This article was medically reviewed by Janice Litza, MD. Dr. Litza is a board certified Family Medicine Physician in Wisconsin. She is a practicing Physician and taught as a Clinical Professor for 13 years, after receiving her MD from the University of Wisconsin-Madison School of Medicine and Public Health in 1998.
There are 7 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 68,171 times.
High cholesterol rarely presents with visible signs and symptoms. There are rare cases in which there may be physical signs, such as around the eyes and/or over the tendons, but this occurs for the minority of people. Normally, high cholesterol must be screened for and detected via a blood test. If you do in fact get diagnosed with high cholesterol, your doctor can advise you as to an appropriate treatment plan.
Steps
Recognizing Signs and Symptoms
-
1Look out for yellow patches around the skin of your eyelids.[1] These are called "xanthelasma palpebrarum." They may be associated with a certain type of high cholesterol called familial hypercholesterolemia (Type IIa hyperlipoproteinemia).
- These yellow patches which may or may not be raised off the skin.
- They tend to be located above or below the eye, and often in both locations.
- They are a sign of cholesterol deposition under the skin.
- Note, however, that this only occurs in certain high cholesterol syndromes, and that the majority of cases of high cholesterol present with no signs or symptoms at all.
-
2Look for yellowish deposits (lumps) in your tendons.[2] These are called "xanthomata," and they occur particularly in the tendons of the fingers. If they occur in the palm, knees, and/or elbows, they may be associated with Type III hyperlipidemia.
- These often appear as bumps over the knuckles in your hands.
- There are often many of them present, and in more than one area at once.
- Again, this only occurs in certain high cholesterol syndromes, and the majority of cases of high cholesterol present with no signs or symptoms.
Advertisement -
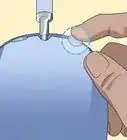
3Watch for a white or gray discoloured "arc" in your eye.[3] If you have this, it is called "circumferential arcus." The part of the eye that is affected is the cornea, which is the transparent outer covering of the eye. It is easiest to see these lesions over the white area of the eye, as the discoloration tends to be most apparent there.
-
4Be aware that elevated cholesterol usually presents with no signs or symptoms. The challenging thing when it comes to detecting elevated cholesterol levels is that almost everyone presents with no visible signs or symptoms. Therefore, doctors rely on screening blood tests to pick up high cholesterol, and to prescribe appropriate treatment as needed.
- Therefore, even if you have no signs or symptoms, it is advisable to ask your doctor to screen your cholesterol levels at least every five years with a simple blood test (and more frequently if you have a family history of high cholesterol and/or other risk factors).
-
5Know the risk factors for high cholesterol.[4] Your chance of developing high cholesterol at some point in your life is higher in proportion to your risk factors. The more risk factors you have, the more frequently you should receive screening blood tests from your doctor. Risk factors to be aware of include:
- Eating an unhealthy diet high in fat and sugar
- Having a large waist circumference
- Being overweight or obese
- Living a sedentary life
- Smoking
- Being diagnosed with diabetes or cardiovascular (heart and blood vessel) disease
Knowing What to Look for in Medical Tests
-
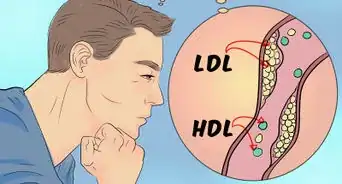
1Ask your doctor for a lipid panel. Because high cholesterol almost always presents with no signs or symptoms, the fastest and easiest way to detect it is via a blood test. Specifically, a "lipid panel" evaluates your HDL ("good") cholesterol, your LDL ("bad") cholesterol, your total cholesterol, and your triglyceride levels (another type of fat).
- It is a fasting blood test, meaning that you cannot eat or drink fluids other than water for nine to 12 hours prior to the blood test.
- You may eat and/or drink immediately following the blood test.
- For this reason, most people do the test first thing in the morning (following an overnight "fast"), and eat breakfast after the blood test is over.
-
2Learn how to interpret your blood test results.[5] When your blood test results come back from the lab, you will want to know whether they are concerning or not. Here's how to interpret your results:
- HDL ("good") cholesterol: below 40mg/dL for men or 50mg/dL for women is poor, 50–59mg/dL is better, and above 60mg/dL is best. Ironically, HDL cholesterol is the one value where the higher numbers are more desirable.
- LDL ("bad") cholesterol: below 70–129mg/dL is desirable (the recommended value for you will depend on your overall health and other cardiovascular risk factors). 130–159mg/dL is considered borderline high, and above 160mg/dL is high.
- Total cholesterol: below 200mg/dL is desirable, 200–239mg/dL is borderline high, and above 240mg/dL is high.
- Triglycerides: below 150mg/dL is desirable, 150–199mg/dL is borderline high, and above 200mg/dL is high.
-
3Be patient when getting rechecked. If you make changes to improve your cholesterol, you may be eager to get your levels rechecked to see how your new, healthier lifestyle has impacted your cholesterol. It can, however, take between two and three months to see the lab changes from diet or medication. Make sure allow your body time to adjust before you get retested and become frustrated or discouraged.
-
4Receive screening at regular intervals.[6] Because there is essentially no way to detect high cholesterol other than through blood tests, you will need repeat screening blood tests throughout your life. It is generally recommended to have your cholesterol levels tested once every five years if your initial test comes back normal. If your initial test is borderline high or high, or if you have risk factors or other medical conditions that may predispose you to elevated cholesterol, your doctor will likely advise that you have more frequent screening blood tests.
- For children, an initial test is recommended between the ages of nine and 11. A second test is recommended between the ages of 17–21.
- Screening can then continue every five years thereafter, unless otherwise indicated.
Treating High Cholesterol
-
1Make lifestyle changes.[7] Depending upon how high your cholesterol levels are, your doctor will suggest lifestyle changes with or without medications to help lower your levels. If your cholesterol levels are only borderline high, lifestyle changes alone may be enough to get you back in the normal range. Positive lifestyle changes you can make include:
- Incorporating more aerobic exercise — three to five sessions of thirty minutes or more each week is recommended. Aerobic exercise includes things like swimming, biking, jogging, or brisk walking — anything that elevates your heart rate continuously for thirty minutes or more. Exercise specifically raises your HDL levels (good cholesterol), which helps to improve your overall cholesterol profile.
- Eating a healthier diet. Specifically, consuming more fruits and vegetables and reducing fat consumption can help to lower your cholesterol levels. Fiber in particular is one of the mainstay dietary changes to lower cholesterol, so try increasing sources of soluble fiber, such as oatmeal, beans, peas, rice bran, barley, citrus fruits, and strawberries.[8]
- Losing weight if you are overweight or obese — talk to your doctor about healthy weight loss goals for you, and where your ideal body weight should be based on your height and build.
-
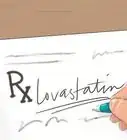
2Take a statin medication.[9] If lifestyle changes alone are insufficient to adequately reduce your cholesterol levels, your doctor will recommend that you begin medical treatment. The usual first-line medication is a "statin," such as Atorvastatin (Lipitor).
- Once you begin medical treatment, your doctor will advise follow-up blood tests to monitor your cholesterol profile and the degree of improvement.
-
3Continue with treatment for the rest of your life.[10] If you have been diagnosed with high cholesterol, you will most likely need to continue with positive lifestyle changes and medical treatment for the rest of your life. If you stop treatment for any reason, your high cholesterol levels are likely to return.
- If you find that side effects of medication are a concern for you, you can ask your doctor for an alternative medication to try, as there are plenty of treatment options for elevated cholesterol.
References
- ↑ http://www.skinsight.com/adult/xanthelasmaPalpebrarum.htm
- ↑ http://www.pcds.org.uk/clinical-guidance/xanthomata
- ↑ http://www.mayoclinic.org/arcus-senilis/expert-answers/faq-20058306
- ↑ http://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/symptoms-causes/dxc-20181874
- ↑ http://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/diagnosis-treatment/diagnosis/dxc-20181913
- ↑ http://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/diagnosis-treatment/diagnosis/dxc-20181913
- ↑ http://www.uptodate.com/contents/high-cholesterol-treatment-options-beyond-the-basics
- ↑ http://www.webmd.com/heart-disease/fiber-and-cholesterol
- ↑ http://www.uptodate.com/contents/high-cholesterol-treatment-options-beyond-the-basics



































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...