This article was co-authored by Ni-Cheng Liang, MD. Dr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
There are 23 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 100% of readers who voted found the article helpful, earning it our reader-approved status.
This article has been viewed 42,617 times.
The thymus is a gland located behind the middle of your chest (sternum) and in front of your lungs. Its main function is to make thymosin to mature and produce immune cells (T cells) to help fight infections and prevent your immune cells from attacking your own body (a condition called autoimmunity). The thymus develops most of your T cells by puberty, after which the gland starts to shrink and is replaced with fat tissue. Thymomas are tumors that slowly grow from the lining of the gland and account for ninety percent of tumors found in the thymus. It is relatively rare with about 500 Americans diagnosed each year (most between the ages of 40 and 60).[1] By learning what symptoms of thymomas to look for and the diagnostic tests associated with the condition, you can know when to see a doctor and what to expect of the diagnosis process.
Steps
Recognizing Symptoms of a Thymoma
-
1Look for shortness of breath. The tumor can press against the windpipe (trachea) causing difficulty getting air into your lungs. Note if you easily become out of breath or feel like something is stuck in your throat to cause a choking feeling.[2]
- If shortness of breath happens after exercise activities note if you have a wheezing (high-pitched whistling sound) noise when breathing. This can be asthma.[3]
-
2Notice additional coughing. The tumor can irritate your lungs, trachea (windpipe), and the nerves associated with your cough reflex. Note if you have had a chronic cough from months to years with no relief from suppressants, steroids, and antibiotics.[4]
- If you have acid reflux from spicy, fatty, or acidic foods, it can lead to a chronic cough. If altering your diet reduces the cough, then it isn’t likely a thymoma.[5]
- If you live in or have traveled to an area with tuberculosis (TB) and have experienced a chronic cough, bloody sputum (blood mucus coughed up), night sweats, and a fever, then you may have TB for which you should still see a doctor immediately.
Advertisement -
3Note instances of chest pain. Due to the tumor pushing on the chest wall and heart, you may develop chest pain characterized by a pressure-like feeling and location only in the center of your chest. Also, you can develop pain behind the breastbone that may hurt when applying pressure to the area.[6] [7] [8]
- If you feel pressure-like chest pain and have sweating, palpitations (feel like your heart is jumping out of your chest), fever, or chest pain when moving or breathing, then you may have an underlying lung or heart disease.[9] Regardless of the root cause, you should see a doctor for these symptoms.
-
4Watch for trouble swallowing. The thymus can grow and push against the esophagus, causing difficulty swallowing.[10] Note if you have trouble swallowing meals or you recently switched to a more liquid diet because it's easier. The trouble may also feel like a choking sensation.
-
5Weigh yourself. Because the thymus tumor can become cancerous and spread throughout the body (very rarely), you may experience weight loss due to the increased needs of the cancer tissue.[11] Check your current weight against an older reading.
- If you experience unintentional weight loss without any known reason, check with your healthcare provider. Many cancers have weight loss as a symptom.
-
6Examine for superior vena cava syndrome. The superior vena cava is a large vessel that collects the returning blood from the veins of the head, neck, upper extremities, and upper torso back in the heart. When this vessel becomes obstructed it backs up the blood from these areas from entering the heart. This leads to:[12]
- Swelling of the face, neck, and upper body. Note if the upper part of your body looks more red or flushed.
- Dilated veins in the upper body. Look at the veins in your arms, hands, and wrist to see if they look more prominent or dilated. These are usually the dark lines or tunnels we see on the hands and arms.
- Headaches due to dilated veins supplying the brain.
- Dizziness/light headedness. Because blood is backed up, the heart and brain receive less oxygenated blood. When your heart pumps less blood to the brain or when your brain doesn't receive enough oxygenated blood, you feel light headed or dizzy and may fall. Laying down helps remove the force of gravity your blood has to fight to supply your brain.[13]
-
7Note symptoms consistent with myasthenia gravis (MG). MG is the most common paraneoplastic syndrome, which is a set of symptoms that are caused by cancer. With MG, your immune system forms antibodies that block the chemical signals that tell your muscles to move. This causes muscle weakness throughout the body. About 30 to 65 percent of people with thymomas also have myasthenia gravis. Look for:[14] [15]
- Double or blurred vision
- Drooping eyelids
- Trouble swallowing food
- Shortness of breath due to weakness in the chest muscles and/or diaphragm
- Slurred speech
-
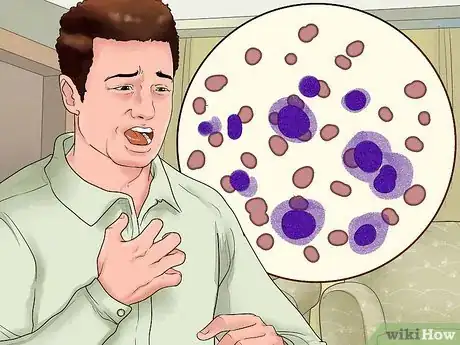
8Look for symptoms of red blood cell aplasia. This is the destruction of premature red blood cells, which leads to symptoms of anemia (low red blood cells). Reduced RBC will lead to lack of oxygen throughout the body. This occurs in about 5 percent of thymoma patients. Look for:[16]
- Shortness of breath
- Fatigue
- Dizziness
- Weakness
-
9Examine for symptoms of Hypogammaglobulinemia. This is when your body lowers production of infection-fighting gamma globulins (protein antibodies). About five to ten percent of thymoma patients develop hypogammaglobulinemia. About ten percent of patients with hypogammaglobulinemia have a thymoma.[17] Together with a thymoma, it is called Good’s syndrome. Look for:[18]
- Recurrent infections
- Bronchiectasis, which includes symptoms such as a chronic cough, large amounts of spit that may contain foul-smelling mucus, shortness of breath and wheezing, chest pain, and clubbing (the flesh under your fingernails and toenails gets thicker).[19] [20]
- Chronic diarrhea[21]
- Mucocutaneous candidiasis, which is a fungal infection that can cause thrush (an oral infection causing white patches or milk curd-looking growths on the tongue).[22]
- Viral infections, including the herpes simplex virus, cytomegalovirus, varicella zoster (shingles), and human herpes 8 (kaposi's sarcoma), which is an underlying skin cancer usually associated with AIDS.[23]
Diagnosing a Thymoma
-
1See your doctor. Your doctor will collect a detailed medical history, including family history and symptoms. He or she will also ask questions based on thymoma symptoms, including those related to myasthenia gravis, red cell aplasia, and hypogammaglobulinemia symptoms. Your doctor may feel for fullness in the middle lower neck for overgrowth of the thymus.[24]
-
2Have your blood drawn. There are no lab tests for thymoma diagnosis, but there is a blood test to detect myasthenia gravis (MG) called anti-Cholinesterase antibody (AB).[25] [26] MG is so common in those with thymomas that it is considered a solid indicator before more expensive testing. About 84% of people under 40 with a positive anti-Cholinesterase AB test have thymomas.[27]
- Before operating to remove the thymoma, your doctor will also treat the MG because if left untreated, it can cause problems with anesthesia during surgery, such as respiratory failure.[28]
-
3Submit to an x-ray. To visualize a tumor mass, your physician will first order an x-ray of the chest. The radiologist will look for a mass or shadow near the center of the chest on the lower neck. Some thymomas are small and will not show up on the x-ray. If your doctor is still suspicious or if an abnormality appears on the chest x-ray, he or she may order a CT scan.[29]
-
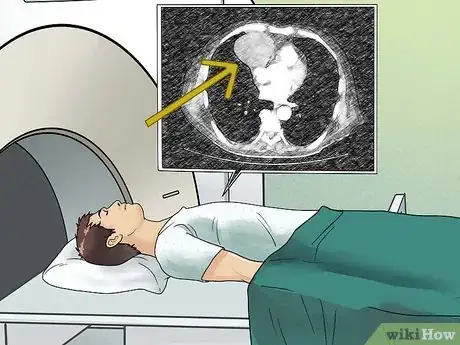
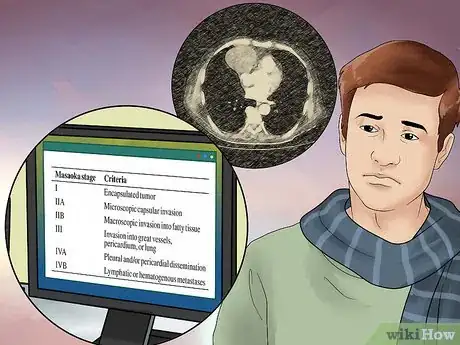
4Undergo a CT scan. A CT scan will take multiple, detailed images in cross sections from the lower part to the upper part of your chest. You may be given a contrast dye to outline the structures and blood vessels in your body. The images will give a more detailed understanding of any abnormalities, including the staging of the thymoma or if it has spread.[30] [31]
- If contrast was given, you may be advised to drink plenty of fluids to flush it out.[32]
-
5Undergo an MRI. An MRI will use radio waves and magnets to produce a series of very detailed images of your chest on a computer screen. A contrast material called gadolinium is often injected into a vein before the scan to better see details. MRI of the chest may be done to look more closely at the thymoma or when you can't tolerate or are allergic to the CT contrast. MRI images are also particularly useful in looking for cancer that may have spread to the brain or spinal cord.[33]
- MRIs are very loud and some are closed meaning that you will be inserted lying down in a large cylindrical space. This can give the sensation of claustrophobia (fear of enclosed spaces) to some people.
- The test may take up to an hour to complete.[34]
- If you were given contrast, you may be advised to drink plenty of fluids to flush it out.[35]
-
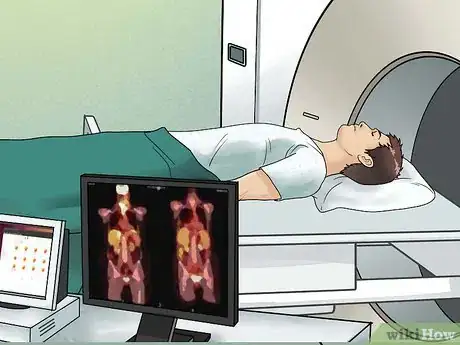
6Submit to a PET scan. This is a scan that uses a radioactive atom in glucose (type of sugar) that attracts to the thymoma. The cancer cells take up the radioactive substance and a special camera is used to create a picture of areas of radioactivity in the body. The picture is not finely detailed like a CT or MRI scan, but it can provide helpful information about your whole body. This test can help determine if a tumor seen on an image is actually a tumor or not or if the cancer has spread to other parts of the body.[36]
- Doctors use combined PET/CT scans more often than PET scans alone when looking at thymomas. This lets the doctor compare areas of higher radioactivity on the PET scan with the more detailed images on the CT scan.[37]
- You will be given either an oral preparation or injection of the radioactive glucose. You will wait thirty to sixty minutes for your body to absorb the material. You'll need to drink plenty of fluids after to help flush the tracer from your body.[38]
- The scan will take approximately thirty minutes.[39]
-
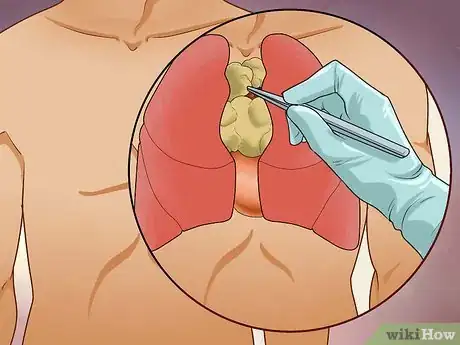
7Allow your doctor to perform a fine needle biopsy. Using a CT scan or ultrasound machine for visual guidance, your doctor will insert a long, hollow needle into your chest and into the suspected tumor. He or she will remove a small sample of the tumor to examine it under a microscope.[40]
- If you are taking blood thinners (coumadin/warfarin), your doctor may ask you to stop days before the exam and not to eat or drink the day of the procedure. If they decide to use general anesthesia or IV sedation, you may be asked to fast the day before the procedure as well.[41]
- A possible downside of this test is that it might not always get enough of a sample to make an accurate diagnosis or allow the doctor to get a good sense of the extent of the tumor.[42]
-
8Have the tumor biopsied after surgery. Sometimes your doctor may do a surgery biopsy (remove the tumor) without a needle biopsy if the evidence of thymoma is strong (lab tests and imaging tests). Other times a doctor will need to perform a needle biopsy first to confirm it is a thymoma. The specimen is sent to the lab after surgery to confirm the diagnosis.[43]
- The exam preparation (fasting, etc.) is similar to that of a needle biopsy, except an incision will be made in the skin to gain access to the tumor to remove it.
-
9Have the thymoma staged and treated. The stage of the tumor refers to the extent of spread to other organs, tissues and distant sites of the body. Therefore, having the thymoma staged is an essential part of determining the best course of treatment. The most commonly used staging method for thymomas is the Masaoka staging system.[44]
- Stage I is an encapsulated tumor without microscopic or gross invasion. Surgical excision is the treatment of choice
- Stage II is a thymoma with a macroscopic invasion of the mediastinal fat or pleura or the microscopic invasion of the capsule. Treatment is usually a complete excision with or without postoperative radiation therapy in order to reduce the incidence of recurrence.
- Stage III is when the tumor has invaded the lungs, great vessels, and the pericardium. Complete surgical excision is necessary together with postoperative radiation therapy so that recurrence will not occur.
- Stage IVA and IV B In these final stages, there is pleural or metastatic spread. The treatment is a combination of surgical debulking, radiation, and chemotherapy.
Expert Q&A
-
QuestionWhat are the symptoms of having a thymoma?
 Ni-Cheng Liang, MDDr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
Ni-Cheng Liang, MDDr. Ni-Cheng Liang is a board certified Pulmonologist and the Director of Pulmonary Integrative Medicine at Coastal Pulmonary Associates affiliated with the Scripps Health Network in San Diego, California. She also serves as a Voluntary Assistant Professor of Medicine at the University of California San Diego School of Medicine while volunteering for the UCSD Medical Student-Run Free Clinic for uninsured patients. With over 15 years of experience, Dr. Liang specializes in pulmonary and respiratory medical concerns, mindfulness teaching, physician wellness, and integrative medicine. Dr. Liang received her Doctor of Medicine (MD) from the University of Maryland School of Medicine. Dr. Liang was voted as a San Diego Top Doctor in 2017 and 2019. She was also awarded the 2019 American Lung Association San Diego Lung Health Provider of the Year.
Board Certified Pulmonologist You might notice pain or pressure in the area where the thymoma is. If the thymoma is especially big, it might compress some of the structures around it. Keep in mind that in many cases, the thymoma is incidentally found on a CT test.
You might notice pain or pressure in the area where the thymoma is. If the thymoma is especially big, it might compress some of the structures around it. Keep in mind that in many cases, the thymoma is incidentally found on a CT test.
Warnings
- While this article offers information regarding the diagnosis of a thymoma, it should not be taken as medical advice. Always consult with your physician if you develop symptoms that you believe may indicate a thymoma.⧼thumbs_response⧽
References
- ↑ https://www.mskcc.org/cancer-care/types/thymoma-other-thymic-tumors/about-thymoma-thymic-tumors
- ↑ http://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=34&ContentID=18785-1
- ↑ http://www.aaaai.org/conditions-and-treatments/library/asthma-library/asthma-and-exercise.aspx
- ↑ Agrawaal KK. et al. Chronic cough in Thymoma. Journal of Nepal Medical association. 2010;49(178):164-6.
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3740808/
- ↑ http://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=34&ContentID=18785-1
- ↑ Meghani M, Siddique M, Sicat M. Thymoma presenting as chest pain. American Journal of the Medical Sciences. vol 344. #5. Nov 2012.
- ↑ Ni-Cheng Liang, MD. Board Certified Pulmonologist. Expert Interview. 18 June 2021.
- ↑ https://www.mountsinai.org/health-library/symptoms/chest-pain
- ↑ http://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=34&ContentID=18785-1
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-signs-symptoms
- ↑ Nickloes T. Superior Vena Cava Syndrome: Pathophysiology. Medscape. Oct 10, 2014.
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-signs-symptoms
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-signs-symptoms
- ↑ Riedel R, Burfeind W. Thymoma: Benign Appearance, Malignant Potential. The Oncologist.2006;11:887–894
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-signs-symptoms
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-signs-symptoms
- ↑ Kelleher P, Misbah SA. What is Good’s syndrome? Immunological abnormalities in patients with thymoma. Journal of Clinical Pathology. 2003;56:12-16
- ↑ http://www.nhlbi.nih.gov/health/health-topics/topics/brn
- ↑ https://www.lung.org/lung-health-diseases/lung-disease-lookup/bronchiectasis/symptoms-diagnosis
- ↑ Qu J. et al. Good Syndrome, a Rare Cause of Refractory Chronic Diarrhea and Recurrent Pneumonia in a Chinese Patient after Thymectomy. Clinical & Vaccine Immunology. July 2013 vol. 20 no. 7 1097-1098.
- ↑ Kelleher P, Misbah SA. What is Good’s syndrome? Immunological abnormalities in patients with thymoma. Journal of Clinical Pathology. 2003;56:12-16
- ↑ Kelleher P, Misbah SA. What is Good’s syndrome? Immunological abnormalities in patients with thymoma. Journal of Clinical Pathology. 2003;56:12-16
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://emedicine.medscape.com/article/1171206-workup
- ↑ http://emedicine.medscape.com/article/1171206-workup
- ↑ Abel M, Eisenkraft J. Anesthetic Implications of Myasthenia Gravis. The Mount Sinai Journal of Medicine. January/March 2002. Vol. 69. Nos. 1 & 2.
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ Ni-Cheng Liang, MD. Board Certified Pulmonologist. Expert Interview. 18 June 2021.
- ↑ http://www.mayoclinic.org/tests-procedures/ct-scan/basics/how-you-prepare/prc-20014610
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.mayoclinic.org/tests-procedures/mri/basics/how-you-prepare/prc-20012903
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.mayoclinic.org/tests-procedures/pet-scan/basics/what-you-can-expect/prc-20014301
- ↑ http://www.mayoclinic.org/tests-procedures/pet-scan/basics/what-you-can-expect/prc-20014301
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.mayoclinic.org/tests-procedures/needle-biopsy/basics/how-you-prepare/prc-20012926
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-diagnosis
- ↑ http://www.cancer.org/cancer/thymuscancer/detailedguide/thymus-cancer-staging
About This Article
You may have a thymoma if you become easily out of breath, have a cough that lasts more than 3 to 4 weeks, or experience pain in the centre of your chest, since these symptoms can be the result of a thymoma pressing against or irritating your windpipe and chest wall. Another symptom of a thymoma is unintentional weight loss without any known reason, so it’s a good idea to weigh yourself regularly to see if you’re losing weight. Since 30 to 65 percent of people suffering from a thymoma also have myasthenia gravis, a condition which causes muscle weakness, look out for symptoms like double or blurred vision, drooping eyelids, and slurred speech. If you think you may have a thymoma, book an appointment to see your doctor to get a proper diagnosis. For more advice from our Medical co-author, including how to recognize when a thymoma is obstructing a blood vessel, keep reading!


































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...