This article was medically reviewed by Erik Kramer, DO, MPH. Dr. Erik Kramer is a Board-Certified Primary Care Physician at the University of Colorado. With over 15 years of experience, his clinical interests include obesity and weight management, diabetes care, and preventive care, as well as embracing a holistic approach to primary care. He received his Doctorate in Osteopathic Medicine (D.O.) from the Touro University Nevada College of Osteopathic Medicine and completed his residency at Central Maine Medical Center. Dr. Kramer is a Diplomate of the American Board of Obesity Medicine.
There are 18 references cited in this article, which can be found at the bottom of the page.
This article has been viewed 12,242 times.
Eosinophilic esophagitis (EoE) is a chronic inflammatory condition where your immune system attacks your esophagus, which often results in low levels of white blood cells called eosinophils. If you have an allergy to certain foods or airborne allergens, your body might release lots of white blood cells into the lining of your esophagus as protection. Unfortunately, that’s what causes the inflammation that’s typical of EoE. It’s hard to diagnose because it shares a lot of the same symptoms as acid reflux and GERD, but there are ways to know for sure. In most cases, it's not serious and you can manage it by changing what and how you eat.
Steps
Altering Your Diet
-
1Eliminate any foods that trigger acid reflux. Don't eat foods that are high in fat, spice, or salt like fried foods, fast food, pizza, bacon, sausage, cheese, and pepper (black, white, and cayenne). Stay away from citrus fruits and acidic condiments like oranges, grapefruit, and tomato-based products because these cause your stomach to produce more gastric acid.[1]
- You can eliminate only the foods that you know are triggers for you or stick to a completely acid reflux-friendly diet.
- You don’t have to stop eating acidic foods forever. However, if you have GERD, it’ll definitely help to avoid them or eat only small amounts every once in a while.
- Chocolate, peppermint, and carbonated drinks are also common triggers for some people, so limit your intake or avoid them altogether.
- Acid reflux doesn't directly cause EoE, but it thins the protective layer of mucus lining your esophagus, making it easier for food allergens to penetrate the walls of your esophagus and cause an inflammatory response.
Tip: Try keeping a food symptom diary for at least 1 week to find out which foods trigger acid reflux for you. Write down the time you ate, what you ate, how much you ate, and any symptoms that may have crept up 30 minutes to 1 hour after eating.[2]
-
2Do a 6-food elimination diet to avoid possible allergens. Dairy, eggs, wheat, soy, peanuts (or other tree nuts), and fish (or shellfish) are the most common allergens that can lead to EoE, so stop eating them to see if it makes a difference. It's hard to cut out that many food options at once, so work with your doctor to come up with a meal plan that satisfies your needs. Be prepared to follow the elimination diet for 4 to 6 weeks.[3]
- Seafood and nuts are less common triggers of EoE, so you may be able to get away with eating those and only avoiding the other 4 foods.
- Your doctor may only suggest you cut out 1 food at a time to find out which one you're allergic to. But if you're having symptoms of EoE, they may tell you cut them all out at the same time until the inflammation subsides.
- Cutting out possible allergens helps prevent your body from releasing eosinophils (a type of white blood cell that is released by your immune system) into your esophagus.
- After you know what food is causing the reaction, you'll need to avoid it indefinitely. But the good news is that you can start to reintroduce the other foods 4-6 weeks after starting the diet.
Advertisement -
3Eat high-fiber foods to keep you full. Load up on healthy whole grains, root veggies, and green veggies to keep you feeling full so you're not tempted to overeat. Eat them slowly and be sure to chew them well so you know when you're ready to stop eating.[4]
- Oatmeal, couscous, brown rice, sweet potatoes, beets, asparagus, green beans, and broccoli are great sources of fiber. As a plus, they’re all alkaline foods, which means they probably won’t trigger acid reflux.
-
4Fill up on foods that contain lots of water. Snack on healthy fruits and veggies like celery, watermelon, lettuce, and cucumber to help dilute and weaken gastric acid in your stomach. If you need to lose weight, these are especially great foods to munch on![5]
- Diluting the acid in your stomach will make it less likely that you'll feel the burn of acid reflux after eating.
-
5Limit or avoid drinking alcohol. If you already have acid reflux or GERD and know that alcohol is a huge trigger for you, avoid it altogether. Enjoy your social hours with alcohol-free cocktails or tea instead.[6]
- If gluten causes acid reflux or an allergic reaction for you, switch to gluten-free beer or avoid it altogether.
- If alcohol isn't a trigger for you, limit your intake to 1 or 2 drinks per day (1 if you're a woman, 2 if you're a man).
- A single drink is equal to 12 fluid ounces (350 mL) of beer, 5 fluid ounces (150 mL) of wine, or 1.5 fluid ounces (44 mL) of distilled spirits.
Making Lifestyle Changes
-
1Lose weight if necessary to be within a healthy range for your age and height. Cut back on calories and amp up your exercise routine to lose weight if you need to. Talk to your doctor about losing weight in a way that's healthy for you, especially if you have other conditions like heart problems, asthma, arthritis, osteoporosis, or diabetes.[7]
- Being overweight puts pressure on your esophageal sphincter, which makes it easier for gastric acid to travel up your esophagus.
-
2Keep an upright posture during meals and for 2 hours after. Sit in a chair that allows you to have good posture—this means no slouching on the couch or laying sideways while you eat. Try going for a walk after eating to speed up the digestive process.[8]
- If you typically eat meals on the couch or in bed, put 2 or 3 pillows behind your back to keep you upright.
-
3Eat your last meal at least 3 hours before going to bed. Don’t eat right before you go to bed because the food will still be digesting, and laying down makes it easier for it to travel up your esophagus. If you go to bed around 11:00 PM, try to eat around 7:00 PM and no later than 8:00 PM (that includes dessert time!).[9]
- It’s okay to have a light bedtime snack, just keep it small and stick to something alkaline like a banana, sliver of avocado, or crackers with nut butter.
-
4Sleep with your head slightly elevated to decrease the risk of nighttime reflux. Use 2 pillows or insert cement or wood blocks to raise the head of your bed by 6–9 inches (15–23 cm). If you're a side sleeper, sleep on your left side so that your stomach is below the level of your esophagus.[10]
- You can also insert a padded wedge between your box spring and your mattress to lift it up.
- The idea is to keep your head just slightly above your stomach so it's harder for gastric acid to travel up your esophagus.
-
5Keep your seasonal allergies under control. Studies have shown that EoE symptoms tend to be worse during times when seasonal allergens are floating around from trees and grasses. Talk to your allergist about getting seasonal allergy shots to help your body get through the high-season with as little symptoms as possible.[11]
- Spring and fall tend to be the worst seasons for airborne allergies, but it varies depending on where you live.
- There's no evidence that seasonal allergies directly cause EoE, but studies have shown that half of the people diagnosed with EoE also suffer from seasonal allergies. It's worth dealing with those symptoms so you don't have to deal with a sneezing, a stuffy nose, and headaches while you're also dealing with EoE.
Did You Know?: If you live in a cold or dry climate, you're at a higher risk of being diagnosed with EoE, especially if you have acid reflux or GERD.[12]
-
6Stop smoking if you currently smoke. Quit cold turkey or use nicotine replacements (like gum, lozenges, or the patch) to wean yourself off slowly. Avoid places or situations in which you're tempted to smoke or come up with a game plan for riding out your cravings.[13]
- For example, you might carry a pack of flavored toothpicks in your pocket and chew on those when you're driving instead of smoking.
- While smoking doesn't directly make it more likely to get EoE, it can trigger acid reflux or GERD, which can lead to EoE.[14]
Assessing Possible Symptoms of EoE
-
1Pay attention if your acid reflux doesn't respond to treatment. If you experience acid reflux quite often and it doesn't go away after you take an antacid (over-the-counter or prescription), it could be GERD or EoE. Talk to your doctor about your persistent reflux and try to avoid your trigger foods as much as possible.[15]
- In most cases, your doctor will initially recommend proton pump inhibitors (PPIs) or antacids as a first treatment for acid reflux. They'll likely also recommend dietary changes and could give you topical glucocorticoids.
- GERD is chronic acid reflux while EoE is an inflammatory response that can be indirectly caused by the excessive stomach acid that eats away at the lining of your esophagus during GERD flare-ups.
-
2Take note of whether or not it's hard to swallow. If you're eating and find it hard or painful to swallow, that's something to talk to your doctor about. To help with this, try eating lots of soft or watery foods like potatoes, well-cooked veggies, and soup—they'll go down easier with less pain.[16]
- The inflammation caused by EoE makes it harder for your esophageal muscles to contract and carry the food down.
-
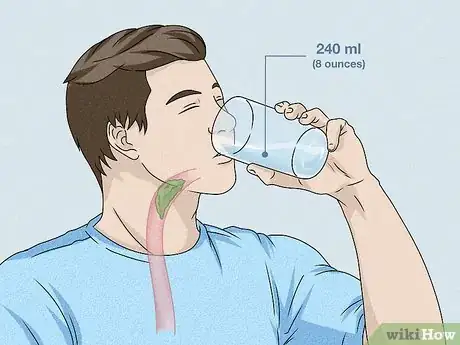
3Notice if food often gets stuck in your throat. Impaction is a telltale symptom of EoE, so you might have your doctor look into the situation if food gets stuck in your throat on a regular basis. To help push it down, try drinking 8 fluid ounces (240 mL) of water or taking a fizzy antacid like Alka-Seltzer.[17]
- You can also try drinking a can of soda—the carbonation can help break up bits of food and dislodge it from your throat.
- If food gets stuck in your throat often, your doctor may do a procedure to dilate your esophageal strictures during an endoscopy. While you're under a mild anesthesia, your doctor will insert a scope down your esophagus to widen areas that are narrow.[18] This can make it easier for you to swallow.
- It's easy for food to get stuck because there's less room for it to travel down your esophagus when the lining is swollen.
- If food gets stuck in your throat and you have trouble breathing or speaking, call for emergency medical care as soon as you can.
-
4Be aware of any unexpected weight loss. While it's not super common, EoE can cause a decrease in appetite. If you suspect you have EoE, weigh yourself once or twice a week to make sure you're maintaining your weight (unless, of course, if you're trying to lose weight). Losing 2–3 pounds (0.91–1.36 kg) without trying isn't much to worry about, but if you suddenly lose 10 pounds (4.5 kg) over the course of a few weeks, talk to your doctor about finding the cause.[19]
- Unexplained weight loss can be caused by a number of things (including other autoimmune disorders and thyroid conditions), so don't assume the loss is definitely due to EoE.
Getting a Diagnosis
-
1Have an upper endoscopy and biopsy to confirm the diagnosis. If your blood tests show higher counts of eosinophils, schedule a day with your gastroenterologist to have an upper endoscopy. It’s a super common procedure that only takes 30 to 45 minutes. You won’t feel a thing because you’ll be sedated. Of course, that means you’ll need to plan to have someone drive you home after the appointment.[20]
- If you're on blood thinners, stop taking them 3-4 days before your appointment.
- Don't eat or drink anything for 8 hours before your appointment unless your doctor says it’s okay to sip some water.
- During the procedure, your doctor will sedate you with a general anesthetic and then insert a long tube with a tiny camera on it down your throat. They'll be checking the walls of your esophagus for any swelling, white spots, horizontal rings, or vertical creases.
- If your doctor ordered a biopsy to confirm the suspicion of EoE, they'll use a small scraping tool to take a sample of tissue from your esophagus. They'll send it off to a lab to be tested for eosinophils and you'll have the results in 2 to 3 days.
- Most insurance plans cover the cost of both the endoscopy and biopsy.
-
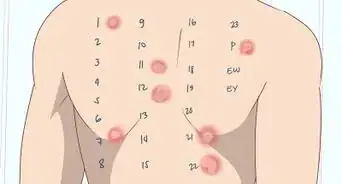
2Go to an allergist to get a skin prick allergy test. If you don't currently have an allergist or immunologist you go to, find one near you and schedule an appointment. Request to have a skin prick test done to see if you're allergic to any food or particular allergens in the air that may be causing or contributing to EoE or EoE-like symptoms.[21]
- The test involves pricking your skin with a tiny needle to introduce a certain allergen to your skin. If any swelling or redness shows up, that's a sign you're allergic to the particular allergen.
- The needles are dipped in extracts from foods that are common allergens to some people. These include milk, soy, wheat, eggs, peanuts, tree nuts (pecans, cashews, almonds, and walnuts), fish, and shellfish.
- Allergy skin prick tests are usually covered by all insurance plans. If you don't have insurance, it costs around $5 per allergen.
-
3Get a blood test to see if you're allergic to a particular allergen. Have your doctor take your blood and test it for higher-than-normal eosinophil counts. You can also have them test your blood for certain antibodies that might denote whether or not you’re allergic to gluten, dairy, nuts, or fish. The procedure is just like getting your blood drawn except it may take a little longer to get the results, especially if your doctor wants to test you for several types of allergies at once.[22]
- You may feel lightheaded after getting your blood taken, so be sure to bring a snack or something with sugar in it if you have to drive afterward. Some nurses will offer apple juice to help with the lightheadedness.
- If you have insurance, this blood test is most likely covered. However, you may end up paying for some of the tests if your doctor opts to test you for multiple allergies.
Warning: Skin prick tests are more sensitive than blood tests, so they're usually more accurate. In some cases, blood tests may show a false positive for a particular allergen.
Warnings
- If food gets stuck in your throat to the point where you’re having trouble breathing or speaking, call for emergency medical care right away.[24]⧼thumbs_response⧽
- EoE isn't life-threatening, but it is a chronic condition that, if left untreated, can cause damage to your esophagus.[25]⧼thumbs_response⧽
- Always talk to your doctor before starting any new diet or exercise regimen.⧼thumbs_response⧽
References
- ↑ https://www.aaaai.org/conditions-and-treatments/related-conditions/eosinophilic-esophagitis
- ↑ https://aboutgerd.org/diet-lifestyle-changes/7-day-food-and-symptom-diary.html
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/29238902
- ↑ https://www.hopkinsmedicine.org/health/wellness-and-prevention/gerd-diet-foods-that-help-with-acid-reflux-heartburn
- ↑ https://www.hopkinsmedicine.org/health/wellness-and-prevention/gerd-diet-foods-that-help-with-acid-reflux-heartburn
- ↑ https://www.ncbi.nlm.nih.gov/pubmed/29025076
- ↑ https://www.mayoclinic.org/diseases-conditions/eosinophilic-esophagitis/diagnosis-treatment/drc-20372203
- ↑ https://www.aboutgerd.org/diet-lifestyle-changes/diet-changes-for-gerd.html
- ↑ https://www.aboutgerd.org/diet-lifestyle-changes/diet-changes-for-gerd.html
- ↑ https://www.mayoclinic.org/diseases-conditions/eosinophilic-esophagitis/diagnosis-treatment/drc-20372203
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5135654/
- ↑ https://www.mayoclinic.org/diseases-conditions/eosinophilic-esophagitis/symptoms-causes/syc-20372197
- ↑ https://www.jacionline.org/article/S0091-6749(18)30627-4/pdf
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469260/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6469260/
- ↑ https://www.aaaai.org/conditions-and-treatments/related-conditions/eosinophilic-esophagitis
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4624046/
- ↑ https://www.winchesterhospital.org/health-library/article?id=645096
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3983983/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4591255/
- ↑ https://www.aaaai.org/conditions-and-treatments/related-conditions/eosinophilic-esophagitis
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4849505/
- ↑ https://www.aboutgerd.org/diet-lifestyle-changes/diet-changes-for-gerd.html
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096106/
- ↑ https://apfed.org/about-ead/egids/eoe/








































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...