Polymyalgia rheumatica
| Polymyalgia rheumatica | |
|---|---|
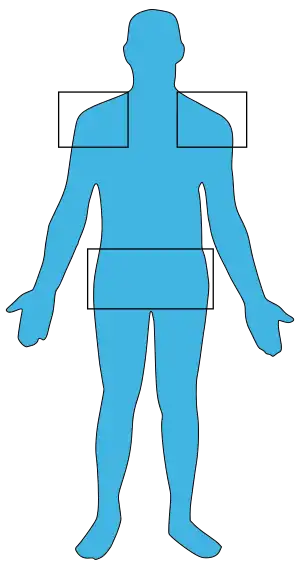 | |
| Usual location of pain in polmyalgia rheumatica | |
| Specialty | Rheumatology |
| Symptoms | Pain and stiffness of the neck, shoulders, and hips, fever, weakness, weight loss[1] |
| Complications | Temporal arteritis[2] |
| Usual onset | > 50 years old[3] |
| Duration | Few years[4] |
| Causes | Unknown[5] |
| Diagnostic method | Supported by CRP and ESR[6] |
| Differential diagnosis | Rheumatoid arthritis, myositis, vasculitis, dermatomyositis, fibromyalgia[6][7] |
| Treatment | Corticosteroids, methotrexate[8][7] |
| Frequency | 6 per 1,000 (N. Europeans over 50 years)[7] |
Polymyalgia rheumatica (PMR) is a syndrome with pain and stiffness, usually in the neck, shoulders, and hips.[1] Other symptoms may include fever, weakness, and weight loss.[1] The onset can be sudden or gradual.[9] Often stiffness is greatest first thing in the morning.[9] PMR may be complicated by temporal arteritis, an inflammation of blood vessels which can cause blindness if not treated.[2]
While the exact cause is unclear, the disorder is believed to be related to immune, genetic, environmental, and age related factors.[5] One theory is that certain infections may act as a trigger.[7][5] While there is no definitive test, C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can be useful.[6]
PMR is usually treated with corticosteroids taken by mouth.[8] Most people need to continue the corticosteroid treatment for six month to two years.[4] The use of NSAIDs may also help but are generally not sufficient on their own.[4] PMR usually resolves within a few years, but treatment results in faster symptom improvement.[4]
PMR is most common in those over the age of 50, particularly in those between the ages of 70 and 80.[3] Persons of Northern European descent are at greatest risk with about 6 per 1,000 people over the age of 50 affected.[7] The disease is uncommon in other ethnic groups.[7] Women are more commonly affected than men.[7] Descriptions of PMR are believed to date from as early as 1888 by Bruce with the current name attributed to Barber in 1957.[10] It takes its name from the Greek word Πολυμυαλγία polymyalgia, which means "pain in many muscles".[11]
Signs and symptoms
A wide range of symptoms can indicate if a person has polymyalgia rheumatica. The classic symptoms include:
- Pain and stiffness (moderate to severe) in the neck, shoulders, upper arms, thighs, and hips, which inhibits activity, especially in the morning/after sleeping. Pain can also occur in the groin area and in the buttocks. The pain can be limited to one of these areas as well. It is a disease of the "girdles" meaning shoulder girdle or pelvic girdle.
- Fatigue and lack of appetite (possibly leading to weight loss)
- Anemia
- An overall feeling of illness or flu-like symptoms.
- Low-grade (mild) fever[12] or abnormal temperature is sometimes present.
- In most people, it is characterized by constant fatigue, weakness and sometimes exhaustion.
About 15% of people who are diagnosed with polymyalgia rheumatica also have temporal arteritis, and about 50% of people with temporal arteritis have polymyalgia rheumatica.[13] Some symptoms of temporal arteritis include headaches, scalp tenderness, jaw or facial soreness, distorted vision, or aching in the limbs caused by decreased blood flow, and fatigue.[13]
Causes

The cause of PMR is not well understood. The pain and stiffness result from the activity of inflammatory cells and proteins that are normally a part of the body's disease-fighting immune system, and the inflammatory activity seems to be concentrated in tissues surrounding the affected joints.[15] During this disorder, the white blood cells in the body attack the lining of the joints, causing inflammation.[16] Inherited factors also play a role in the probability that an individual will develop PMR. Several theories have included viral stimulation of the immune system in genetically susceptible individuals.[17]
Infectious disease may be a contributing factor. This would be expected with sudden onset of symptoms, for example. In addition, new cases often appear in cycles in the general population, implying a viral connection. Studies are inconclusive, but several somewhat common viruses were identified as possible triggers for PMR.[15] The viruses thought to be involved include the adenovirus, which causes respiratory infections; the human parvovirus B19, an infection that affects children; and the human parainfluenza virus.[16] Some sufferers attribute the onset of PMR to stress.
Persons having the HLA-DR4 type of human leucocyte antigen appear to have a higher risk of PMR.[18]
Diagnosis
| Criteria | No US | With US |
|---|---|---|
| Morning stiffness > 45 min | 2 | 2 |
| Hip pain or decreased ability to move | 1 | 1 |
| No RF or ACPA | 1 | 1 |
| No other joints involved | 1 | 1 |
| Shoulder or hip bursitis or synovitis | N/A | 1 |
| Both shoulders bursitis or synovitis | N/A | 1 |
No specific test confirms the diagnoses and many other diseases can cause inflammation and muscle pain, but a few tests can support the diagnosis as can the description of the symptoms.[17][19]
Based on 2012 criteria for PMR, a score of > 3 without the addition of ultrasound findings and a score of >4 with ultrasound findings confirms the diagnosis in those over the age of 50 with typical symptoms and an elevated ESR or CRP.[7]
Blood tests
Blood tests usually performed are the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). ESR measures measures how fast the person's red blood cells settle in a test tube. The faster the blood cells settle, the higher the ESR value, which means inflammation is present. Many conditions can cause an elevated ESR, so this test alone is not proof that a person has polymyalgia rheumatica.[19][20]
CRP is produced by the liver in response to an injury or infection, and people with polymyalgia rheumatica usually have high levels.[19][20] However, like the ESR, this test is also not very specific.
Biopsy
If symptoms of temporal arteritis are present a biopsy sample may be taken from the temporal artery.[7] Such a biopsy is not needed in those who do not have symptoms of temporal arteritis.[7]
Treatment
Prednisone is the drug of choice for PMR,[21] and treatment duration is frequently greater than one year.[17] If the person does not experience dramatic improvement after three days of 10–20 mg prednisone per day by mouth, the diagnosis should be reconsidered.[22] Sometimes relief of symptoms may occur in several hours after starting treatment.
In those who are unable to take steroids due to side effects, relapse despite steroid therpy, or require prolonged treatment methotrexate may be used.[7]
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen are ineffective in the initial treatment of PMR,[23] but they may be used in conjunction with the maintenance dose of corticosteroid.[24]
Along with medical treatment, people are encouraged to exercise and eat healthily—helping to maintain a strong immune system and build strong muscles and bones.[25] A diet of fruits, vegetables, whole grains, and low-fat meat and dairy products, avoiding foods with high levels of refined sugars and salt is recommended.[26]
Epidemiology
PMR generally only affects adults over the age of 50.[23] The average age of onset is about 70 years old.[13][27] Women are twice as likely to get PMR as men.[27] Caucasians are more likely to get the disease; specifically people of Northern European origin such as Scandinavians.[27][13]
See also
References
- 1 2 3 Nancy Garrick, Deputy Director (11 April 2017). "Polymyalgia Rheumatica". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Archived from the original on 9 October 2020. Retrieved 27 September 2020.
- 1 2 Schmidt, J; Warrington, KJ (1 August 2011). "Polymyalgia rheumatica and giant cell arteritis in older patients: diagnosis and pharmacological management". Drugs & Aging. 28 (8): 651–66. doi:10.2165/11592500-000000000-00000. PMID 21812500.
- 1 2 Nancy Garrick, Deputy Director (11 April 2017). "Polymyalgia Rheumatica". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Archived from the original on 9 October 2020. Retrieved 27 September 2020.
- 1 2 3 4 Nancy Garrick, Deputy Director (11 April 2017). "Polymyalgia Rheumatica". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Archived from the original on 9 October 2020. Retrieved 27 September 2020.
- 1 2 3 Nancy Garrick, Deputy Director (11 April 2017). "Polymyalgia Rheumatica". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Archived from the original on 9 October 2020. Retrieved 27 September 2020.
- 1 2 3 Nancy Garrick, Deputy Director (11 April 2017). "Polymyalgia Rheumatica". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Archived from the original on 9 October 2020. Retrieved 27 September 2020.
- 1 2 3 4 5 6 7 8 9 10 11 12 Matteson, EL; Dejaco, C (2 May 2017). "Polymyalgia Rheumatica". Annals of internal medicine. 166 (9): ITC65–ITC80. doi:10.7326/AITC201705020. PMID 28460395.
- 1 2 Dejaco, C; Singh, YP (October 2015). "2015 Recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative". Annals of the Rheumatic Diseases. 74 (10): 1799–807. doi:10.1136/annrheumdis-2015-207492. PMID 26359488.
- 1 2 Nancy Garrick, Deputy Director (11 April 2017). "Polymyalgia Rheumatica". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Archived from the original on 9 October 2020. Retrieved 27 September 2020.
- ↑ Clinic, Cleveland (2010). Current Clinical Medicine E-Book: Expert Consult - Online. Elsevier Health Sciences. p. 1147. ISBN 978-1-4377-3571-0. Archived from the original on 28 August 2021. Retrieved 27 September 2020.
- ↑ Sebastian, Anton (2018). A Dictionary of the History of Medicine. Routledge. ISBN 978-1-351-46999-9. Archived from the original on 28 August 2021. Retrieved 27 September 2020.
- ↑ "Polymyalgia Rheumatica symptoms". MayoClinic. Dec 4, 2010. Archived from the original on 2011-12-31. Retrieved 2012-01-19.
- 1 2 3 4 Gelfand JL (November 18, 2007). "Polymyalgia Rheumatica and Temporal Arteritis". WebMD. Archived from the original on 2008-06-11. Retrieved 2008-06-10.
- ↑ Manzo, Ciro; Natale, Maria; Castagna, Alberto (September 2021). "Polymyalgia rheumatica as uncommon adverse event following immunization with COVID‐19 vaccine: A case report and review of literature". AGING MEDICINE. 4 (3): 234–238. doi:10.1002/agm2.12171. Retrieved 10 February 2023.
- 1 2 "Polymyalgia Rheumatica causes". MayoClinic. Dec 4, 2010. Archived from the original on 2008-06-23. Retrieved 2012-01-19.
- 1 2 "Polymyalgia Rheumatica causes". MayoClinic. May 17, 2008. Archived from the original on June 23, 2008. Retrieved 2012-01-19.
- 1 2 3 Shiel Jr WC (2008-03-13). "Polymyalgia Rheumatica (PMR) & Giant Cell Arteritis (Temporal Arteritis)". MedicineNet. Archived from the original on 2008-06-11. Retrieved 2008-06-10.
- ↑ Page 255 in: Elizabeth D Agabegi; Agabegi, Steven S. (2008). Step-Up to Medicine (Step-Up Series). Hagerstwon, MD: Lippincott Williams & Wilkins. ISBN 978-0-7817-7153-5.
- 1 2 3 "Polymyalgia Rheumatica tests and diagnosis". MayoClinic. Dec 4, 2010. Archived from the original on 2008-06-23. Retrieved 2012-01-19.
- 1 2 "Polymyalgia Rheumatica tests and diagnosis". MayoClinic. May 17, 2008. Archived from the original on June 23, 2008. Retrieved 2012-01-19.
- ↑ Hernández-Rodríguez J, Cid MC, López-Soto A, Espigol-Frigolé G, Bosch X (Nov 2009). "Treatment of polymyalgia rheumatica: a systematic review". Archives of Internal Medicine. 169 (20): 1839–50. doi:10.1001/archinternmed.2009.352. PMID 19901135.
- ↑ McPhee SJ, Papadakis MA (2010). Current Medical Diagnosis and Treatment. p. 767. ISBN 978-0071624442.
- 1 2 Docken WP (August 2009). "Polymyalgia rheumatica". American College of Rheumatology. Archived from the original on 2011-12-28. Retrieved 2012-01-20.
- ↑ "Polymyalgia rheumatica". MDGuidelines. Archived from the original on 2012-02-15. Retrieved 2012-01-20.
- ↑ "Polymyalgia Rheumatica lifestyle and home remedies". MayoClinic. May 17, 2008. Archived from the original on June 23, 2008. Retrieved 2012-01-19.
- ↑ "Polymyalgia Rheumatica lifestyle and home remedies". MayoClinic. Dec 4, 2010. Archived from the original on 2008-06-23. Retrieved 2012-01-19.
- 1 2 3 "Polymyalgia Rheumatica risk factors". MayoClinic. Dec 4, 2010. Archived from the original on 2012-01-02. Retrieved 2012-01-19.
External links
| Classification | |
|---|---|
| External resources |
- Questions and Answers about Polymyalgia Rheumatica and Giant Cell Arteritis Archived 2017-04-04 at the Wayback Machine - US National Institute of Arthritis and Musculoskeletal and Skin Diseases