This article was medically reviewed by Annette Lee, MD. Dr. Lee is a Reproductive Endocrinologist and Medical Director at RADfertility in Newark, Delaware. She has over 17 years of experience with IVF and is double board certified in Obstetrics & Gynecology. She has received Castle Connolly’s Regional Top Doctor Award for five years and Vitals.com Patient Choice Award for five years as well. She completed her medical degree at the Drexel University School of Medicine.
There are 19 references cited in this article, which can be found at the bottom of the page.
wikiHow marks an article as reader-approved once it receives enough positive feedback. This article received 19 testimonials and 95% of readers who voted found it helpful, earning it our reader-approved status.
This article has been viewed 204,863 times.
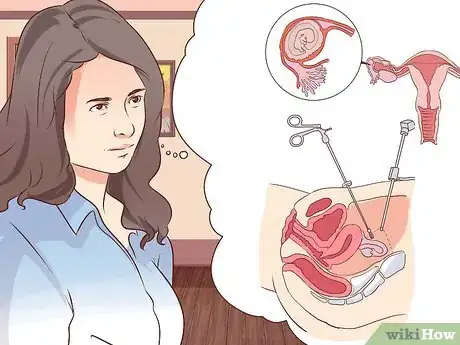
Experts say that in an ectopic pregnancy, the embryo (the fertilized egg) implants in a different area of the reproductive tract than the uterus. Although the most common location for an ectopic pregnancy is the fallopian tube, in rare instances, it might also implant in the ovary or abdomen. Research demonstrates that ectopic pregnancies are not viable-- meaning the embryo cannot develop into a healthy fetus -- and pose serious danger to the woman’s body, so they require prompt treatment.[1] While recovering from an ectopic pregnancy can be tough, you can use your resources to heal both physically and emotionally.[2]
Steps
Recovering Physically
-
1Understand your treatment options. How your doctor and you choose to treat the ectopic pregnancy will depend on your health, the location of the ectopic pregnancy, and the extent of existing damage to your reproductive organs.
- Some ectopic pregnancies are eliminated by the woman’s body. If your ectopic pregnancy is very early and you have no negative symptoms, your doctor may recommend “expectant management” or “active monitoring.” With this process, you wait for approximately a month, with frequent doctor supervision, to see whether your body can resolve the ectopic pregnancy without additional treatment. In general, this approach only makes sense when your hCG (a hormone produced during pregnancy) levels are low and declining, and when you have no symptoms.[3]
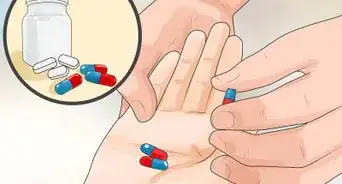
- If the ectopic pregnancy has been diagnosed very early and you do not have internal bleeding, your doctor may suggest an injection of methotrexate. Methotrexate will stop the growth of rapidly dividing cells, including pregnancy tissue (so it's important to rule out a normal pregnancy). It could take a couple of injections for this method to work completely.[4]
- A laparoscopic salpingostomy is a procedure that removes the pregnancy tissue without removing any portion of the tube. This treatment is generally appropriate for early ectopic pregnancies where the fallopian tube has not ruptured. Most surgical treatments of ectopic pregnancies use laparoscopy, which is done under general anesthesia and involves using a small tube with a camera and light inserted through a small incision.[5]
- A total salpingectomy may be necessary if the fallopian tube is very damaged, if you have very heavy bleeding, or in the case of a large ectopic pregnancy. In a total salpingectomy, the fallopian tube containing the ectopic pregnancy is removed.[6]
- A laparotomy is an abdominal surgery that is usually required in emergency cases of ruptured fallopian tubes or heavy bleeding. Laparotomies involve larger incisions and longer recovery times than laparoscopies.[7]
-
2Ask your doctor about the physical recovery process. Recovery time depends on the specific type of procedure that was used. In
- With laparoscopic surgeries, you will usually be able to go home the same day as surgery. Recovery is fairly quick, with most women being able to resume walking. You can usually resume your regular activities within 7 to 14 days. It can take about a month to fully recover from laparoscopy.[8]
- Surgeries done by laparotomy usually require several days in the hospital. This is because the incision is more extensive, and it will interfere with the functioning of your intestines. You will get clear liquids the morning after surgery and start solid foods within 24-36 hours. Laparotomy incisions may take up to 6 weeks to heal.
- While there may be little physical recovery necessary for early ectopic pregnancies that don't require surgery, your doctor will carefully monitor your health to ensure the ectopic pregnancy resolves on its own.
Advertisement -
3Avoid exercise or excessive physical activity. You may begin to feel better within a few days after your surgery. Do not push your body by exercising or doing too much physical activity. You also want to avoid any movements that may stretch or put strain on your incisions.[9]
- Do not lift anything that weighs more than 20 pounds for the first week.
- Climb stairs slowly, pausing after every few steps.
- Walk around whenever you feel able to. Do not try to jog or run.
-
4Expect constipation. Abdominal surgery can interfere with the functioning of your intestines and cause constipation. Your doctor will provide you with instructions on how to treat constipation. Some things you can do on your own include:[10]
- Eat high-fiber foods, such as fruits, vegetables, and whole grains.
- Drink plenty of water.
- Use laxatives or stool softeners (as recommended by your doctor).
-
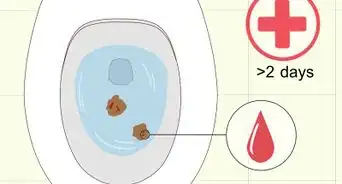
5Be prepared for regular hospital testing. If you had a salpingostomy or were treated by methotrexate injection, you will need to have regular tests to determine if the hCG levels in your blood return to zero. If they do not, you may need additional treatment with methotrexate.
-
6Expect some pain. There are many possible reasons why you would experience pain after an ectopic pregnancy. The incisions can take time to heal, and the resulting scar tissue may cause pain as well. If the pain becomes persistent, severe or unmanageable, contact your doctor.[11]
- Pain may also be due to your body trying to resume its normal menstrual cycle. Your body may resume its normal cycle between 4-6 weeks after treatment, although it could take longer.
- Some women report that they are more aware of ovulation following an ectopic pregnancy. They may experience pain when ovulating.[12]
-
7Recognize signs that you should seek medical help. Pain is usually your body’s way of telling you to rest. However, if you have any of the following symptoms along with pain, you should contact your doctor:[13] [14]
- Fever (above 100F or 38C)
- Vaginal discharge, especially if it smells “fishy” or ”funky”
- Lumps or bumps around the incision or scar that are red or hot to the touch
- Discharge from the incision site
- Nausea and/or vomiting
- Dizziness or fainting
-
8Discuss contraception with your doctor. After an ectopic pregnancy, you may not be able to use some contraception methods. You should discuss your options with your physician to determine what will work best for you.[15]
- IUDs and progesterone-only contraception are usually not recommended after an ectopic pregnancy.
- You should also speak with your doctor to determine when it is safe to have sexual intercourse again.The treatment you received will largely determine this.
-
9Wait to become pregnant again. If your ectopic pregnancy was treated with methotrexate, your doctor will advise you on how long you should wait before trying to become pregnant again. This is generally about one to three months, depending on the dosage you received. Methotrexate can cause problems for an early pregnancy by reducing the availability of folic acid to the fetus, so you need to wait until the drug is out of your system.
Recovering Emotionally
-
1Understand that your feelings are natural. An ectopic pregnancy is a physically and emotionally taxing experience. There are several reasons why you might feel angry, worried, or sad. You should know that these feelings are natural, and there is nothing “wrong” with you. There is no “right” or “wrong” way to feel.
- Your body’s hormonal balance has been in flux. This can lead to depressive symptoms. It can also cause symptoms such as palpitations, agitation, and dizziness.[16]
- Even though your body cannot carry an ectopic pregnancy to term, it can be devastating to learn that your pregnancy must be terminated.
- You may be worried about your health and your ability to have another pregnancy.
- You may blame yourself or feel guilty. You should know that ectopic pregnancies are not your fault.[17]
- Recovering from a major surgery can put further strain on your emotions.[18]
-
2Ask your doctor about counseling. Your hospital or community clinic may be able to refer you to counselors with special training in pregnancy-related issues. Losing a pregnancy and having major surgery are both experiences that you may find helpful to discuss with a mental health professional.[19]
- You may also wish to involve your partner in counseling. Some people may have difficulty expressing their feelings, and going to counseling together may help both of you work through this difficult time.[20] [21]
- It is a common myth that men do not grieve the loss of a pregnancy. However, research suggests this is not true. Men may express their grief differently than women, but they may also experience anger or depression after their partners lose a pregnancy.[22]
-
3Talk with friends or family. There is nothing that says you have to talk if you don’t want to. However, you may find that it helps to get support from those close to you. Find friends or family members that aren't afraid to acknowledge your loss and provide the support you need to work through this difficult time.[23]
-
4Find a support group. One of the most important elements that helps recovery is not feeling alone. You may find that a support group where you can talk with others who have had similar experiences will help you process your feelings.[24]
- In the United States, RESOLVE, the National Infertility Association, has support groups across the country. You can find a listing at their website.
- SHARE Pregnancy and Infant Loss Support also has local support groups in the US. You can find a support group in your area on their website.
- In the UK, the Ectopic Pregnancy Trust and the Miscarriage Association both offer resources and counseling for women who have lost pregnancies.[25]
- You may find that online support forums also provide a space for you to talk about your feelings. The Ectopic Pregnancy Trust maintains online forums overseen by medical professionals where you can discuss your experience and share your feelings.[26]
-
5Treat yourself with kindness. Some women find that doing something special for themselves helps them deal with the difficult days after an ectopic pregnancy. A trip to the spa or similar outing may alleviate the sadness and provide welcome pampering. You may just wish to sit on the couch and watch your favorite movies. Give yourself the love you need.[27]
- Do not feel guilty about treating yourself with kindness. Ectopic pregnancy can be physically and emotionally exhausting, and you need time to recover.
-
6Get exercise once it is safe to do so. Exercise after recovery is complete can be an effective way to minimize sadness and regain lost energy. Physical activity releases feel-good hormones called endorphins into the body, which are a natural mood-booster. Ask your doctor when you can begin an exercise regimen.[28]
- Do not do anything high-impact or vigorous without consulting with your doctor.
-
7Talk to your doctor before trying to get pregnant again after ectopic pregnancy. Your doctor will tell you when your body is physically ready and advise you about potential risk for another ectopic pregnancy. Some risk factors include smoking, endometriosis, pelvic inflammatory disease and a previous ectopic pregnancy. Those at risk will be closely monitored during a subsequent pregnancy, in order to catch potential problems and treat them early.[29]
- Consider seeing a reproductive endocrinologist, who is an ob/gyn with subspecialty training in fertility treatment. You will need evaluation of the fallopian tubes, for example, and this kind of doctor is the best person to provide that. You can find a board certified REI at www.srei.org.
Warnings
- Ectopic pregnancy can be a life-threatening medical condition. It cannot become a healthy fetus. You must get treatment.⧼thumbs_response⧽
- If you are pregnant and have abdominal pain, dizziness, faintness, diarrhea, or painful urination or bowel movements, seek medical help immediately.⧼thumbs_response⧽
References
- ↑ https://my.clevelandclinic.org/health/diseases/9687-ectopic-pregnancy
- ↑ https://www.nhs.uk/conditions/ectopic-pregnancy/treatment/
- ↑ http://www.nhs.uk/Conditions/Ectopic-pregnancy/Pages/Treatment.aspx
- ↑ https://www.acog.org/womens-health/faqs/ectopic-pregnancy
- ↑ https://jogcr.com/article-1-294-en.html
- ↑ https://emedicine.medscape.com/article/267384-overview
- ↑ https://pubmed.ncbi.nlm.nih.gov/23217480/
- ↑ http://www.nhs.uk/Conditions/Ectopic-pregnancy/Pages/Treatment.aspx
- ↑ http://www.uofmmedicalcenter.org/healthlibrary/Article/86330
- ↑ http://www.uofmmedicalcenter.org/healthlibrary/Article/86330
- ↑ http://www.ectopic.org.uk/patients/your-body-after-an-ectopic-pregnancy/
- ↑ http://www.ectopic.org.uk/patients/your-body-after-an-ectopic-pregnancy/
- ↑ http://www.ectopic.org.uk/patients/your-body-after-an-ectopic-pregnancy/
- ↑ http://www.uofmmedicalcenter.org/healthlibrary/Article/86330
- ↑ http://www.healthywa.wa.gov.au/Healthy-WA/Articles/A_E/Ectopic-pregnancy
- ↑ http://www.ectopic.org.uk/patients/emotional-impact/
- ↑ http://www.ectopic.org.uk/patients/emotional-impact/
- ↑ http://www.healthywa.wa.gov.au/Healthy-WA/Articles/A_E/Ectopic-pregnancy
- ↑ http://www.apa.org/monitor/2012/06/miscarriage.aspx
- ↑ http://www.healthywa.wa.gov.au/Healthy-WA/Articles/A_E/Ectopic-pregnancy
- ↑ http://americanpregnancy.org/pregnancy-loss/miscarriage-surviving-emotionally/
- ↑ http://www.apa.org/monitor/2012/06/miscarriage.aspx
- ↑ http://www.ectopic.org.uk/patients/emotional-impact/
- ↑ http://www.apa.org/monitor/2012/06/miscarriage.aspx
- ↑ http://www.ectopic.org.uk
- ↑ http://www.ectopic.org.uk/talk
- ↑ http://www.ectopic.org.uk/patients/emotional-impact/
- ↑ https://www.fairview.org/Patient-Education/Articles/English/a/f/t/e/r/After_Laparoscopic_Treatment_of_Ectopic_Pregnancy_86330
- ↑ https://my.clevelandclinic.org/health/diseases/9687-ectopic-pregnancy
- ↑ http://www.ectopic.org.uk/patients/your-body-after-an-ectopic-pregnancy/











































































Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...