This article was co-authored by Courtney Fose, RD, MS. Courtney Fose is a Registered Dietitian and Certified Nutrition Support Clinician at the University of Arkansas for Medical Sciences. She has worked as a Dietitian since 2009, and received her MS in Clinical Nutrition from the University of Arkansas in 2016.
There are 13 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 21,976 times.
People get cholesterol tests in order to assess their risk of heart disease. As cholesterol levels indicate the amount of lipids—that is, different kinds of fats—in your blood, a high result means that a person will need to take measures to lower their cholesterol and get re-tested in the future. If you’re considering getting a cholesterol test, or your doctor has recommended one, you should evaluate your candidacy for the test, find out what preparatory procedures are expected of you, and fast according to the doctor’s recommendations.[1]
Steps
Getting Ready for Your Test
-
1Determine if you are a candidate for cholesterol testing. Most doctors recommend that all adults over the age of 18 get their cholesterol checked every five years. You might want to undergo more frequent testing, though, if you fall into a higher-risk category. Factors such as a family history of heart disease, obesity, lack of physical activity, diabetes, and smoking can exacerbate one’s risk of heart disease, so you should be particularly vigilant about cholesterol if you possess one of these qualities.[2]
- Children are at a lower risk of high cholesterol, but it’s still recommended that a child receive one screening test between the ages of 9 and 11. Teenagers between 17 and 21 years of age should also get a cholesterol test.[3]
-
2Determine an appropriate day and time for your test. While fasting is generally no longer required before a cholesterol test, there are still some considerations, such as prior surgeries, infections, pregnancy, or illnesses, which you should take into account when scheduling. For example, one should wait at least two months after a heart attack, pregnancy, or major surgery in order to ensure optimally accurate results.[4]Advertisement
-
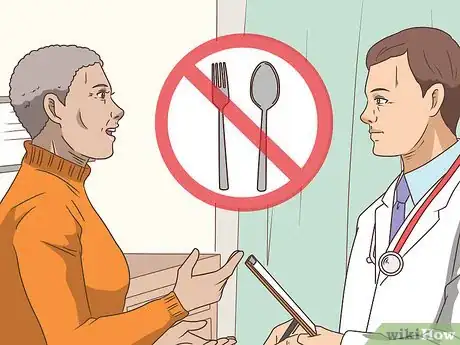
3Ask your doctor if you should fast before the screening. While non-fasting lipid testing is quickly becoming the standard throughout the world, there are some specific tests and scenarios when your doctor might stipulate fasting. For example, some medical professionals argue that triglyceride monitoring requires fasting for more accurate results.[5]
- If your doctor has recommended it, you will need to abstain from eating anything for twelve hours before your test. Additionally, don’t drink any fluids but water.[6]
-
4Don't drink alcohol or eat fatty foods before your test. Alcohol and fatty or sugary foods can spike your cholesterol levels significantly in the hours following consumption, so you should avoid them in order to receive the most accurate results on your cholesterol test. Some particularly fatty foods to avoid include fried and greasy dishes, fatty steak or pork, and cheesy items.
- Wine can also boost your 'good cholesterol' levels, distorting your cholesterol reading results even more.
-
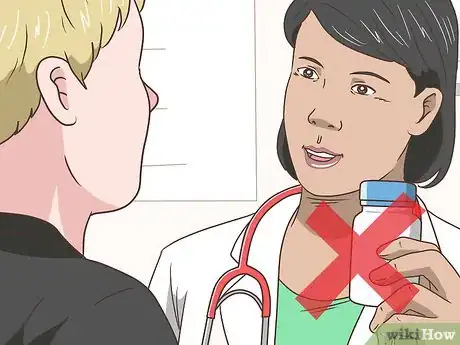
5Ask your doctor about any regular medications you should discontinue. Some medications, such as oral corticosteroids, can significantly affect the results of a cholesterol test, so your doctor might want you to discontinue use for a day or two before the screening. Draw up a full list of the medications you take regularly or semi-regularly and give it to your doctor at least a week before the exam.[7]
- Don't forget to include any herbal or dietary supplements you take in this list.[8]
Ensuring Good Results for Your Next Test
-
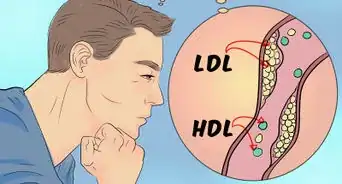
1Exercise for 30 minutes every day. Whether your cholesterol test results came out high or you're just trying to maintain your good levels, you can help ensure a positive result at your next lipid test by making some basic lifestyle changes. Perhaps most importantly, physical activity is essential to raising levels of high-density lipoproteins (HDL)—or “good cholesterol” as it is often called. Aim for at least 30 minutes of aerobic exercise, such as brisk walking, cycling, jogging, or swimming, per day.[9]
- Daily exercise can also be invaluable for managing one’s weight. This is important for lowering your cholesterol levels, as excess weight has been linked to high cholesterol and heart disease as a risk factor.
-
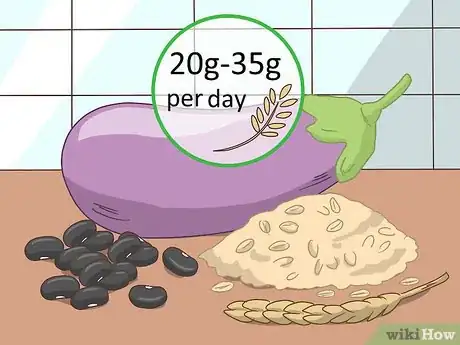
2Eat foods rich in soluble fiber. Soluble fiber is important to a cholesterol-conscious diet, as it binds to cholesterol in the digestive tract and gets it out of the body. It’s recommended that you consume at least 20-35 grams of fiber a day, with five to ten grams of that being of the soluble variety.[10]
- Some fiber-rich foods include oats barley, oat bran, beans, and eggplant.[11]
-
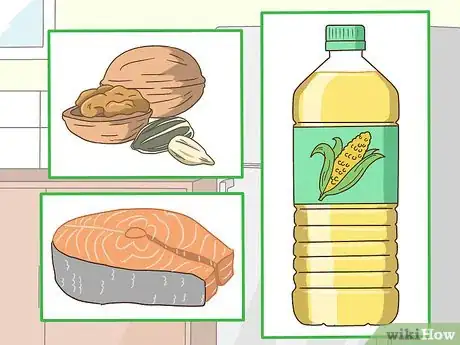
3Consume polyunsaturated fats. Including polyunsaturated fats in your diet can directly lower your low-density lipoproteins (LDL)—or “bad cholesterol” levels.[12] Eat plenty of foods rich in these ‘good fats’—for example, nuts, vegetable oils, and fatty fish—and you may be able to get better results on your very next cholesterol test without taking any medication or supplements.
- Also be sure to avoid saturated fats and trans fats! Trans and saturated fats have been linked to heart disease and high ‘bad cholesterol’ levels, so keep them out of your diet at all costs. Trans fats are designed to extend shelf life, so you’ll find them mostly in fast food and highly processed products.[13]
-
4Quit smoking. Smoking is one of the risk factors most strongly correlated to high cholesterol and heart disease. If you’re a smoker, consider quitting this highly addictive habit for a plethora of health benefits. In addition to improving respiratory health and decreasing your chances of contracting cancer, you’ll also improve your HDL cholesterol levels.[14]
- The cardiovascular benefits of quitting are so significant that it halves your risk of heart disease after just one year.[15]
-
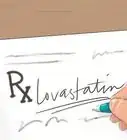
5Ask your doctor if you should take a cholesterol-lowering drug. If your doctor deems it prudent, you might be prescribed a regular medicine to help lower your cholesterol. Statins, bile acid sequestrants, nicotinic acid, fibric acids, and cholesterol absorption inhibitors are all popular drugs with demonstrated success in this capacity.[16]
- Even if you end up taking a cholesterol lowering drug, you’ll still need to make corresponding lifestyle changes, such as performing daily exercise and monitoring your diet.
References
- ↑ https://www.cdc.gov/cholesterol/cholesterol_screening.htm
- ↑ https://www.cdc.gov/cholesterol/checked.htm
- ↑ https://www.cdc.gov/cholesterol/checked.htm
- ↑ http://my.clevelandclinic.org/health/articles/lipid-blood-tests
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/25316740
- ↑ https://wexnermedical.osu.edu/heart-vascular/conditions-treatments/cholesterol-test
- ↑ http://www.nhs.uk/chq/Pages/medication-before-a-blood-test.aspx
- ↑ https://wexnermedical.osu.edu/heart-vascular/conditions-treatments/cholesterol-test
- ↑ https://www.cdc.gov/cholesterol/prevention.htm
- ↑ http://www.health.harvard.edu/heart-health/11-foods-that-lower-cholesterol
- ↑ http://www.health.harvard.edu/heart-health/11-foods-that-lower-cholesterol
- ↑ https://www.hsph.harvard.edu/nutritionsource/what-should-you-eat/fats-and-cholesterol/types-of-fat/
- ↑ http://www.health.harvard.edu/heart-health/how-to-lower-your-cholesterol-without-drugs
- ↑ https://www.nhs.uk/conditions/high-cholesterol/how-to-lower-your-cholesterol/
- ↑ https://www.nhs.uk/conditions/high-cholesterol/how-to-lower-your-cholesterol/
- ↑ https://www.nhlbi.nih.gov/health/resources/heart/heart-cholesterol-hbc-what-html





























































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...