This article was co-authored by Pippa Elliott, MRCVS. Dr. Elliott, BVMS, MRCVS is a veterinarian with over 30 years of experience in veterinary surgery and companion animal practice. She graduated from the University of Glasgow in 1987 with a degree in veterinary medicine and surgery. She has worked at the same animal clinic in her hometown for over 20 years.
This article has been viewed 21,960 times.
Stomatitis is an infection that takes hold in the gums and the mouth lining at the back of a cat's mouth.[1] The true cause of the infection is unknown, although it is thought to relate to an abnormal reaction the immune system has to plaque, gingivitis, or other common oral infections. In order to diagnose stomatitis you will need to understand the symptoms usually exhibited by cats with this infection, the risk factors that increase its likelihood, and how a veterinarian will give a positive diagnosis.
Steps
Identifying the Signs of Stomatitis
-
1Pay attention to signs of oral pain.[2] Stomatitis causes pain and irritation at the back of the mouth. If your cat has stomatitis, it may be hesitant to eat its food, when it usually loves chowing down. If your cat is not eating as usual, then you should be suspicious that it may have a health problem that needs to be addressed.
- It may also paw at its face, attempting to get at the pain.
-
2Look for signs of weight loss and dehydration. The pain caused by stomatitis often causes cats to shy away from their food. If your cat has suddenly lost weight or shows signs of dehydration, which includes a loss of elasticity of the skin, sunken eyes, and cold paws, it may be due to a stomatitis infection in the mouth.
- Weight loss and dehydration can be signs of a variety of illnesses. Whatever the cause, they are symptoms that needs to be investigated by a veterinarian.
Advertisement -
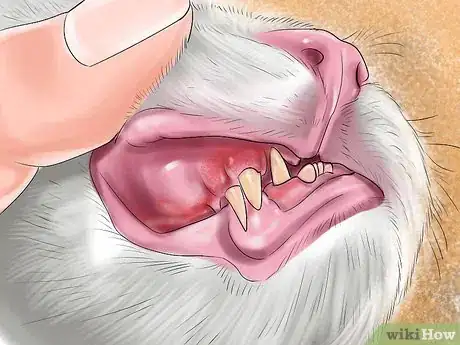
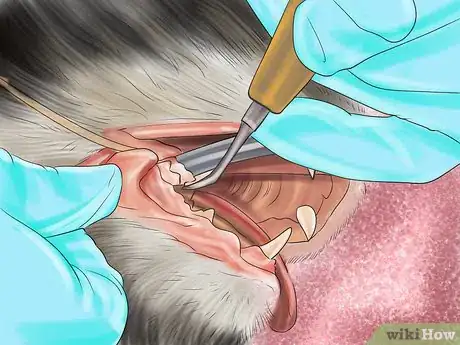
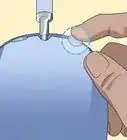
3Inspect your cat's gums. Cats with stomatitis have red, inflamed gums. It can be hard to see, as this inflammation usually occurs at the back of the mouth. If you are intent on looking, get the help of another person to hold the cat while you open the cat's mouth.
- If you notice the other symptoms of stomatitis you may want to leave the mouth inspection to a veterinarian, especially if your cat does not like you to get too close.
- In advanced cases of stomatitis, the infection will spread from the infected tooth around the mouth. Ulcers may develop around the mouth and blood may be visible in the cat's saliva.[3]
- While inspecting your cat's gums, take a moment to assess its breath as well. An infection in your cat's mouth can make your cat's breath very bad. A breath that smells different than usual can be an additional indicator of a stomatitis infection.
-
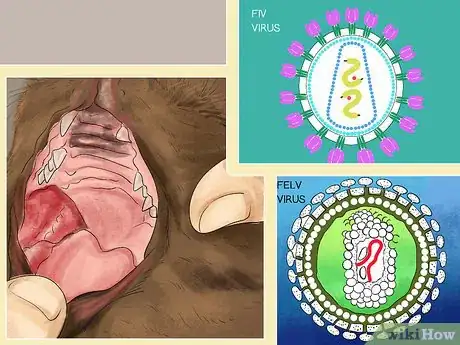
4Take risk factors into consideration. Cats with certain immune diseases, in particular feline immunodeficiency virus (FIV) and feline leukemia virus (FeLV), are more likely to get stomatitis. There is still more research needed to make it clear how the two diseases are connected, but there is a connection in rates of infection nonetheless.[4]
- If your cat has FIV then it is a good idea to keep on the look out for stomatitis and other opportunistic infections that are related to your cat's autoimmune disease.
Getting a Veterinary Diagnosis of Stomatitis
-
1Take your cat to its veterinarian. If you believe that your cat has the symptoms of stomatitis, then contact your veterinary office to get an appointment. Whether or not your cat's illness ends up being stomatitis, a cat that is having issues with eating and weight retention needs to be looked at by a veterinarian.[5]
- If you let your cat's symptoms persist, the infection could advance so much that the cat is unable to eat or drink at all due to the pain. This could get so bad that it could threaten the cat's life.[6]
-
2Tell the veterinarian about your cat's symptoms. Keep a record of your cat's symptoms, including what they are and when you first noticed them. Giving your veterinarian as much information as possible will help the vet to narrow down his or her diagnosis.
- Giving your veterinarian a correct accounting of your cat's symptoms is important. Include changes in its physical appearance, its bodily functions, as well as changes in behavior.
-
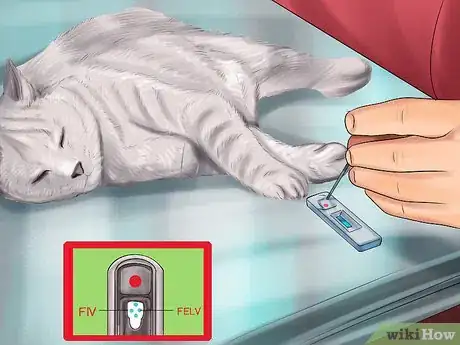
3Agree to veterinary testing. The only way to positively diagnose stomatitis is to do a biopsy of the affected tissue. The veterinarian will collect a small sample of affected tissue and the tissue will be assessed by the veterinarian or in a lab. This testing will allow the veterinarian to confirm if the infection is due to an overreaction of the cat's own immune system.
- The veterinarian may also test your cat for FIV or FeLV, as stomatitis is often associated with these infections.
Treating Stomatitis
-
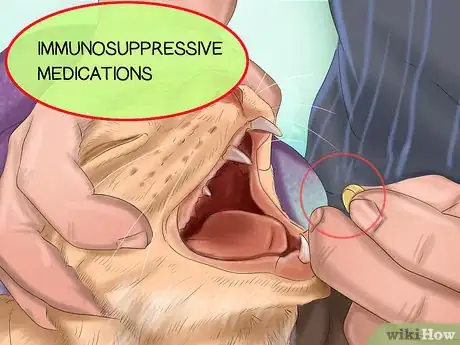
1Give your cat medication. Anti-inflammatory therapies are usually prescribed for cats with stomatitis. These may eliminate the infection or they may simply reduce the symptoms temporarily. The effectiveness depends on the cat and the level of infection that it is suffering from.[7]
- Medications used include both systemic antibiotics or immunosuppressive medications. Follow your veterinarian's directions for the medication, including how long to give them to your cat.
-
2Consider teeth removal as an option. If anti-inflammatory and antibiotic therapies don't work for your cat's infection, then the veterinarian may suggest removing some or all of the cat's teeth.[8] This is an extreme treatment and should be undertaken only if all other treatment options have proved unsuccessful.
- Removing the cat's teeth should only be done after other treatments are attempted. If your veterinarian suggests doing it before any other treatments, consider getting a second opinion.
- After your cat's teeth are removed it will need to be cared for at home while it recovers. You will need to give it antibiotics and pain killers for a week or two after surgery.[9]
- After recovery the cat may need some adjustment to its diet but should be fine otherwise. For instance, if all of your cat's teeth have been removed, it will likely need to eat wet food instead of dry food. Otherwise, it should regain weight and have a better quality of life than it would have with an infected mouth.
-
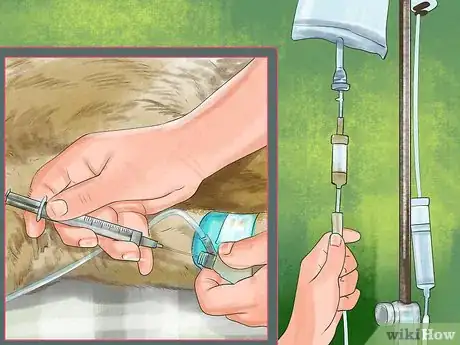
3Investigate the newest treatments. There is a new therapy for stomatitis that uses the cat's own stem cells to treat the infection. Cats that have had all other types of treatment, including all of their teeth removed, are the only animals that are eligible for this new treatment. You will have to find one of the few veterinary schools and veterinary hospitals that is performing this procedure to have your cat treated.
- Stem cell therapy requires that your cats own stem cells are harvested and then they are given back to the cat through an IV.
- This therapy has been shown to improve the health and quality of life of about seventy percent of study participants. However, the procedure is still in developmental stages.
References
- ↑ https://www.vet.cornell.edu/departments-centers-and-institutes/cornell-feline-health-center/health-information/feline-health-topics/gingivostomatitis
- ↑ https://penncurrent.upenn.edu/2012-11-15/latest-news/penn-vet-study-cat-teeth-could-help-humans
- ↑ https://www.vet.cornell.edu/departments-centers-and-institutes/cornell-feline-health-center/health-information/feline-health-topics/gingivostomatitis
- ↑ https://www.petmd.com/cat/conditions/mouth/c_ct_stomatitis
- ↑ https://www.petmd.com/cat/conditions/mouth/c_ct_stomatitis
- ↑ https://www.vet.cornell.edu/departments-centers-and-institutes/cornell-feline-health-center/health-information/feline-health-topics/gingivostomatitis
- ↑ https://penncurrent.upenn.edu/2012-11-15/latest-news/penn-vet-study-cat-teeth-could-help-humans
- ↑ https://penncurrent.upenn.edu/2012-11-15/latest-news/penn-vet-study-cat-teeth-could-help-humans
- ↑ http://www.veterinarypracticenews.com/Why-Teeth-Removal-is-Best-When-Your-Patient-Has-Feline-Stomatitis/
About This Article
Your cat may have feline stomatitis if you notice that it is hesitant to eat food or not eating as usual, since stomatitis causes irritation that makes eating painful. As a side effect of not eating, your cat may suddenly lose weight or display signs of dehydration like sunken eyes or cold paws. You should weigh your cat so you can compare its weight to a previous reading. Since stomatitis causes inflammation at the back of the mouth, try to inspect your cat’s gums to see if they are red and inflamed. To do this, enlist a friend to hold your cat while you open its mouth. If your cat is displaying symptoms of feline stomatitis, contact your vet so they prescribe treatment. For more advice from our Veterinary co-author, including how to keep an accurate record of your cat’s symptoms for the vet, keep reading!