 117 (2): 325–35. doi:10.1093/brain/117.2.325. PMID 8186959.
Further reading
- Pachner AR (1989-10-01). "Neurologic manifestations of Lyme disease, the new "great imitator"". Reviews of Infectious Diseases. 11 Suppl 6: S1482-6. doi:10.1093/clinids/11.supplement_6.s1482. PMID 2682960. S2CID 3862308. Archived from the original on 2021-09-22. Retrieved 2022-09-17.
- Chou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, et al. (September 2015). "Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis". Annals of Internal Medicine. 163 (5): 373–81. doi:10.7326/M15-0934. PMID 26302454. S2CID 25696028.
External links
| Classification |
|---|
- Radiculopathy at the US National Library of Medicine Medical Subject Headings (MeSH)