This article was co-authored by Chris M. Matsko, MD. Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
This article has been viewed 59,483 times.
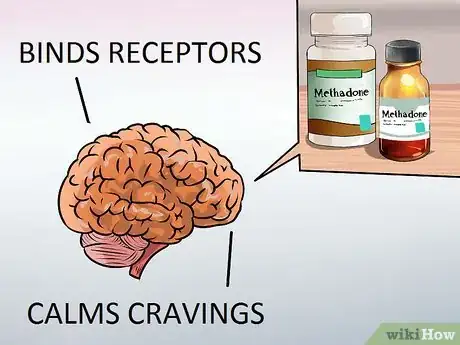
Methadone is a drug used as a pain reliever or to help detoxify and reduce withdrawal symptoms in people addicted to opiate drugs, such as heroin.[1] Methadone works by altering the way your brain and nervous system respond to pain, which results in pain relief from withdrawal. As a strong prescription drug, methadone should be taken exactly as directed by your doctor to avoid becoming addicted to it or experiencing other potentially harmful side effects.
Steps
Taking Methadone
-
1Consult with your doctor. If you are interested in taking methadone for opioid addiction, make an appointment with your doctor for an interview and physical exam. By law, methadone is only dispensed through an opioid treatment program (OTP) certified by the Substance Abuse and Mental Health Services Administration (SAMHSA) and supervised by a licensed physician.[2] As such, if you are accepted into the program, you need to see your doctor every 24 – 36 hours to get your appropriate dose.
- The length of time for methadone treatment varies, but it should be a minimum of 12 months.[3] Some patients require years of treatment.
- Methadone is given primarily by mouth through either tablets, powder or liquid.
- Single doses of methadone should not exceed 80 – 100 mg daily — its effectiveness can last between 12 – 36 hours depending on your age, weight, level of addiction and tolerance to the drug.
-
2Discuss the potential of taking methadone at home. After a period of stable progress and consistent compliance with the methadone dosage schedule, you may be given the drug in larger quantities to take home and administer it there to yourself.[4] You'll still need to see your doctor for progress visits and social support meetings, but you'll have more freedom away from the clinic. The decision is the doctor's and basically boils down to trust and a proven track record of compliance and desire to kick your addiction.
- Addiction clinics often disperse liquid methadone to patients, although tablets and powders that dissolve in water are typically given to patients for home use.
- Never share your specific allotment of methadone with anyone. It's illegal to give it out or sell it.
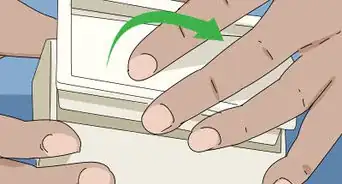
- Keep your methadone in a safe and secure place within your home, particularly out of reach of children.
- Methadone is not injected at clinics or for supervised home use, although sometimes illicit methadone is injected into the vein by street users.
Advertisement -
3Never alter your dosage. Methadone dosage is generally based on your body weight and opiate tolerance, but the specific dosage is calculated and altered over time based on your progress — which is measured by reduced opiate cravings. Once the dosage is established and then progressively lowered, it's crucial to follow the doctor's instruction exactly. Never take more methadone than recommended in hopes of it working better or quicker. If a methadone dose is missed or forgotten, or it doesn't feel like it's working, don't take an extra dose — resume your schedule and dose the following day.
- The tablets, sometimes called "diskettes," contain about 40 mg of methadone — which is a common dosage for people to take while administering at home.
- If you can't remember your doctor's instructions, then follow the directions on the prescription label carefully or ask the pharmacist to explain anything you don't understand.
-
4Learn how to take methadone at home. If you are given liquid methadone for home use, then carefully measure the medicine with a dosing syringe or with a special dose-measuring spoon or cup — you can get these from any pharmacist.[5] Don't mix the liquid with any additional water. If you have tablets or diskettes, drop them into at least four ounces (120 mL) of water or orange juice — the powder will not dissolve entirely. Drink the solution right away and then add a little more liquid to get the entire dose. Never chew the dry tablets or diskettes.
- You may be instructed to take only half of a tablet, so break it along the lines that are scored into it.
- Take your methadone at the same time every day, or according to your doctor's instructions.
- Set your watch, phone or alarm clock to remind yourself of the dosing time.
-
5Avoid methadone if you have risk factors. You shouldn't use methadone if you are allergic to it or if you have asthma, severe breathing problems, heart rhythm disorder, heart disease or bowel obstruction (paralytic ileus).[6] Any of these conditions are likely to increase the risk of experiencing negative reactions to methadone.
- Patients should share their complete medical/drug history with healthcare providers to ensure the safe use of methadone.
- Your doctor will normally decrease your dosage or tell you to take less methadone as your treatment progresses, but they might increase the dose if you experience any unforeseen withdrawal pain.
Understanding the Uses of Methadone
-
1Learn what methadone is commonly prescribed for. Methadone was first made in the 1930s in Germany because doctors were attempting to produce a pain-killing drug (analgesic) created with readily available precursors. That way Germany's opium shortage would be solved. By the early 1970s, methadone was used less as a painkiller and more for helping people reduce or quit their addiction to opiates, including morphine and heroin. Methadone is now the top choice for opiate addiction and widely used in comprehensive medication-assisted treatment (MAT) programs that also include counseling and social support.[7]
- If you're dealing with significant chronic pain and want a painkiller to take long-term, methadone is likely not the answer due to its numerous side effects.
- When taken as prescribed and over the short term, methadone is relatively safe and effective for helping people recover from their narcotic addictions.
-
2Understand how methadone works. Methadone works as an analgesic by changing how your brain and nervous system respond to pain signals/sensations.[8] So while it can lessen the painful symptoms of heroin withdrawal, it also blocks the euphoric effects of opiates — essentially stopping the pain without triggering the sensation of being "high." As such, an addict uses methadone while taking less opiates until there is no withdrawal pain. Then, the addict is weaned off of methadone.
- Methadone is available as pills, liquids and wafer forms. It's meant to be taken once daily and the pain relief lasts between four and eight hours depending on dosage.
- Opiate drugs include heroin, morphine and codeine, whereas as semi-synthetic opioids include oxycodone and hydrocodone.
-
3Be aware of unwanted side effects. Although methadone is considered a relatively safe medication, side effects are not uncommon. The most common side effects triggered by methadone use include dizziness, drowsiness, nausea, vomiting and/or increased sweating.[9] The more serious, albeit less common, side effects include labored or shallow breathing, chest pain, racing heartbeat, hives, severe constipation and/or hallucinations/confusion.[10]
- Although methadone is intended to prevent opiate addiction, dependence and painful withdrawal symptoms, there's still potential for getting addicted to methadone.
- Perhaps ironically, methadone is abused as an illicit street drug, although it's ability to get people "high" (euphoric) is not nearly as strong as opiates.
- Women who are pregnant or breastfeeding can take methadone for addiction (it won't cause birth defects) and it lowers the risk of miscarriage.
-
4Consider the alternatives. Aside from methadone, there are a few other options for the treatment of opioid dependence: buprenorphine and L-alpha-acetyl-methadol (LAAM). Buprenorphine (Buprenex) is a very strong semi-synthetic narcotic recently approved to help treat heroin addiction. Compared to methadone, it causes far less respiratory problems and is thought to be more difficult to overdose. LAAM is a good alternative to methadone because it has longer lasting effects — instead of daily treatments, addicts only take the drug three times weekly. LAAM is similar to methadone in that it doesn't get the user "high", but it's considered a little safer in terms of side effects.
- Buprenorphine doesn't lead to significant physical dependence or discomforting withdrawal symptoms, so getting off it is typically much easier compared to methadone.
- LAAM can trigger anxiety in users and it can lead to liver dysfunction, hypertension, skin rashes and nausea.
Expert Q&A
-
QuestionHow long does methadone stay in your system?
 Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Chris M. Matsko, MDDr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017.
Family Medicine Physician The half life elimination of methadone is 35 hours +/- 22 hours; therefore, the range is nine to 87 hours. This can be prolonged if the patient has and alkaline pH.
The half life elimination of methadone is 35 hours +/- 22 hours; therefore, the range is nine to 87 hours. This can be prolonged if the patient has and alkaline pH.
Warnings
- Do not combine alcohol with methadone, as it can cause severe complications and lead to sudden death.⧼thumbs_response⧽
- Methadone may impair your ability to think and/or react, so void driving your car or operating machinery while taking it.⧼thumbs_response⧽
References
- ↑ https://www.nlm.nih.gov/medlineplus/druginfo/meds/a682134.html
- ↑ http://www.samhsa.gov/medication-assisted-treatment/treatment/methadone
- ↑ http://www.samhsa.gov/medication-assisted-treatment/treatment/methadone
- ↑ http://www.samhsa.gov/medication-assisted-treatment/treatment/methadone
- ↑ https://www.drugs.com/methadone.html
- ↑ https://www.drugs.com/methadone.html
- ↑ http://www.samhsa.gov/medication-assisted-treatment/treatment/methadone
- ↑ http://www.samhsa.gov/medication-assisted-treatment/treatment/methadone
- ↑ https://www.drugs.com/methadone.html