Simple bone cyst
| Simple bone cyst | |
|---|---|
| Other names: Solitary bone cyst,[1][2] unicameral bone cyst (not recommended)[1] | |
 | |
| X-ray: Simple bone cyst in left upper arm of 13 year old | |
| Specialty | Orthopedics |
| Symptoms | None, or broken bone[3] |
| Complications | Broken bone[1] |
| Causes | Unknown[1] |
| Diagnostic method | X-ray.[3] |
| Prognosis | Good[4] |
| Frequency | 2M:F[1] |
A simple bone cyst, also known as a solitary bone cyst, is a non-cancerous cavity in bone, filled with a yellow-colored fluid, usually in a long bone of a child.[1][2] It is usually discovered by chance as often there are no symptoms, but may present with an unexpected broken bone, pain, swelling or reduced movement.[1][2]
The cause is unknown.[1] Diagnosis is usually by X-ray.[3] Treatment ranges from simply monitoring it to see if it spontaneously heals, draining the fluid and instilling steroid/bone marrow, or surgically scraping it out.[3]
It does not spread beyond the bone.[5] The outcome is generally good.[4] Around 10 - 20% recur, particularly if diagnosed before age 5 years.[1] After a broken bone, around 10% can heal.[1] Males are twice as likely to be affected than females.[1]
It was recognised as a distinct condition in 1942 by Jaffe and Lichtenstein.[6]
Classification
It can be classified into two categories: active and latent.[4] An active cyst is next to the growth plate and tends to grow until it fills the entire diaphysis, the shaft, of the bone; depending on the invasiveness of the cyst, it can cause an unprovoked break of the bone or even destroy the growth plate leading to the permanent shortening of the bone.[4] A latent cyst is located away from the growth plate and is more likely to heal with treatment.[4]
Signs and symptoms
_(Radiopaedia_7616).png.webp)
Most simple bone cysts do not cause any symptoms and are discovered as accidental findings on radiographs or CT scans made for other reasons.[3] Although it can form in any bone structure, it is predominantly found in the long bone of the upper arm near the shoulder, and long bone of the thigh near the hip.[6] Large lesions can cause nearby areas of bone to thin, which may result in a fracture and cause pain.[1][2] There may be a swelling or problem in moving the affected bone.[1]
Cause
The cause is unknown.[1]
Whether the cause is associated with a disorder of the growth plate, problems with circulation, or trauma, is unclear.[6]
Diagnosis
X-rays
Simple bone cysts are often found incidentally on X-rays. About 90 to 95% of the lesion is found in metaphysics of long bones. The cyst is centered, oblong in shape along the long axis of a long bone. Rarely, they are large and multicameral and are found in diaphysis. When fracture is present, there may be a small bone fragment migrated in the cystic fluid. This is called "fallen fragment sign" which is diagnostic of simple bone cyst. Besides, a bubble migrating upwards (known as "rising bubble sign") is another feature suggesting of simple bone cyst.[7]
 Multloculated cavity in the long bone of the thigh, near the hip.
Multloculated cavity in the long bone of the thigh, near the hip.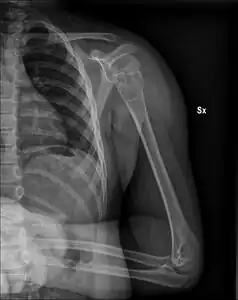 Unprovoked break in the long bone of the upper arm,, with "fallen leaf" sign.
Unprovoked break in the long bone of the upper arm,, with "fallen leaf" sign. Unprovoked break in big toe, with "fallen leaf" sign.
Unprovoked break in big toe, with "fallen leaf" sign..jpg.webp) Break through simple bone cyst in the long bone of the thigh, near the hip.
Break through simple bone cyst in the long bone of the thigh, near the hip.
CT scan
CT scan shows a thin-walled lesion with pseudo septum (incomplete septum or a septum with perforations that allows communications between two chambers). CT scan is used to assess cyst wall thickness and risk of fracture.[7]
MRI

Magnetic resonance imaging (MRI) is used to identify the precise location of the cyst, to see how aggressive the disease is, and to determine the actual shape and size.[4] The MRI uses a combination of magnets and radio-frequencies to produce various detailed, computerized images of the cyst and its surrounding body structures.[4]
Bone scans
Bone scintigraphy is generally not preformed as may not show the cyst.[8] It might show a very small uptake in tracer with low density in the centre.[8]
Treatment
If there is a high probability of a fracture resulting from the unicameral bone cyst, then surgical treatment is necessary.[4] Specific methods can be determined by the physician based upon the person's age, medical history, tolerance for certain medical procedures or medicine, health, and extremity of the disease.[4] The treatment can involve or incorporate one or more of the following surgical methods, which are performed by a pediatric orthopedic surgeon:[4]
- Surgeons create an incision or opening in the bone to drain out the fluids inside the cyst.[4] After the fluid is drained, a curette is used to scrape the lining tissue out of the lesion.[4]
- Bone grafting is proceeded with after curettage; the empty cavity is transplanted with donor bone tissue, bone chips taken from another bone, or artificial material.[4]
- Steroid injection:
- An injection of methylprednisolone acetate into the lesion helps reduce the levels of prostaglandin.[4] Prostaglandin is a fatty acid that reduces cyst’s ability to be reabsorbed into the bone.[4] To begin an operation using steroids, biopsy needles are placed into the cyst and the interstitial fluids are drained.[4] The cyst is then filled with radiographic contrast to determine the volume and shape of the cyst.[4] If the cyst can be filled, it will be injected with methylprednisolone acetate in several intervals for a time span of six to twelve months.[4] Once the level of prostaglandin decreases, the cyst will be reabsorbed into the bone and disappear.[4] Treatments using steroid injections are preferred over curettage, but there are few risks from the method, which are limited to infection, fracture, and reappearance of the cyst.[4]
If a person needs to be treated with surgery, a standard surgical procedure would be called for; the person would be resting in Fowler's position, a semi-sitting position, under general anesthesia.[9] The exact size, shape, and distance between the acromion to the midpoint of the cyst are measured by a digital radiograph or MRI scan.[9] A small, longitudinal skin incision, about 1 cm long, is made at the center of the cyst.[9] Next, by using a trephine or drill bit, a small aperture is made inside the incision.[9] Fluids contained in the cyst are drained and curved, metal impactors are used to break any septa, or membranes, within the cyst.[9] Curettes are then used to remove the entire cyst from the diaphysis.[9] After the removal of the cystic membrane, a 95% ethanol solution is injected into the cavity to produce a chemical cauterization to burn away any residual active membrane for 30 seconds and then aspirated.[9] Saline solution is then immediately injected into the cavity to wash out any residual ethanol solution and to mitigate any damage to healthy tissue; this irrigation process of ethanol and saline solutions is repeated for another 2 to 3 times.[9] A curved impactor is inserted into the cavity and used to penetrate the boundary between the cyst and bone marrow; the intentional penetrations will allow bone marrow cells to migrate into the cavity to produce a source of osteoinductive cells, cells that induce bony growth.[9] Furthermore, the cavity is completely filled with bone graft substitute, such as calcium sulfate.[9] Finally, one cannulated screw is placed into the aperture.[9]
Outcome
The outcome is generally good.[4] It does not spread beyond the bone.[5] Around 10 - 20% recur, particularly if diagnosed before age 5 years.[1] After a broken bone, around 10% can heal.[1]
Epidemiology
Most simple bone cysts are diagnosed in growing bone in under 20 year olds.[1] Around half occur in the long bone of the upper arm and a quarter in the long bone of the thigh.[1] Males are twice as likely to be affected than females.[1]
History
One theory of its cause was hypothesized by Jonathan Cohen in 1970.[6] Cohen studied interstitial fluid in six children undergoing treatment for unicameral bone cysts.[6] He believed that the chemical composition of the fluid found in the bone cyst was similar to the chemical make-up in serum.[10] Cohen theorized that the unicameral bone cyst occurs when interstitial fluids in cancellous bones quickly accumulate in one region from blockage.[10]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 WHO Classification of Tumours Editorial Board, ed. (2020). "3. Bone tumours: simple bone cyst". Soft Tissue and Bone Tumours: WHO Classification of Tumours. Vol. 3 (5th ed.). Lyon (France): International Agency for Research on Cancer. pp. 467–469. ISBN 978-92-832-4503-2. Archived from the original on 2021-06-13. Retrieved 2021-06-06.
- 1 2 3 4 "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Archived from the original on 1 August 2018. Retrieved 6 June 2021.
- 1 2 3 4 5 Maruthainar, Nimalan; Bhumbra, Rej; Cannon, Steve (2018). "7. Orthopaedic oncology". In Ramachandran, Manoj (ed.). Basic Orthopaedic Sciences (2nd ed.). CRC Press. pp. 105–121. ISBN 978-1-4441-2098-1. Archived from the original on 2021-06-13. Retrieved 2021-05-04.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Roukhsi, Redouane (2013). "Unicameral Bone Cyst: A Case Report and Literature Review". International Journal of Medical Imaging. 1 (2): 19. doi:10.11648/j.ijmi.20130102.11. ISSN 2330-8303. Archived from the original on 2021-08-29. Retrieved 2022-03-14.
- 1 2 "Unicameral Bone Cysts - OrthoInfo - AAOS". www.orthoinfo.org. Archived from the original on 17 April 2021. Retrieved 8 June 2021.
- 1 2 3 4 5 Mehlman, Charles T. "Unicameral Bone Cyst". Medscape Reference. Archived from the original on 4 April 2020. Retrieved 17 March 2012.
- 1 2 Mascard, E.; Gomez-Brouchet, A.; Lambot, K. (February 2015). "Bone cysts: Unicameral and aneurysmal bone cyst". Orthopaedics & Traumatology: Surgery & Research. 101 (1): S119–S127. doi:10.1016/j.otsr.2014.06.031. Archived from the original on 2020-06-26. Retrieved 2020-06-23.
- 1 2 Noordin, Shahryar; Allana, Salim; Umer, Masood; Jamil, Mujahid; Hilal, Kiran; Uddin, Nasir (28 June 2018). "Unicameral bone cysts: Current concepts". Annals of Medicine and Surgery. 34: 43–49. doi:10.1016/j.amsu.2018.06.005. ISSN 2049-0801. PMID 30224948. Archived from the original on 29 August 2021. Retrieved 6 June 2021.
- 1 2 3 4 5 6 7 8 9 10 11 Hou, Hsien-Yang; Karl Wu; Chen-Ti Wang; Shun-Min Chang; Wei-Hsin Lei; Rong-Sen Yang (2011). "Treatment of Unicameral Bone Cyst: Surgical Technique". The Journal of Bone and Joint Surgery. American Volume. 93: 92–99. doi:10.2106/JBJS.J.01123.
- 1 2 Cohen, Jonathan (1970). "Etiology of Simple Bone Cyst". The Journal of Bone and Joint Surgery. 52 (7): 1493–97. Archived from the original on 29 August 2021. Retrieved 23 March 2012.
External links
| Classification | |
|---|---|
| External resources |
|